Patients with bile and pancreatic duct problems can find relief through ERCP.bile duct stent procedureWhat Doctor to See For Blood Clots in Legs and How Is DVT Recovery Managed? This method is a less invasive way to diagnose and treat these issues. It helps improve patients’ lives and quality of care.
An ERCP uses a thin, flexible tube called an endoscope. It goes through the mouth, esophagus, and stomach into the duodenum. This lets our team see the bile and pancreatic ducts with X-ray imaging. They can then accurately diagnose and treat any blockages or problems.
Our team uses advanced ERCP techniques to place a stent. This helps restore biliary flow and makes patients more comfortable. This life-improving procedure shows the progress in medical technology and our dedication to top-notch care.
Key Takeaways
- ERCP is a minimally invasive procedure used to diagnose and treat bile and pancreatic duct issues.
- The procedure involves passing an endoscope through the mouth into the duodenum.
- X-ray imaging is used during ERCP to visualize the bile and pancreatic ducts.
- Stent placement via ERCP can restore biliary flow and improve patient outcomes.
- Advanced ERCP techniques enhance the precision and effectiveness of the procedure.
Understanding Biliary Obstruction and Stenting
It’s important to know why biliary obstruction happens and what it can lead to. This blockage stops bile from flowing from the liver to the intestine. This can harm the liver and cause other problems.
Common Causes of Bile Duct Blockages
Many things can block bile ducts, like gallstones, tumors, and narrowings. Gallstones are a big cause, as they can move into the bile ducts. Tumors, both good and bad, can also block the ducts. Narrowings, from injury or surgery, can stop bile from flowing.
Role of Stents in Restoring Bile Flow
Stents are key in fixing bile flow problems. By using ERCP (Endoscopic Retrograde Cholangiopancreatography), we can put a stent in to open the blockage. This lets bile flow into the intestine again. It helps with symptoms like jaundice and itching and improves liver health.
Clinical Presentations Requiring Intervention
People with bile flow problems often have jaundice, dark urine, and itching. They might also feel pain, have a fever, and lose weight. These signs mean they need help to fix the blockage and get bile flowing right again. Stenting through ERCP is a good way to help them, making them feel better and live better.
The Bile Duct Stent Procedure: Overview and Approaches
ERCP is now the top choice for placing bile duct stents. It’s less invasive and can treat many problems. We’ll look at the different ways to stent the bile duct, their benefits, and when to use them.
Endoscopic vs. Percutaneous Approaches
There are two main ways to stent the bile duct: endoscopic and percutaneous. The endoscopic method uses ERCP. It goes through the mouth and guides the stent to the bile duct with cameras and X-rays. The percutaneous method goes through the skin, often with ultrasound or CT help.
Each method has its own benefits. Doctors choose based on the patient’s health, the cause of the blockage, and any special anatomy.
Advantages of ERCP for Stent Placement
ERCP is often the best choice for stenting the bile duct. It’s less invasive, leading to quicker recovery and fewer complications. It also lets doctors see the bile duct clearly, making stent placement more accurate.
ERCP has many benefits. It’s safer than surgery, causes less pain, and can handle many problems in one go.
When Each Approach is Indicated
Choosing between endoscopic and percutaneous stenting depends on several factors. ERCP stenting is best for blockages caused by stones, strictures, or tumors that can be reached endoscopically.
Percutaneous stenting is better when endoscopy can’t reach the blockage. This might be due to previous surgery or complex strictures.
The right approach depends on the patient’s specific situation and the doctor’s skills. Each case is unique, and the best method varies.
Patient Preparation for ERCP Stent Placement
Getting ready for ERCP stent placement is key. This includes checking health, managing meds, and teaching patients. Doing these steps well helps avoid risks and makes the procedure a success.
Pre-procedure Assessment and Testing
Before the ERCP, patients get a full check-up. This is to spot any risks or problems. Here’s what happens:
- Medical History Review: We look at the patient’s health history to see if it might affect the procedure.
- Laboratory Tests: Blood tests and other tests to check the patient’s health and find any issues.
- Imaging Studies: Tests like CT scans or MRI to see the bile ducts and find any blockages.
This helps us make the procedure fit the patient’s needs and lower the chance of problems.
Medication Management Protocol
Managing meds is a big part of getting ready. Patients must:
- Disclose All Medications: Tell their doctor about all meds they’re taking, like blood thinners and diabetes meds.
- Adjust Medications as Necessary: Change or stop some meds to lower the risk of bleeding or other issues during the procedure.
Our team gives clear instructions on managing meds to keep patients safe during the ERCP.
Fasting Guidelines and Patient Instructions
Patients need to fast before the procedure to avoid aspiration risks. Our team gives specific advice on:
- Fasting Duration: How long to fast before the procedure.
- Dietary Restrictions: What foods to avoid before the procedure.
- Pre-procedure Care: More instructions on getting ready, like when to arrive and what to bring.
Following these guidelines is important for a safe and successful ERCP stent placement.
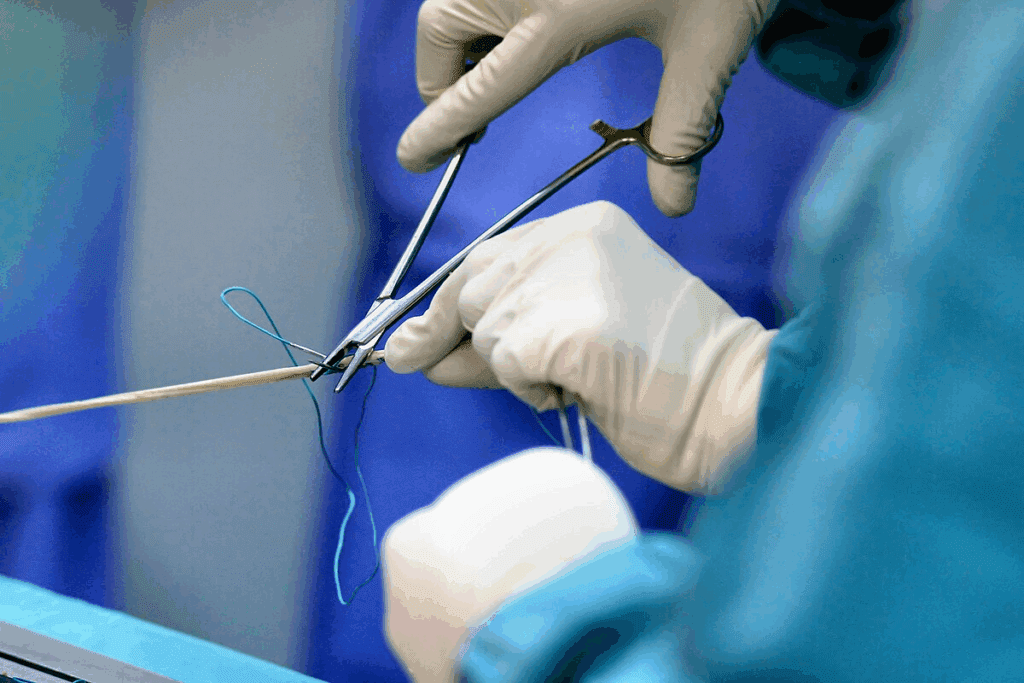
Equipment and Team Required for Biliary Stent Insertion
To do ERCP with stent placement well, you need top-notch equipment and a team that works together.
Endoscopic Equipment and Accessories
The process of putting in a biliary stent depends a lot on advanced endoscopic tools. These include:
- Duodenoscopes with high-resolution imaging
- Sphincterotomes for precise cannulation
- Guidewires for navigating the biliary tree
- Balloon catheters for dilation when needed
These tools help us see the bile duct clearly and do the stenting job right.
Stent Delivery Systems
Stent delivery systems are key for putting in biliary stents right. We use:
- Plastic stents for some benign conditions
- Self-expanding metal stents (SEMS) for malignant obstructions
- Stent delivery catheters for precise placement
Multidisciplinary Team Composition
A team from different fields is essential for biliary stent insertion success. Our team has:
- Gastroenterologists with ERCP expertise
- Radiologists for imaging guidance and interpretation
- Nurses and endoscopy assistants for patient care and support
- Anesthesiologists for sedation and monitoring
This team effort ensures our patients get the best care and results from biliary stent insertion.
Step-by-Step ERCP Procedure for Bile Duct Stenting
We take great care in every step of the ERCP procedure. This includes patient positioning and stent placement. The ERCP is a detailed process aimed at successful bile duct stenting.
Patient Positioning and Sedation
The first step is getting the patient ready. We place them on their stomach or side, depending on the procedure. Sedation helps them relax and stay comfortable.
Conscious sedation is used. This way, the patient can stay awake but feel relaxed.
Duodenoscope Insertion Technique
With the patient ready, we insert the duodenoscope. It goes through the mouth, esophagus, and stomach, reaching the duodenum. The duodenoscope has a camera and tools for seeing and working on the bile duct.
Cannulation of the Biliary Tree
Cannulation is a key step. We use the duodenoscope to reach the bile duct and insert a cannula. This tube injects contrast material for better visualization.
This step helps us see any blockages or issues. For more details, visit ERCP page.
Cholangiography and Obstruction Assessment
After cannulation, we do cholangiography. This involves X-ray images after contrast material is injected. It helps us find any obstructions or issues.
Based on these findings, we decide on the best stenting plan.
| Step | Description | Key Considerations |
| Patient Positioning and Sedation | Positioning the patient and administering sedation | Patient comfort and safety |
| Duodenoscope Insertion | Guiding the duodenoscope through the digestive tract | Scope manipulation and visualization |
| Cannulation of the Biliary Tree | Accessing the bile duct with a cannula | Precision and accuracy |
| Cholangiography and Obstruction Assessment | Visualizing the bile duct and assessing obstructions | Contrast material and X-ray imaging |
Types of Stents Used in ERCP and Stenting
Choosing the right stent in ERCP depends on many things. This includes the problem and what’s best for the patient. Making the right choice is key to a good outcome.
Plastic Stents: Characteristics and Applications
Plastic stents are often used in ERCP because they’re easy to put in and take out. They’re made from materials like polyethylene or Teflon and come in different sizes. They’re good for problems like bile duct stones or strictures and are cheaper than metal stents.
One big plus of plastic stents is how easy they are to remove. This makes them great for temporary needs. But, they can get blocked more easily and might need to be replaced more often than metal stents.
Self-Expanding Metal Stents (SEMS)
Self-expanding metal stents (SEMS) are another choice for stenting. They expand to fit the bile duct better than plastic stents. This makes them good for serious blockages because they stay open longer.
SEMS are made from materials like nitinol and stainless steel. They fit well in the bile duct and are less likely to move around.
Covered vs. Uncovered Metal Stents
Metal stents can be covered or uncovered. Covered stents have a layer that stops tumors from growing into the stent. Uncovered stents let some tissue grow into the stent, helping it stay in place.
Choosing between covered and uncovered stents depends on the situation. Covered stents are better for stopping tumor growth. Uncovered stents are used when there’s a risk of the stent moving.
Stent Selection Based on Pathology
The type of problem affects which stent is best. For simple problems, plastic stents are often used because they’re easy to remove and less expensive. For serious blockages, metal stents are preferred because they stay open longer.
Other things, like the patient’s health, also play a part in choosing a stent. It’s important to consider all these factors to find the best stent for each patient.
Post-ERCP With Stent Placement Care
After an ERCP with stent placement, we take a detailed approach to care. This is to manage symptoms and avoid complications. We know how important this time is for your recovery and comfort.
Immediate Recovery Monitoring
Right after the ERCP with stent, you’ll be watched closely in a recovery area. We check your vital signs and look for any signs of bleeding, perforation, or other bad reactions.
This monitoring lasts a few hours. We check how you’re doing and manage any pain or discomfort. This helps us catch any problems early and make sure you recover well.
Pain and Symptom Management
Managing pain is key after an ERCP. We use different methods to help with discomfort, like medicine and other support. We also tell you how to handle symptoms at home, like belly pain or bloating.
Good symptom management makes you more comfortable. It also helps us spot any problems early. We teach you what to expect and when to get help.
Diet Progression Protocol
We give you special diet advice as you recover. First, you might need to stick to a clear liquid diet. Then, you can start eating solid foods as you feel ready. We tailor your diet to your needs and how you’re doing.
A good diet plan helps you feel better and lowers the risk of problems. We also tell you which foods to avoid and which are good for you during recovery.
Discharge Instructions and Red Flags
Before you go home, we give you all the details on caring for yourself after the procedure. We also tell you about signs of serious problems to watch for, like severe belly pain, fever, or bleeding.
It’s very important to understand these instructions to stay safe and recover well. We make sure you know what to do next and when to get help right away.
| Care Aspect | Description | Patient Action |
| Immediate Recovery | Monitoring for complications | Rest and follow hospital instructions |
| Pain Management | Medication and supportive care | Take medication as directed |
| Diet Progression | Gradual introduction of foods | Follow dietary advice provided |
| Discharge Instructions | Understanding red flags and follow-up | Recognize signs of complications and attend follow-up appointments |
Potential Complications of Liver and Bowel Duct Stenting
Stenting in the liver and bowel ducts comes with risks. It’s a common treatment for blockages but can lead to complications. These can be related to the procedure or the stent itself.
Procedure-Related Complications
Complications from the ERCP procedure are direct results. These include:
- Pancreatitis: Inflammation of the pancreas is a known risk of ERCP.
- Bleeding: Bleeding can occur during or after the procedure.
- Infection: Introduction of bacteria into the biliary system can lead to infection.
- Perforation: Though rare, perforation of the duodenum or bile duct can occur.
These issues are managed by careful patient selection, precise technique, and monitoring after the procedure.
Stent-Specific Complications
Stent-specific complications can also happen. These include:
- Stent Occlusion: Blockage of the stent can occur due to sludge, tumor ingrowth, or other factors.
- Stent Migration: The stent can migrate from its original position, potentially causing complications.
Addressing these complications often requires additional procedures to clear or replace the stent.
Management Strategies
Managing complications involves preventive measures and timely intervention. Strategies include:
- Monitoring: Close follow-up to detect issues early.
- Endoscopic Intervention: Repeat ERCP to address complications such as stent occlusion.
- Antibiotic Prophylaxis: Use of antibiotics to prevent infection in certain cases.
Prevention Techniques
Preventing complications is key to successful stent placement. Techniques include:
- Careful Patient Selection: Assessing the risk-benefit ratio for each patient.
- Technical Precision: Ensuring that the stent placement is done with high precision.
- Post-Procedure Care: Providing clear instructions and follow-up care to patients.
Understanding complications and using strategies to manage and prevent them can improve patient outcomes. This is true for liver and bowel duct stenting.
Success Rates and Outcomes of Biliary Stent Placement
Biliary stenting is known for its high success rates and many benefits. It works well in getting bile flow back, mainly for those with cancer blockages.
Technical Success Rates
The success rate of biliary stent placement is very high, over 90%. This success comes from better stent technology and skilled endoscopists.
Key factors contributing to high technical success rates include:
- Improved stent design and materials
- Enhanced visualization techniques during ERCP
- Expertise of the medical team
Clinical Effectiveness in Benign vs. Malignant Disease
Biliary stenting works for both benign and malignant conditions. But, the results can differ based on the cause. For cancer, it greatly improves life quality.
Clinical effectiveness is measured by:
- Successful relief of obstruction
- Improvement in liver function tests
- Reduction in symptoms such as jaundice and pruritus
Quality of Life Improvements
Patients with biliary stent placement see big life quality boosts. It helps get rid of symptoms that mess up daily life.
Notable improvements include:
- Reduced jaundice and itching
- Improved nutritional status
- Enhanced overall well-being
Stent Patency Duration and Factors Affecting Longevity
How long a biliary stent stays open depends on many things. These include the stent type, the disease, and the patient’s health.
Factors influencing stent patency include:
| Factor | Description | Impact on Patency |
| Stent Type | Plastic vs. metal stents | Metal stents generally have longer patency |
| Disease Pathology | Benign vs. malignant | Malignant disease often requires more frequent interventions |
| Patient Factors | Presence of comorbidities | Can affect overall health and stent function |
Knowing these factors helps us better manage patient hopes and improve stent performance.
Conclusion: Advances in Bile Duct Stent Procedures and Future Directions
Advances in bile duct stenting have greatly improved patient care. They help restore bile flow and ease symptoms of biliary obstruction. New stent designs and placement methods have made liver stent surgery more effective.
Looking ahead, research is focused on making stents last longer and work better. They also aim to improve placement techniques to reduce complications. These efforts will likely make patient care even better.
We are dedicated to providing top-notch healthcare through the latest in biliary stenting. Our goal is to continually improve liver stent surgery. This way, we can offer the best results for our patients.
FAQ
What is ERCP and how is it used for bile duct stent placement?
ERCP stands for Endoscopic Retrograde Cholangiopancreatography. It’s a way to look at and fix problems in the bile ducts and pancreas. We use it to put a stent in the bile duct to help bile flow.
What are the common causes of biliary obstruction that require stenting?
Biliary obstruction can happen due to gallstones, tumors, or strictures. Stents help restore bile flow and ease symptoms like jaundice and pain.
What are the advantages of ERCP for stent placement compared to percutaneous approaches?
ERCP is less invasive, leading to quicker recovery. It also lets us do stent placement and other treatments in one go. We choose ERCP over other methods for these reasons.
How do I prepare for ERCP stent placement?
Before ERCP, you’ll need to have tests and follow fasting rules. We also ask you to manage your medications. Following these steps is key for a safe procedure.
What type of stent is used in ERCP and how is it chosen?
We use different stents, like plastic and metal ones. The type chosen depends on the problem and the patient. We pick the best stent for each case.
What are the possible complications of liver and bowel duct stenting?
Complications can include pancreatitis and stent problems. We have ways to manage and prevent these issues.
What is the success rate of biliary stent placement?
Stent placement is usually successful. The success rate depends on the disease type. We see better quality of life and stent function over time.
What are the post-procedure care instructions after ERCP with stent placement?
After the procedure, you’ll be watched for recovery. We’ll manage pain and symptoms. You’ll get instructions on diet and what to watch for after leaving the hospital.
How is biliary stent placement performed?
The procedure involves several steps. These include positioning, sedation, and using a duodenoscope. A team of experts performs it.
What are the benefits of biliary stent placement using ERCP?
ERCP stent placement is a minimally invasive method. It offers relief from obstruction and improves outcomes. We use it for many conditions.
References
- Centers for Disease Control and Prevention (CDC). (2022). ERCP – Endoscopic Retrograde Cholangiopancreatography. U.S. Department of Health & Human Services. https://www.cdc.gov/nchs/fastats/er/endoscopy.htm


































