Last Updated on November 26, 2025 by Bilal Hasdemir
Proper care of a bile duct drainage bag is key to safe recovery after biliary procedures. At Liv Hospital, we know how vital effective biliary drainage management is. This is true for patients who have had procedures with a bile catheter or biliary duct drainage catheter.
Managing biliary drainage can be tough, but with the right help, it’s easier. A bile duct drainage bag is a vital tool. It helps collect bile safely and prevents problems.
Our guide will cover the basics of biliary drainage. We’ll look at the various drainage bags and how to use them well. We want to give patients and healthcare workers the knowledge they need for safe recovery.
Key Takeaways
- Understanding the role of a bile duct drainage bag in biliary drainage management
- Importance of proper care and maintenance of biliary drainage systems
- Types of biliary drainage bags and their applications
- Effective management strategies for biliary drainage
- Preventing complications associated with biliary drainage
The Biliary System and Drainage Fundamentals
Understanding the biliary system is key to managing drainage. It includes the liver, gallbladder, and bile ducts. These parts work together to move bile from the liver to the small intestine, aiding digestion.
Anatomy of the Biliary System
The biliary system’s structure is quite complex. It has intrahepatic and extrahepatic bile ducts. The liver makes bile, which is stored in the gallbladder. It then flows into the small intestine through the common bile duct.
Knowing the biliary tree’s layout is critical. This includes the right and left hepatic ducts joining to form the common hepatic duct. This knowledge is essential for managing bile duct drainage.
| Component | Function |
| Liver | Produces bile |
| Gallbladder | Stores bile |
| Bile Ducts | Transports bile to the small intestine |
Conditions Requiring Bile Duct Drainage
Some conditions block bile flow, requiring drainage. These include malignant strictures, gallstones, and bile leaks after surgery. Draining the bile ducts helps restore normal flow, easing symptoms and preventing further issues.
“Biliary drainage is a lifesaving procedure for patients with obstructive jaundice due to malignant biliary strictures.” – Medical Expert, Interventional Radiologist.
.Benefits of Controlled Bile Collection
Collecting bile in a controlled manner has many benefits. It relieves jaundice, reduces itching, and prevents infections. Proper bile flow improves liver function and overall health.
Key benefits include:
- Relief of jaundice and pruritus
- Prevention of cholangitis
- Improved liver function
Understanding the biliary system and conditions needing drainage helps healthcare providers. They can then offer better management, improving patient outcomes.
Types of Bile Duct Drainage Bags
There are many bile duct drainage bags to choose from. Each one is made for different needs and situations. They help manage bile drainage in various ways.
External Drainage Collection Systems
External drainage systems are for patients who need to collect bile outside their bodies. They are key for managing bile in certain conditions or after surgery.
- Design and Functionality: These systems aim to be both efficient and comfortable. They have features to prevent leaks and bad smells.
- Clinical Use: They are used in many settings, like after surgery or for biliary obstruction.
Internal-External Biliary Drainage Bags
Internal-external biliary drainage bags do two things at once. They allow for both internal and external bile drainage. This is very helpful in complex cases.
Key Features:
- They let bile drain internally, reducing the chance of leaks.
- They also let you collect bile externally, helping with patient care.
Liver Drainage Bags for Hepatic Procedures
Liver drainage bags are made for liver surgeries and treatments. They meet the special needs of these procedures.
These bags are designed to:
- Effectively manage bile during and after liver procedures.
- Reduce the risks of bile leaks.
Knowing about the different bile duct drainage bags helps healthcare providers give better care. They can tailor treatment to each patient’s needs.
Bile Catheter Systems and Components
It’s important to know about bile catheter systems to manage biliary drainage well. These systems help drain bile from the liver or bile ducts. They are key for patients with biliary blockages or other issues needing biliary decompression.
Biliary Duct Drainage Catheters
Biliary duct drainage catheters are a vital part of bile catheter systems. They are put into the bile ducts to help with drainage. There are different sizes and types, like pigtail catheters, which are often used because they stay in place well.
These catheters are made from materials that don’t react with bile. Their size and number of holes are set to ensure good drainage without clogging.
Biliary tubes and Connection Systems link the catheter to a collection bag or other drainage tools. They are made to be flexible and not kink, so drainage keeps flowing. The connection systems, like Luer locks, keep the catheter attached to the bag, stopping it from coming loose.
The design of these tubes and connections is key to keeping the system clean and preventing problems like infections or bile leaks.
Materials and Design Considerations
The materials in bile catheter systems are chosen for their safety, strength, and ability to resist bile’s corrosive effects. Polyurethane and other polymers are often used because they work well.
When designing these systems, factors like the catheter’s size, length, and hole placement are important. The tip design is also critical, as it needs to be easy to insert without harming the bile duct.
We know that the success of bile catheter systems depends on their design, materials, and how they are used in patient care. Understanding these systems helps healthcare providers improve patient outcomes and quality of life.
Percutaneous Biliary Drainage Procedures
Biliary obstruction management has seen big improvements with percutaneous drainage techniques. This method is a minimally invasive way to relieve bile duct blockages. We will look at when this procedure is used, who it’s for, and how often it works. We’ll also cover the steps of the procedure and the importance of imaging guidance.
Indications and Patient Selection
Percutaneous biliary drainage helps patients with bile duct blockages. This can be due to cancer, benign strictures, or post-surgery issues. Choosing the right patient involves checking the blockage’s cause and the patient’s health. Patients with bleeding problems or fluid buildup in the belly need extra care before the procedure.
Doctors decide on this procedure after looking at imaging tests like ultrasound, CT, or MRI. These tests show where and why the blockage is happening. This helps the radiologist plan the best approach.
Technical Success Rates in Contemporary Research
Recent studies show high success rates for this procedure. Research shows it works in over 90% of cases, greatly improving symptoms and quality of life. Success rates can change based on the blockage’s cause and the patient’s health.
| Cause of Obstruction | Technical Success Rate (%) | Clinical Improvement (%) |
| Malignant Obstruction | 92 | 85 |
| Benign Stricture | 95 | 90 |
| Postoperative Complications | 88 | 80 |
Procedure Steps and Imaging Guidance
The procedure starts with accessing the bile ducts under imaging. Ultrasound and fluoroscopy guide the needle and catheter placement. A catheter is then placed to drain the bile, easing pressure and jaundice.
Imaging guidance is key to the procedure’s success, reducing risks. Afterward, the catheter’s function and the patient’s health are closely monitored. Adjustments are made as needed to ensure proper drainage.
Understanding percutaneous biliary drainage helps healthcare providers manage biliary obstructions better. This improves patient outcomes and quality of life.
Internal-External Biliary Drainage for Malignant Obstruction
Internal-external biliary drainage is a key treatment for malignant biliary obstruction. It helps patients with malignant biliary strictures. This improves their quality of life by relieving symptoms.
Management of Malignant Biliary Strictures
Malignant biliary strictures are common in cancer patients, often seen in pancreatic or bile duct tumors. Internal-external biliary drains are used to manage these strictures. They ensure bile flows properly, reducing symptoms like jaundice and pruritus.
This method creates a pathway for bile to flow out of the liver. It’s done percutaneously, giving immediate relief from symptoms.
Effects on Pruritus and Quality of Life
Internal-external biliary drainage greatly reduces pruritus, a severe symptom of biliary obstruction. It improves patient comfort and quality of life by restoring normal bile flow.
Studies show a significant decrease in pruritus and an improvement in well-being after this procedure. Quality of life assessments highlight their.
Long-term Outcomes and Considerations
Long-term outcomes of internal-external biliary drainage are important. While it offers many benefits, there are risks like catheter occlusion or infection. These need to be managed.
The table below summarizes long-term outcomes for patients with malignant obstruction:
| Outcome | Description | Management Strategy |
| Catheter Patency | Maintaining catheter patency is key to effective aging. | Regular flushing and monitoring. |
| Infection Prevention | Preventing infection is vital to avoid complications. | Prophylactic antibiotics and sterile technique. |
| Quality of Life | Improving and maintaining quality of life is a main goal. | Palliative care and symptom management. |
Understanding these aspects helps healthcare providers manage patient expectations and outcomes. This ensures internal-external biliary drainage is used effectively for malignant biliary obstruction.
Using Your Bile Duct Drainage Bag: Patient Guide
Learning how to use and care for your bile duct drainage bag can greatly improve your life. It’s important to manage it well to stay comfortable and avoid problems.
Daily Care and Maintenance Routine
To keep your bile duct drainage bag working right, follow a daily routine. This includes:
- Cleaning the skin around the catheter site with mild soap and water
- Drying the area well to stop infection
- Checking the catheter and drainage bag for damage or leaks
Regular inspection of the drainage bag and its connections is keyto tocatchingh problems early.
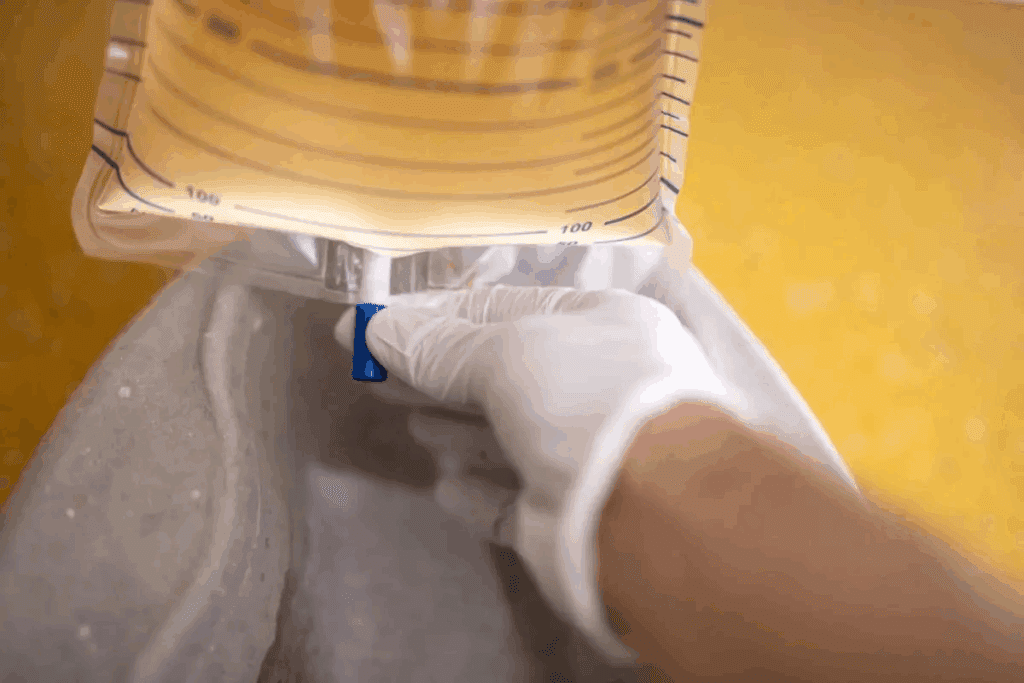
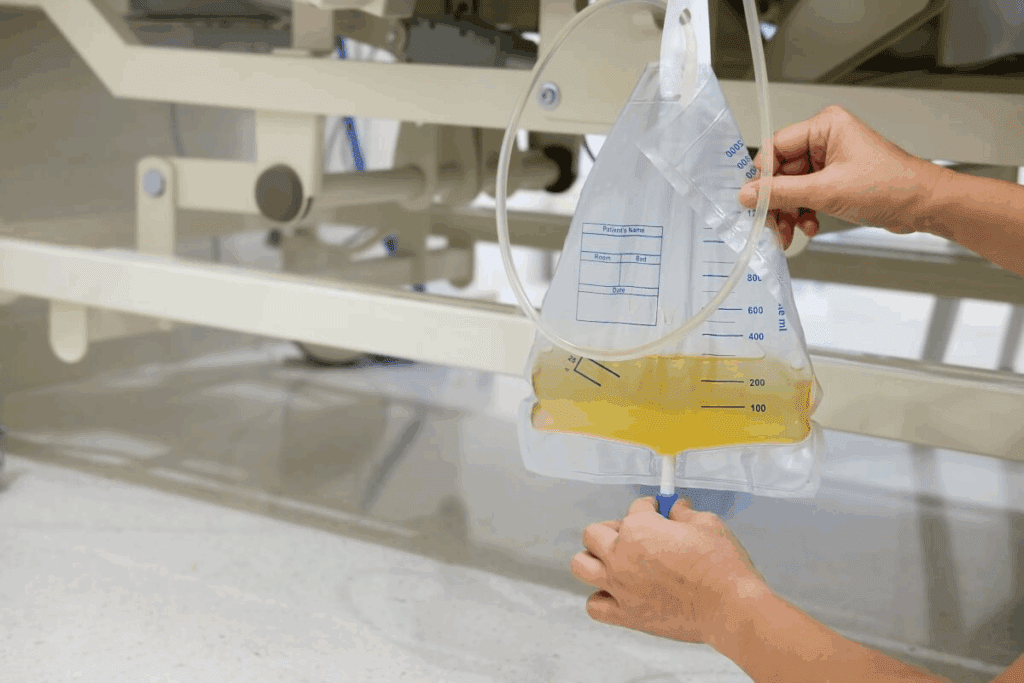
Emptying and Measuring Drainage Output
It’s important to empty your bile duct drainage bag often to avoid overflow. To do this:
- Wash your hands well before touching the drainage bag
- Open the drainage valve and empty the contents into a measuring container
- Record how much drainage you have
- Close the valve tightly after emptying
Accurate measurement of drainage helps your doctor keep track of your health and adjust your treatment as needed.
Troubleshooting Common Issues
Occasionally, you might run into problems with your bile duct drainage bag. Common issues include:
- Blockages or kinking of the catheter
- Leakage from the drainage bag or connections
- Infection signs like redness, swelling, or fever
If you face any of these problems, reach out to your healthcare provider for help. Often, simple changes can fix the issue.
“Proper care and maintenance of your bile duct drainage bag are key to successful biliary drainage management.”
Monitoring Biliary Drainage Color and Output
Watching the color and amount of biliary drainage is key. It shows if a patient is getting better or facing problems.
Normal vs. Abnormal Drainage Characteristics
Bile’s color and texture can change based on the patient’s health. Normally, it’s golden yellow to dark green. But, if it’s:
- Clay-colored or pale, it might mean a blockage or lack of bile salts.
- Dark or bloody, it could be a sign of bleeding or serious issues.
- Full of debris, it might show an infection or other problems.
Cholecystectomy Drainage Color Assessment
After a cholecystectomy, bile color can tell a lot about recovery. It’s usually green to yellow. But if the color changes, it might mean a complication.
| Drainage Color | Possible Indication |
| Green to Yellow | Normal bilious drainage |
| Clay-colored or Pale | Possible blockage or absence of bile salts |
| Bloody or Dark | Bleeding or serious complication |
Quantification Methods for Liver Drainage
Measuring liver drainage is vital for checking on a patient’s health. It helps see if the treatment is working. Ways to measure include:
- Regularly checking how much drainage there is.
- Looking for blood or other odd things in the drainage.
- Using images to see how the biliary system is doing.
Getting accurate measurements helps doctors make better decisions for their patients.
Preventing Complications with Proper Management
To avoid problems, managing biliary drainage well is key. Taking care of the bile duct drainage bag and catheters is important. It helps lower the chance of issues and makes biliary drainage work better.
Infection Prevention Protocols
Stopping infections is a big deal in biliary drainage care. We suggest strict cleanliness when dealing with the drainage bag or catheter. This means washing hands well before and after touching the system. Also, cleaning and disinfecting the catheter exit site often is a must. Using sterile tools and following aseptic methods for dressing changes can greatly cut down infection risk.
We also tell patients to watch their temperature closely. If they feel feverish or have chills, they should tell their doctor right away. Catching infections early can help treat them quickly and avoid bigger problems.
Strategies to Avoid Bile Leakage
Bile leakage is a problem that can be lessened with good management. Making sure the catheter and drainage bag are securely connected is key. We suggest checking these connections often for any signs of leaks or damage. Using a drainage bag with anti-reflux valves can also help stop bile from flowing back into the catheter, lowering leakage risk.
Patients should also be careful when moving or changing positions. This helps avoid putting too much stress on the catheter or drainage bag. Such stress can cause dislodgment or leakage.
Maintaining Catheter Patency
Keeping the biliary catheter open is critical for ongoing drainage. We advise regular flushing of the catheter as a healthcare professional tells you to. This removes any blockages caused by debris or sediment. It’s also key to watch the drainage output and tell a healthcare provider if there are big changes or if drainage stops.
Regular check-ups with a healthcare provider are important. They help ensure the catheter is in the right place and working properly. This way, any problems can be caught early and fixed quickly.
Post-Procedural Care for Different Biliary Interventions
The care needed after biliary procedures changes a lot based on the type of procedure. It’s important to know these differences. This helps in giving the right care and making sure patients do well.
Care After Cholecystectomy with Drainage
Patients need close watch after a cholecystectomy with drainage to avoid problems. We suggest:
- Regular dressing changes to keep the wound clean
- Watching the drainage for volume and what it looks like
- Telling patients about the signs of possible issues
Key Considerations: It’s vital to remind patients about the need for follow-up. This is to check if the drain can be removed and to watch for any late problems.
Management Following Percutaneous Transhepatic Cholangiography
PTC needs special care to lower risks. We focus on:
- Watching the puncture site for bleeding or infection
- Looking out for complications like bile leakage
- Teaching patients about post-procedure care and follow-up
Recovery from Internal-External Biliary Drain Placement
Internal-external biliary drain placement needs a detailed care plan. Important parts include:
| Care Aspect | Description |
| Drain Maintenance | Regular flushing and checking for kinking or blockage |
| Output Monitoring | Tracking volume, color, and consistency of drainage |
| Patient Education | Instructions on drain care, signs of complications, and follow-up |
Good care after biliary procedures is key to avoiding problems and getting the best results. By customizing care for each procedure, healthcare teams can greatly help patients recover and improve their quality.
Conclusion
Effective biliary drainage management is key to good patient outcomes. We’ve looked at what makes this process complex. The type of bile duct drainage bag, patient care, and post-procedure management are all important.
Patients and healthcare providers can work together for the best results. We’ve seen how different bags help manage biliary conditions. This includes external and internal-external bags.
Good patient care is critical. It includes daily routines, watching the drainage, and solving common problems. A complete approach to care is essential for the best results.
FAQ
What is a bile duct drainage bag used for?
A bile duct drainage bag collects bile after certain procedures. It helps prevent problems and ensures bile flows properly.
How do I care for my bile duct drainage bag?
To care for your bag, clean it daily and watch for leaks or damage. Empty and measure the bag regularly.
What are the different types of bile duct drainage bags available?
There are many types of bags, like external and internal-external systems. Each is for different needs and procedures.
How do I monitor the color and output of my biliary drainage?
Watch the drainage color and amount. Know what’s normal and what’s not. Use methods to measure liver drainage.
What are the signs of complications with biliary drainage, and how can they be prevented?
Complications include infection and blockages. Prevent them with good infection control and by keeping the catheter open.
What is internal-external biliary drainage used for?
It’s for managing blockages in the bile ducts. It helps patients feel better and live better.
How is internal-external biliary drainage performed?
This procedure is done by inserting a catheter. It’s guided by images to ensure it works right.
What is the role of a biliary catheter in biliary drainage management?
A biliary catheter is key for draining bile. Keeping it clean is vital to avoid problems.
How do I manage my biliary drainage after cholecystectomy?
After cholecystectomy, watch the drainage closely. Follow care instructions to avoid issues.
What are the long-term considerations for patients with internal-external biliary drainage?
Patients need regular check-ups and to keep the catheter open. Managing symptoms is also important for a good life.
References
- Popat, B. (2016). Percutaneous transhepatic biliary drainage in the management of bile duct injuries and leaks. World Journal of Gastrointestinal Surgery, 8(1), 20-27. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC5346079/





