
Being referred to a hepatobiliary specialist means you have complex issues with your liver, gallbladder, or pancreas. These problems need special care. Issues like bile duct obstruction or obstructive biliary disease are hard to diagnose and treat. That’s why you need an expert’s help.
Liv Hospital’s Hepatobiliary Clinic uses a team approach. They follow the latest care pathways and protocols. This ensures patients get the right treatment for their liver or biliary disease.
Key Takeaways
- A hepatobiliary specialist is key for complex liver, gallbladder, or pancreatic diseases.
- Conditions like bile duct obstruction need special care.
- Liv Hospital uses a team approach for thorough patient evaluation.
- They use the latest protocols for treating biliary diseases.
- Specialized care helps improve treatment results for liver disorders.
Understanding the Hepatobiliary System
To grasp the complexities of hepatobiliary referrals, we must first understand the system’s anatomy and function. The hepatobiliary system, which includes the liver, gallbladder, and pancreas, is key to our digestive health.
Anatomy and Function of the Liver, Gallbladder, and Pancreas
The liver is our largest internal organ. It detoxifies, makes proteins, and produces biochemicals for digestion. The gallbladder holds bile, a fluid from the liver that helps digest fats. The pancreas makes digestive enzymes and hormones like insulin, which controls blood sugar.
The liver does many things, like metabolizing nutrients and detoxifying harmful substances. It also makes bile. The gallbladder concentrates and stores bile, releasing it into the small intestine for fat digestion. The pancreas produces digestive enzymes and hormones.
The Role of Bile Ducts in Digestive Health
Bile ducts are vital for digestive health. They carry bile from the liver and gallbladder to the small intestine. Bile duct obstruction can cause severe health problems, like jaundice, itching, and digestive issues. Symptoms of bile duct obstruction or liver duct obstruction include jaundice, abdominal pain, and changes in stool or urine color.
- Bile ducts are essential for transporting bile to the small intestine.
- Obstruction of bile ducts can lead to serious health issues.
- Symptoms of biliary obstruction include jaundice and abdominal pain.
Knowing the hepatobiliary system’s anatomy and function is key to diagnosing and treating related disorders. Conditions like biliary obstruction show how important a well-working hepatobiliary system is.
Common Reasons for Hepatobiliary Referrals
The hepatobiliary system includes the liver, gallbladder, and bile ducts. It can face several issues that need a specialist’s help. These problems show up in different ways and need a hepatologist’s skills to diagnose.
Liver Disease Indicators
Liver disease is a big reason for needing a hepatologist. High liver function tests often mean there’s a problem. This can be due to hepatitis, fatty liver, or cirrhosis.
Abnormal liver function tests can come from many sources. This includes viruses, too much alcohol, and metabolic issues. A hepatologist must figure out the cause and how to treat it.
Gallbladder and Pancreatic Concerns
Gallbladder and pancreatic issues are also common reasons for seeing a hepatologist. Problems like gallstones, cholecystitis, and pancreatitis can be serious. They often cause pain, jaundice, and digestive problems.
A blocked bile duct or blocked gallbladder duct can cause jaundice. This is when your skin and eyes turn yellow. It also makes your urine dark and your stools pale. This needs quick attention to avoid worse problems.
Unexplained Abdominal Pain and Digestive Issues
Unexplained pain and digestive problems are also reasons to see a hepatologist. Issues like irritable bowel syndrome and functional dyspepsia can be hard to figure out and treat.
To find out what’s causing the symptoms, tests and procedures might be needed. A hepatologist can help manage these complex issues.
Bile Duct Obstruction: A Primary Cause for Specialist Referral
Bile duct blockage is a main reason for seeing a specialist. It happens when bile can’t flow right because of a block. This can cause jaundice, infection, and harm to the liver.
Defining Obstructive Biliary Disease
Obstructive biliary disease means bile can’t flow because of a block. This block can be from gallstones, tumors, or inflammation. It stops bile from reaching the intestine, causing jaundice and other symptoms.
“The obstruction of bile ducts is a serious condition that requires prompt medical attention to prevent long-term liver damage.” Doctors say quick diagnosis and treatment are key to managing this disease and avoiding serious problems.
Common Causes of Bile Duct Blockage
Several things can cause bile duct blockage, including:
- Gallstones that move into the bile ducts
- Tumors, both benign and malignant, that block the bile ducts
- Inflammatory diseases, such as primary sclerosing cholangitis
- External compression by nearby masses or lymph nodes
These can cause partial or complete blockage of the bile ducts.
Risk Factors and Progression of Biliary Obstruction
Some factors increase the chance of bile duct obstruction. These include gallstones, past biliary surgery, and conditions like primary sclerosing cholangitis. The blockage can lead to infections and scarring of the liver.
The risk of complications shows why early diagnosis and treatment are so important. Doctors use imaging and other tests to find the cause and extent of the blockage.
In summary, bile duct obstruction is a serious issue that needs specialist care. Knowing its causes, risks, and complications is key to managing and treating it effectively.
Key Symptoms That Prompt Hepatobiliary Referrals
Knowing the symptoms is key to knowing when to see a hepatobiliary specialist. The liver, gallbladder, and bile ducts are vital for digestion and health. When they’re not working right, certain symptoms show up, signaling the need for expert care.
Jaundice and Skin Changes
Jaundice, a yellow skin and eye condition, is a clear sign of liver or bile duct trouble. Obstructive jaundice happens when the bile duct is blocked. It makes it hard for bilirubin to leave the body. Itching (pruritus) can also occur, making life harder for those affected.
Digestive Symptoms and Abdominal Pain
People with liver or bile duct issues often have digestive problems. These include:
- Nausea and vomiting
- Changes in stool color or consistency
- Abdominal pain, mainly in the right upper quadrant
- Bloating and discomfort after eating
Abdominal pain is a big warning sign of liver or bile duct disease. It can be caused by inflammation, blockages, or other issues.
Systemic Symptoms of Hepatobiliary Disorders
Hepatobiliary disorders can also cause symptoms that affect the whole body. These include:
- Fatigue and general malaise
- Weight loss
- Fever, in cases of infection or inflammation
These symptoms might not be specific but, along with jaundice or pain, they can mean it’s time to see a specialist.
Spotting these symptoms early is vital. It helps ensure patients get the right care for their health issues.
Diagnostic Tests Leading to Specialist Referrals
Healthcare providers use many tests to find out about liver and gallbladder diseases. These tests check the liver, gallbladder, and pancreas. They help find problems that need a specialist.
Blood Tests and Liver Function Markers
Blood tests are key to checking liver health. They look at enzymes and proteins like ALT and AST. These show if the liver is damaged.
Liver function tests also check if the liver works right. This includes detoxifying and making proteins.
Imaging Studies for Hepatobiliary Assessment
Imaging studies are very important for diagnosing liver and gallbladder problems. Ultrasound, CT scans, and MRI give clear pictures of these organs. They help find issues like gallstones or tumors.
An ultrasound can spot gallstones or bile duct problems. A CT scan shows how much damage there is or if there are tumors. MRI cholangiopancreatography (MRCP) is great for seeing the bile and pancreatic ducts well.
Specialized Diagnostic Procedures
Some tests are needed for specific liver and gallbladder problems. ERCP lets doctors look at bile and pancreatic ducts. It can also remove gallstones or take tissue samples.
Percutaneous transhepatic cholangiography (PTC) involves putting contrast material into the bile ducts. It helps find blockages or other issues. These procedures are key for diagnosing and sometimes treating these problems.
Liver Conditions Requiring Specialist Care
The liver can get sick with cirrhosis, hepatitis, and liver cancer. These problems hurt the liver’s function and health. They need quick and expert care.
Cirrhosis and Advanced Liver Disease
Cirrhosis is when the liver gets scarred from diseases like hepatitis and too much alcohol. This scarring can’t be undone, so finding and treating it early is key.
Key aspects of cirrhosis include:
- Liver damage that is not reversible
- Potential for complications such as portal hypertension
- Need for lifestyle changes and medical management
Hepatitis (Viral, Autoimmune, and Other Forms)
Hepatitis means the liver is inflamed, often from viruses. But toxins and autoimmune diseases can also cause it. Each type affects the liver differently.
|
Type of Hepatitis |
Causes |
Implications |
|---|---|---|
|
Viral Hepatitis |
Hepatitis A, B, C viruses |
Can lead to acute or chronic infection |
|
Autoimmune Hepatitis |
Immune system attacking liver cells |
Can lead to cirrhosis if not treated |
Liver Tumors and Cancer
Liver cancer starts in the liver. It can be primary or spread from another part of the body.
Risk factors for liver cancer include:
- Chronic infection with hepatitis B or C
- Cirrhosis
- Heavy alcohol consumption
Spotting liver cancer early and treating it quickly can help people live longer. Getting help from specialists is very important.
Gallbladder and Biliary Tract Disorders
Gallbladder and biliary tract disorders include many conditions that need quick diagnosis and treatment. These issues can greatly affect a person’s life quality. They can also lead to serious problems if not handled correctly.
Complicated Gallstone Disease
Complicated gallstone disease is a big worry in gallbladder issues. Gallstones can block bile ducts, causing pain, jaundice, and serious infections. Many people with gallstones don’t show symptoms, but when they do, it’s severe. Risk factors include being overweight, certain diets, and family history.
Quick action is key to avoid serious problems like cholecystitis or pancreatitis. Doctors use ultrasound to find gallstones and see how they affect the biliary system.
Cholecystitis and Cholangitis
Cholecystitis is inflammation of the gallbladder, often caused by a blocked cystic duct. It can be acute or chronic and may need urgent surgery. Cholangitis is an infection of the bile ducts that’s very dangerous if not treated fast with antibiotics and sometimes drainage.
“Early recognition and treatment of cholecystitis and cholangitis are critical to preventing serious complications and improving patient outcomes.”
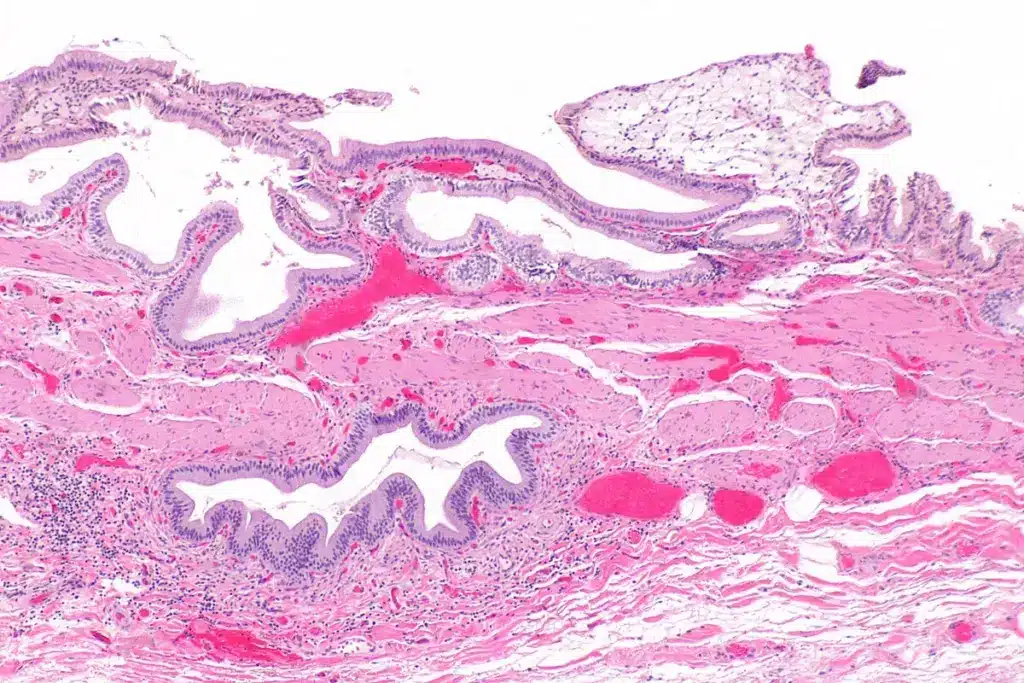
Biliary Tract Tumors
Biliary tract tumors, like cholangiocarcinoma, are rare but aggressive. They can happen anywhere in the biliary tree and often cause jaundice and weight loss. Diagnosis involves imaging studies and biopsy. Treatment depends on the tumor’s location and stage, from surgery to palliative care.
Managing gallbladder and biliary tract disorders needs a team effort from gastroenterologists, surgeons, and oncologists. Knowing the causes and risk factors is vital for good management and better patient results.
Pancreatic Conditions Warranting Referral
Pancreatic diseases, like pancreatitis and pancreatic cancer, need a specialist’s care. The pancreas is key for digestion and metabolism. Problems here can seriously affect health.
Acute and Chronic Pancreatitis
Pancreatitis is inflammation of the pancreas, acute or chronic. Acute pancreatitis is sudden and may get better with treatment. Chronic pancreatitis lasts long and can cause permanent damage.
Causes include gallstones, alcohol, and some meds. Symptoms are severe pain, nausea, and vomiting. Doctors use blood tests, CT scans, and endoscopy for diagnosis.
“Early diagnosis and treatment of pancreatitis are key to avoid complications and better outcomes.” -A leading gastroenterologist
- Acute pancreatitis needs quick medical help to manage pain and prevent issues.
- Chronic pancreatitis needs long-term care, including lifestyle changes and sometimes surgery.
Pancreatic Cancer and Tumors
Pancreatic cancer is serious with a poor prognosis, often due to late diagnosis. Risks include smoking, family history, and genetic syndromes.
|
Risk Factor |
Description |
|---|---|
|
Smoking |
Smoking doubles the risk of pancreatic cancer. |
|
Family History |
Having a first-degree relative with pancreatic cancer increases risk. |
|
Genetic Syndromes |
Certain genetic conditions, like BRCA2 mutations, can increase risk. |
Diagnosis involves imaging, biopsy, and genetic testing. Treatment depends on the stage and may include surgery, chemotherapy, and radiation.
Pancreatic Cysts and Pseudocysts
Pancreatic cysts are fluid-filled sacs in the pancreas, which can be benign or cancerous. Pseudocysts are fluid collections that can develop after pancreatitis or trauma.
Diagnosis is through imaging like ultrasound or MRI. Management depends on the cyst’s type, size, and symptoms. Some cysts need drainage or surgery.
- Small, asymptomatic cysts may be monitored with regular imaging.
- Large or symptomatic cysts often need intervention to prevent complications.
Understanding these pancreatic conditions is key for timely referral and proper management. This improves patient outcomes.
Referral Statistics and Urgency Levels
Referral statistics show how urgent and complex hepatobiliary cases are. They guide specialist care. It’s key to manage these conditions well.
Understanding Urgent vs. Non-Urgent Referrals
Hepatobiliary referrals are split into urgent and non-urgent. Urgent referrals are for serious conditions needing quick action. Examples include acute liver failure or obstructive jaundice.
Non-urgent referrals are for important but not emergency conditions. These include chronic hepatitis or gallstones without sudden symptoms.
Statistical Breakdown of Hepatobiliary Referral Types
Most hepatobiliary referrals are urgent. For example, bile duct obstruction or acute pancreatitis need quick care.
- Urgent referrals: 40% of total referrals
- Non-urgent referrals: 60% of total referrals
Factors Determining Referral Priority
Several things decide how urgent a referral is. These include symptom severity, complicating factors, and the patient’s health.
- Severity of symptoms: Severe symptoms like jaundice or pain get priority.
- Presence of complicating factors: Conditions like cirrhosis or liver disease make referrals urgent.
- Patient’s overall health: Patients with many health issues or a weak immune system are high priority.
Understanding these factors and referral types helps healthcare providers. They can ensure patients get the right care on time.
The Referral Process and Pathway Challenges
The journey from primary care to specialist care has many steps and challenges. For those with hepatobiliary conditions, knowing this process is key for timely care.
From Primary Care to Specialist: The Referral Journey
The referral journey starts with a primary care doctor’s check-up. If they find signs of a hepatobiliary condition, they might send the patient to a specialist. This choice is based on guidelines and the patient’s needs.
After the referral, the patient must give their medical history and do some tests. This info is then sent to the specialist for the first meeting.
Current Challenges in Referral Pathways
Despite the need for quick referrals, several issues can slow things down. These include:
- Long waits for specialist appointments
- Incorrect or missing info sent to specialists
- Poor communication between primary care and specialists
Fixing these problems needs teamwork from healthcare providers to improve the referral process.
Preparing for Your First Hepatobiliary Consultation
To get the most from your first visit, patients should:
- Collect all medical records and test results
- Write down symptoms and questions
- Bring a list of current medications
Being ready ensures the specialist has all the info needed for a correct diagnosis and treatment plan.
Specialized Treatments Available Through Hepatobiliary Care
Hepatobiliary care offers many ways to manage complex digestive diseases. Specialists in this field provide treatments tailored to each patient’s needs. This includes conditions of the liver, gallbladder, and pancreas.
Medical Management Options
Medical management is often the first step for many diseases. It uses medicines to control symptoms, slow disease growth, and handle complications. For example, people with liver diseases might take drugs to reduce inflammation or manage conditions like cirrhosis or hepatitis.
Common medical management strategies include:
- Pharmacological interventions to manage symptoms and disease progression
- Lifestyle modifications, such as dietary changes and alcohol cessation
- Monitoring and management of complications associated with hepatobiliary diseases
“Effective management of hepatobiliary diseases requires a holistic approach. This includes medical treatment, lifestyle adjustments, and regular monitoring.” – Hepatobiliary Specialist
Interventional Procedures
For those needing more than just medicine, interventional procedures offer a less invasive option than surgery. These methods can diagnose and treat various conditions, like bile duct blockages and gallstones.
Examples of interventional procedures include:
|
Procedure |
Description |
Indications |
|---|---|---|
|
ERCP (Endoscopic Retrograde Cholangiopancreatography) |
A technique that combines endoscopy and fluoroscopy to diagnose and treat conditions of the bile and pancreatic ducts. |
Bile duct obstruction, gallstones, pancreatitis |
|
Percutaneous Transhepatic Cholangiography (PTC) |
A procedure that involves injecting contrast material into the bile ducts through the skin to visualize the biliary tree. |
Bile duct obstruction, diagnostic purposes |
Surgical Approaches for Hepatobiliary Conditions
Surgery is often needed for complex or advanced diseases. The type of surgery, open or laparoscopic, depends on the patient’s condition and the disease’s nature.
Surgical options may include:
- Liver resection for tumors or damaged liver tissue
- Gallbladder removal (cholecystectomy) for gallstones or cholecystitis
- Pancreatic surgery for pancreatic cancer or other pancreatic disorders
In conclusion, hepatobiliary care offers a wide range of treatments. From medical management and interventional procedures to surgery, patients get the best care for their specific condition.
Long-term Care and Retention in Specialist Services
For patients with liver and bile duct issues, long-term care is key. It helps manage complex conditions. A strong relationship with specialized healthcare providers is needed.
Importance of Continued Specialist Care
Getting ongoing care from specialists is very important. It means patients get the right treatment for their needs. It also helps catch problems early, so they can be treated quickly.
Key benefits of continued specialist care include:
- Personalized treatment plans
- Monitoring for disease progression
- Adjustments to treatment as needed
- Enhanced patient education and support
Factors Affecting Patient Retention Rates
Keeping patients in specialist care depends on several things. Healthcare providers need to know these to improve care and patient happiness.
Some of the key factors include:
- The quality of the patient-provider relationship
- Accessibility of care and follow-up appointments
- Patient education and engagement in their care
- The effectiveness of the treatment plan
Multidisciplinary Approach to Complex Cases
For tough liver and bile duct cases, a team effort is best. This means doctors from different fields working together. They provide a full range of care.
|
Specialty |
Role in Hepatobiliary Care |
|---|---|
|
Gastroenterology |
Diagnosis and management of liver and bile duct disorders |
|
Surgery |
Surgical interventions for hepatobiliary conditions |
|
Oncology |
Management of liver and bile duct cancers |
Using a team approach helps ensure patients get the best care for their complex needs.
Conclusion: Navigating Your Hepatobiliary Referral Journey
Understanding and preparing for your hepatobiliary referral journey is key. Getting to specialist care on time is vital for managing liver and bile duct issues. We’ve looked at the complexities of the hepatobiliary system, why referrals happen, and why specialist care matters.
Knowing about the referral process and the tests and treatments available can empower patients. Recognizing symptoms and risk factors early helps get the right care quickly. This ensures patients get the care they need.
Managing liver and bile duct conditions well depends on getting specialist care fast. By navigating the referral journey well, patients can get the specialized care they need. This helps manage their condition effectively.
FAQ
What is a hepatobiliary referral, and why might I need one?
A hepatobiliary referral is a doctor’s advice to see a specialist. This specialist deals with liver, gallbladder, and pancreatic issues. You might need one if you have symptoms or test results showing problems with these organs.
What are the common symptoms of bile duct obstruction?
Common symptoms include jaundice, dark urine, pale stools, itching, and abdominal pain. These happen because bile can’t flow into the intestine. This leads to a buildup of bilirubin in the blood.
What causes bile duct obstruction?
Bile duct obstruction can be caused by gallstones, tumors, inflammation, or narrowing. It can also be due to external compression or a congenital condition.
How is obstructive biliary disease diagnosed?
Diagnosis involves blood tests and imaging studies like ultrasound, CT, or MRI scans. Sometimes, ERCP is used to directly see the bile ducts and treat the obstruction.
What are the treatment options for bile duct obstruction?
Treatment options include endoscopic procedures, surgery, or other interventions. These aim to remove blockages, bypass or remove obstructions, and manage symptoms.
Can liver disease be treated, and how?
Yes, liver disease can be treated. Treatment depends on the cause and stage. It may include lifestyle changes, medications, or in severe cases, liver transplantation.
What are the signs that I should see a hepatobiliary specialist?
Signs include persistent or severe abdominal pain, jaundice, and significant changes in bowel movements or urine color. These suggest liver, gallbladder, or pancreatic disorders.
How do I prepare for my first hepatobiliary consultation?
To prepare, gather all medical records and test results. Make a list of your symptoms and any medications you’re taking. This helps your specialist understand your situation better.
What is the role of a hepatobiliary specialist in managing my care?
A hepatobiliary specialist diagnoses and manages liver, gallbladder, and pancreatic conditions. They provide treatments like medical management, interventional procedures, and surgery tailored to your needs.
Why is long-term care important for hepatobiliary conditions?
Long-term care is key for chronic conditions. It prevents complications and improves quality of life. Regular follow-ups help monitor the disease and adjust treatments as needed.
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6246548/





