
Recent studies show that survival rates for blood clot patients differ a lot. This depends on where the clot is and the person’s health.Understand the survival rate of a blood clot in heart survival rate, life expectancy factors, and effective treatments that improve outcomes.
For those with pulmonary embolism, knowing how it affects life expectancy is key.
It’s important to know about blood clots to stay healthy. Blood clots are like gel-like clumps that form when the body gets hurt or when blood clotting factors get out of balance.
These clots can happen anywhere in the body. Knowing the risk factors and symptoms is key to getting help quickly.
Blood clots are classified by where they form and the problems they cause. For example, Deep Vein Thrombosis (DVT) is when clots form in the deep veins of the legs. Pulmonary Embolism (PE) is when clots reach the lungs.
Arterial clots can lead to heart attacks or strokes. Thrombophlebitis is when clots form in the veins just under the skin.
Blood clotting is a complex process that involves blood flow, clotting factors, and the condition of blood vessel walls. When a blood vessel gets hurt, the body tries to stop bleeding by forming a clot.
Sometimes, clots can form without an injury. This often happens because of health conditions or genetics.
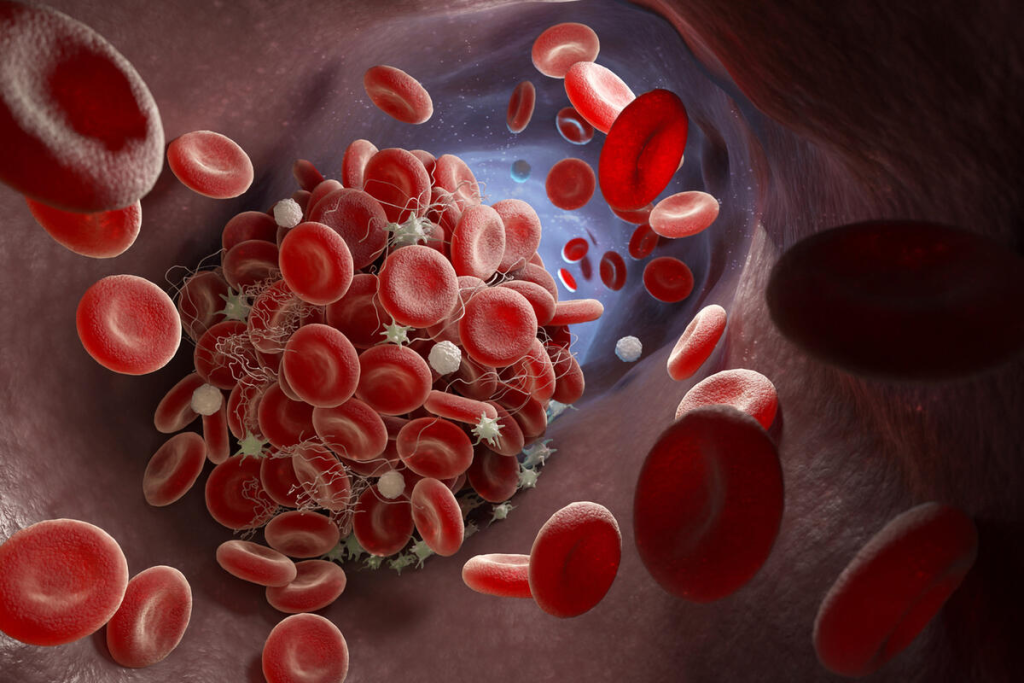
Blood clots can form anywhere in the body. But they most often appear in the legs (DVT), lungs (PE), heart, and brain. Where the clot forms affects symptoms and possible complications.
| Location | Common Condition | Potential Complications |
| Legs | Deep Vein Thrombosis (DVT) | Pulmonary Embolism (PE), Post-Thrombotic Syndrome |
| Lungs | Pulmonary Embolism (PE) | Respiratory failure, Cardiac arrest |
| Heart | Cardiac Thrombosis | Heart Attack, Cardiac failure |
| Brain | Cerebral Venous Thrombosis | Stroke, Seizures |
To manage blood clot risks, it’s important to understand these aspects. This includes living a healthy lifestyle, watching for symptoms, and following doctor’s advice if you’re at risk.
Understanding the statistics on surviving a blood clot in the heart is key. The survival rate for heart-related blood clots has greatly improved over time.
Quick treatment is vital. Research shows that fast action can greatly improve patient outcomes. “Effective and timely treatment is critical in saving lives,” as recent studies highlight.
The size of the clot, the area affected, and overall health are important for long-term survival. Long-term survival also depends on the treatment’s success and the patient’s follow-up care.
The survival rate for pulmonary embolism (PE) changes with age. As we get older, our bodies change in ways that affect recovery from serious illnesses. Knowing how age affects survival rates helps doctors create better treatment plans.
Research shows that survival rates for PE drop as age increases. People under 50 tend to have a much higher survival rate than those over 70. A study found that the 30-day death rate for those under 50 was about 2%. But for those over 70, it was around 12%.
Several factors lead to lower survival rates in older adults. Older patients often have health issues like heart disease, diabetes, or COPD. These conditions can make treatment harder and outcomes worse. Also, older adults may have less energy to recover from a pulmonary embolism.
Despite age-related challenges, medical progress has improved survival rates for all ages. Early diagnosis and timely treatment have led to better outcomes. For instance, using anticoagulant and thrombolytic therapies has shown to increase survival chances in pulmonary embolism patients.
Understanding what happens after a pulmonary embolism (PE) is key for both patients and doctors. The outcome can depend on how severe the PE was, any health issues the person had before, and how well treatment worked.
The first few weeks are very important. Doctors watch for any problems and start treatment to stop more clots.
Later on, patients might face chronic thromboembolic pulmonary hypertension (CTEPH). This is high blood pressure in the lungs’ blood vessels. Regular check-ups are needed to handle these risks.
One big worry is that the clot could come back. But, studies show that the right treatment can lower this risk a lot. Using anticoagulants can greatly reduce the chance of another PE.
Pulmonary embolism is a big threat to heart health. Its mortality rates show how serious it is. We look at the latest stats, past trends, and how it compares to other heart issues to grasp the risks.
Recent studies show the death rate from pulmonary embolism is going down. This is thanks to better diagnosis and treatment. Early detection and proper care are key to lowering death rates. The drop in death rates comes from better healthcare and more awareness.
In the past, pulmonary embolism was very deadly. But, thanks to better understanding and treatment, survival rates have improved. New anticoagulant therapies and better imaging have helped a lot. We need to keep researching and improving care to keep death rates down.
When we compare pulmonary embolism to other heart diseases, it’s clear PE is a big risk. But, it’s not the deadliest among heart diseases. Myocardial infarction and stroke have higher death rates. Knowing this helps us focus our health efforts and awareness campaigns.
By studying the death rate of pulmonary embolism, we can see how well treatments work. We can also find areas to get better. Keeping up with research and spreading awareness are vital to fight pulmonary embolism risks.
Silent pulmonary embolism is a condition where people might not show typical symptoms of PE. This makes it hard to diagnose because there are no obvious signs. As a result, getting medical help can be delayed.
Pulmonary embolism often shows symptoms like shortness of breath, chest pain, and coughing. But in silent PE, these signs can be mild or not there at all. Some people might only feel very slight or vague symptoms that don’t point to a pulmonary embolism.
Why don’t people notice these symptoms? It could be because the clot is small or in a tricky spot. Or it might be because some people can handle the blockage better than others. This means silent PE can be missed until it gets worse or is found by accident during tests for something else.
How long it takes for symptoms to show up in pulmonary embolism can really vary. Some people might feel symptoms right away, while others might not notice anything for a long time. This difference depends on things like how big the clot is, any heart or lung problems, and the person’s overall health.
Symptoms can change over time, like if the clot gets smaller or if the body finds ways to work around it. But even without symptoms, a pulmonary embolism can be very dangerous. This is true, even if the clot is small or if it happens more than once.
There are a few reasons why diagnosing pulmonary embolism can be delayed. Not knowing about the symptoms and risks of PE is a big one. Also, having other health problems like heart failure or lung disease can make it harder to figure out if someone has a PE.
Knowing about these risk factors is key to catching pulmonary embolism early, even in silent cases. By being aware of the possibility of no symptoms and watching for small signs, we can get better at diagnosing and treating PE on time.
Fatal pulmonary embolism is a serious condition that needs immediate help. Knowing the warning signs and how fast to act is key to saving lives.
Signs of a fatal pulmonary embolism include severe shortness of breath and chest pain. Coughing up blood and feeling lightheaded are also warning signs. Recognizing these symptoms early is vital for timely intervention.
In some cases, a pulmonary embolism can cause sudden collapse or cardiac arrest. Immediate medical response is necessary to prevent death.
The time from symptoms to death can be very short, often just hours. Prompt medical treatment is essential to prevent fatal outcomes.
The speed of a pulmonary embolism’s progression depends on several factors. These include the size of the clot and the individual’s health. Understanding these factors can help in assessing the risk and taking appropriate action.
In cases of suspected pulmonary embolism, emergency services should be contacted immediately. The response time can significantly impact the outcome, with timely intervention being critical to survival.
We emphasize the importance of acting quickly when symptoms are recognized. Every minute counts in preventing a fatal outcome.
Patients often wonder about their life expectancy after being diagnosed with DVT. Deep Vein Thrombosis is a serious condition where a blood clot forms in a deep vein, usually in the legs. The recovery period and long-term complications greatly affect a patient’s health outcome.
The first step in treating DVT is anticoagulation therapy. This prevents the clot from growing and lowers the risk of pulmonary embolism. We use medications like heparin and warfarin, and newer options like direct oral anticoagulants (DOACs). The success of this therapy is key in the early recovery.
Long-term DVT complications can impact life expectancy and quality of life. A major complication is post-thrombotic syndrome (PTS). It causes chronic pain, swelling, and skin changes in the affected limb. Other issues include recurrent DVT and pulmonary embolism.
PTS can significantly affect a patient’s quality of life. Symptoms range from mild to severe, including pain, heaviness, and swelling in the leg. Managing PTS involves compression therapy, pain management, and lifestyle changes. Regular follow-ups with healthcare providers are also important to monitor the condition and adjust treatments as needed.
| Factor | Impact on Life Expectancy | Management Strategies |
| Effectiveness of Anticoagulation Therapy | Highly effective therapy improves survival rates. | Regular monitoring of anticoagulation levels, adherence to medication. |
| Presence of Post-Thrombotic Syndrome | PTS can reduce quality of life and potentially affect life expectancy. | Compression therapy, pain management, lifestyle changes. |
| Recurrent DVT | Increases the risk of complications and potentially affects life expectancy. | Long-term anticoagulation therapy, monitoring for recurrence. |
Diagnosing blood clots has seen big improvements in recent years. This has led to better survival rates for those affected. New diagnostic methods help find and treat blood clots early. This is key to avoiding serious problems and better patient results.
Techniques like CT pulmonary angiography (CTPA) have changed how we diagnose blood clots. CTPA lets doctors see the pulmonary arteries clearly. This helps them quickly spot pulmonary embolism.
Laboratory tests, like D-dimer assays, are also important. They check for D-dimer, a sign of blood clot dissolution. High D-dimer levels suggest a blood clot might be present.
Point-of-care testing (POCT) lets doctors test patients right where they are. This quick testing is great for emergency situations. It helps diagnose and treat blood clots fast.
Early detection of blood clots thanks to new methods greatly improves survival. These methods allow for quick treatment. This is a big win for patients with blood clots.
Managing blood clots well is key to better survival rates and fewer complications. We’ll look at the different treatments and how they affect patients.
Anticoagulation therapy is the main treatment for blood clots. It stops new clots from forming and helps dissolve existing ones. Medications like heparin and warfarin are used to prevent clotting.
This therapy greatly improves survival chances by stopping clot growth.
In some cases, thrombolytic therapy is used to quickly dissolve clots. It’s most helpful for big or dangerous clots. Thrombolytic agents, like alteplase, activate the body’s clot-dissolving system.
Though effective, it can increase the risk of bleeding.
For some, surgical interventions are needed to remove or bypass clots. Procedures like thrombectomy remove the clot, improving blood flow. These surgeries are for cases where other treatments can’t be used.
The field of blood clot treatment is always changing. Novel therapies and clinical trials offer new hopes for better results. Researchers are looking into safer and more effective treatments.
Joining clinical trials gives patients access to new treatments and helps medical science grow.
After a blood clot, patients face many challenges. They must deal with physical and emotional issues. Surviving a blood clot is a big win, but it’s just the start of getting back to normal.
Right after a blood clot, patients often feel limited. They might have pain, swelling, or trouble moving. For example, those with post-thrombotic syndrome may have ongoing pain and swelling in their leg.
Getting better takes time and gentle steps. Doctors usually suggest starting with simple exercises. This helps the body heal and prevents more problems.
The mental effects of surviving a blood clot are big. It can lead to anxiety, depression, or even PTSD. It’s key for patients to get support from loved ones or mental health experts.
Counseling and therapy help patients face their fears. Support groups, online or in-person, offer a sense of community and understanding.
Going back to normal after a blood clot needs careful planning. Patients must balance wanting to do things as usual with not overdoing it. This might mean taking breaks, avoiding long sitting or standing, and eating well.
Following medication is also vital. This usually means taking long-term anticoagulation therapy to stop new clots. Regular check-ups with doctors are important to keep an eye on things and adjust treatments if needed.
Managing long-term meds is a big part of life after a blood clot. Anticoagulants help prevent new clots but need regular checks. This is to make sure they’re working right and to avoid bleeding problems.
People on these meds need to know about side effects and how they interact with other drugs. They should also know how to handle small bleeds and when to get medical help.
Preventing blood clots from coming back is key. It’s important for living longer and feeling better. People who have had blood clots need a good plan to avoid more problems.
Using anticoagulants for a long time is very important. Anticoagulant medications stop blood from clotting. This helps prevent new clots from forming. It’s vital for patients to take their medicine as told.
Choosing the right anticoagulant depends on many things. This includes the patient’s health and other conditions. Newer anticoagulants might be better because they have fewer side effects and don’t need as much monitoring.
Changing your lifestyle can also help a lot. Being at a healthy weight and exercising regularly can lower clot risk. It’s also important to move around often, not sit or stand for too long.
Quitting smoking and drinking less alcohol are also good ideas. They help your heart and reduce clotting risks. Drinking enough water is also important to avoid dehydration and clotting.
Seeing your doctor regularly is a must. It helps check if the medicine is working right. It also lets you change treatment plans if needed. This care helps catch any problems early.
By using medicine, making lifestyle changes, and seeing your doctor often, you can lower your risk of blood clots. This can help you live longer and feel better. We’re here to help our patients every step of the way.
Blood clots can happen to anyone. But some groups face a higher risk. Knowing these risks helps prevent, detect, and treat blood clots effectively.
Pregnancy brings changes that raise blood clot risks. This risk grows even more after giving birth. Healthcare providers need to understand these risks to manage pregnancy complications better.
Cancer and its treatments increase blood clot risks. Some cancers, like pancreatic cancer, are more linked to blood clots. Cancer patients should watch for blood clot signs and get medical help fast.
Surgery raises the risk of blood clots, like deep vein thrombosis (DVT). Major surgeries, like those in the lower body, increase this risk. Doctors use early movement and blood thinners to lower this risk.
The COVID-19 pandemic shows a link between viral infections and blood clot risks. Severe COVID-19 cases are at higher risk. Blood thinners are often part of their treatment.
Managing blood clot risks is key to staying healthy. We’ve looked at how blood clots affect health, the need for early detection, and treatment choices.
Knowing the risks and acting early can lower your chance of getting a blood clot. Spotting signs and symptoms early helps get quick medical help. This can lead to better recovery. Managing risks means making lifestyle changes, following medication, and keeping an eye on your health.
By focusing on heart health and understanding blood clot risks, you can lower your risk of heart problems. We stress the importance of being aware and taking steps to prevent these risks.
The life expectancy with a blood clot depends on several factors. These include the type of clot, its location, and the person’s health. Treatment effectiveness, underlying health conditions, and the risk of clotting again also matter.
Some people can have a pulmonary embolism without symptoms. This is called silent PE. The time it takes for symptoms to appear can vary a lot. Some people might feel symptoms right away, while others might not notice them for a long time.
Survival rates for pulmonary embolism vary by age. Older adults face a higher risk of death from PE. This is because they may have less health reserve, other health issues, and might get diagnosed later.
A fatal pulmonary embolism can happen quickly if not treated fast. In severe cases, death can occur in just a few hours. This shows how critical quick medical help is.
Knowing the signs of a pulmonary embolism is key. Look out for severe shortness of breath, chest pain, and collapse. Quick medical care is vital to avoid fatal outcomes.
After DVT, recovery starts with anticoagulation therapy to stop clot growth and prevent more. Long-term, complications like post-thrombotic syndrome can occur. This condition causes chronic pain, swelling, and skin changes in the affected limb.
Preventing blood clots requires a full approach. This includes knowing your risk factors, recognizing symptoms, and following treatment plans. Using long-term medications, making lifestyle changes, and regular check-ups can help prevent clots from coming back.
Treating blood clots involves several strategies. These aim to stop clot growth, reduce recurrence risk, and improve survival. Treatments include anticoagulation therapy, thrombolytic treatments, surgery, and new therapies.
Surviving a blood clot can greatly impact daily life. Physical limitations, mental effects, and long-term medication needs can all affect well-being and daily activities.
Some groups, like pregnant women, cancer patients, post-surgical people, and those with COVID-19, face unique blood clot risks. It’s important to understand these risks and take steps to reduce them for better outcomes.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us