Occlusion is a key medical term. It means a blood vessel is blocked. This can lead to serious health problems.
In medical terms, occlusion happens when blood flow is blocked in an artery or vein. This is often due to coronary artery disease.
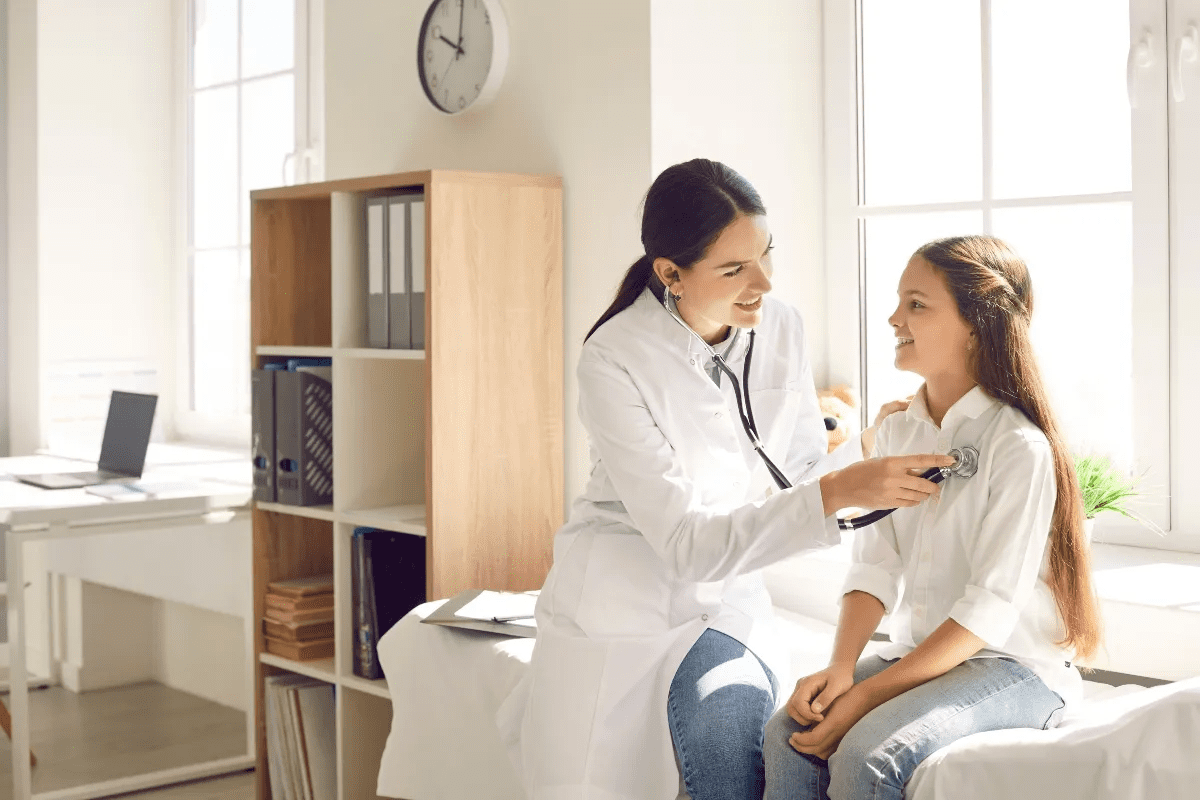
At Liv Hospital, we focus on quick diagnosis and top-notch vascular care for occlusion patients. We stress the need for fast action to avoid permanent damage or death.
What is a blood clot occlusion? Learn what this dangerous medical term means, the common types, and the critical warning signs.
Key Takeaways
- Occlusion is when a blood vessel is blocked, stopping normal blood flow.
- It’s vital to spot the signs and symptoms of occlusion early.
- Quick action is key to avoid serious health issues.
- Liv Hospital offers expert vascular care for occlusion patients.
- Getting a diagnosis and treatment fast can greatly improve patient outcomes.
The Medical Definition of Occlusion
In medical terms, occlusion means a blockage in a vessel, organ, or passageway. This can include heart attacks and strokes, or problems with teeth alignment. It’s a broad term covering many conditions.
Etymology and Historical Context
The word “occlusion” comes from the Latin “occludere,” meaning “to shut.” It’s been key in medicine, like in understanding heart diseases. Coronary occlusion was first talked about by Sir William Osler in 1910, showing its big role in heart health.
Occlusion vs. Stenosis: Understanding the Difference
Occlusion and stenosis are not the same, even though they’re related. Stenosis is when a passage or vessel narrows. If it narrows too much, it can cause an occlusion. Knowing the difference helps doctors diagnose and treat better.
Clinical Significance of Occlusive Conditions
Occlusive conditions can cause serious health problems like heart attacks and strokes. The term occlusive means any blockage, like from blood clots or fatty plaque. Quick action is key to helping patients.
We’ll keep looking into occlusion in the next parts. We’ll cover its types, causes, and how to treat it.
Types of Occlusions in Medicine
Occlusion in medicine means different blockages in the body. It’s important to know these types for diagnosis and treatment.
Vascular Occlusions
Vascular occlusions block blood vessels, which can be arteries or veins. These blockages can cause serious health problems, depending on where and how bad they are.
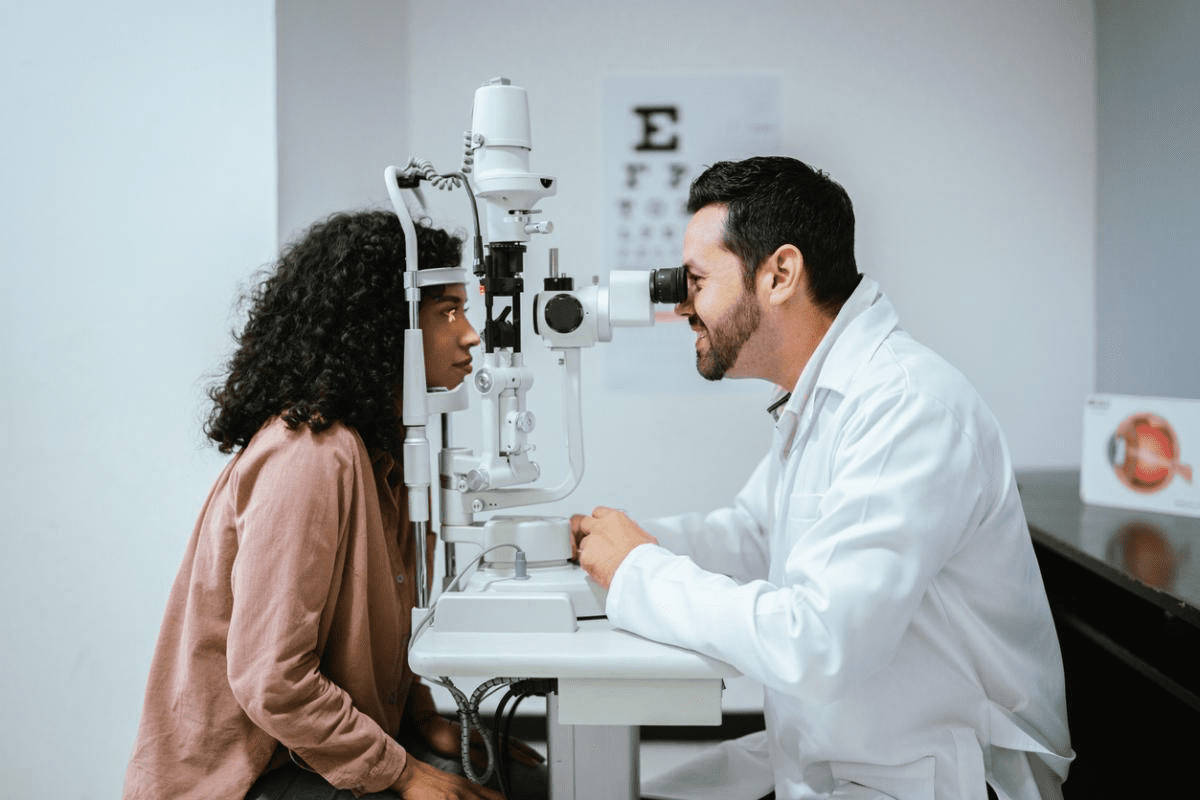
Blood clot occlusion is a common type. It happens when blood clots block blood flow. For example, central retinal vein occlusion (CRVO) affects the retina and can cause vision issues.
Common Types of Vascular Occlusions:
- Arterial thrombosis
- Venous thrombosis
- Embolic occlusions
Dental and Gastrointestinal Occlusions
In dentistry, occlusion is about how upper and lower teeth fit together. Misocclusion or malocclusion can cause tooth wear and jaw pain.
In the gastrointestinal tract, occlusion can be caused by tumors, adhesions, or volvulus. This leads to bowel obstruction.
System | Type of Occlusion | Common Causes |
Vascular | Arterial/Venous Occlusion | Thrombosis, Embolism |
Dental | Malocclusion | Genetic, Trauma |
Gastrointestinal | Bowel Obstruction | Tumors, Adhesions, Volvulus |
Other Forms of Medical Occlusions
Occlusions can also happen in other parts of the body. For example, in bile ducts (causing cholestasis) or in the urinary tract (causing obstructive uropathy).
“The understanding and management of occlusive disorders require a multidisciplinary approach, involving various medical specialties.” – Medical Expert
Exploring different types of occlusions in medicine shows each has its own causes, symptoms, and treatments. Accurate diagnosis and proper management are key to avoiding complications and improving patient care.
Blood Clot Occlusion: Mechanisms and Pathophysiology
A blood clot in a vessel can lead to serious problems. We’ll look at how blood clots block vessels. This includes the clotting process and how clots form.
The Clotting Cascade and Thrombus Formation
The clotting process is complex. It involves proteins in blood that form a clot. Thrombus formation happens when this clot blocks blood flow. Over time, plaque builds up, narrowing arteries and increasing the risk of blockage.
Platelet Aggregation in Occlusive Events
Platelet aggregation is key in occlusive events. When platelets stick together, they form a plug that can block a vessel. This process is critical in understanding how occlusions occur. Knowing about platelet aggregation helps in finding ways to prevent blockages.
Progression from Partial to Complete Vessel Blockage
Blockage can quickly move from partial to complete. As more platelets and clotting factors join, the clot grows. This can lead to serious issues like heart attacks or strokes. We’ll see how this affects patients and why quick medical help is vital.
Causes and Risk Factors for Vascular Occlusions
It’s important to know what causes vascular occlusions. These blockages in blood vessels can lead to serious problems like heart attacks and strokes. They can also cause peripheral arterial disease.
Atherosclerosis and Plaque Formation
Atherosclerosis is a big reason for vascular occlusions. It happens when plaque builds up in artery walls, narrowing them and causing blockages. Plaque formation is a mix of lipids, inflammatory cells, and smooth muscle cells.
Studies show that during acute vascular events, clots can form quickly. Diabetes, high blood pressure, and smoking can all lead to coronary artery disease. This is often due to atherosclerotic plaque.
Hypercoagulable States and Thrombophilia
Hypercoagulable states and thrombophilia increase the risk of blood clots. These can be genetic or acquired. Thrombophilia makes it more likely for clots to form and block blood vessels.
- Genetic conditions such as Factor V Leiden mutation
- Acquired conditions like antiphospholipid syndrome
- Cancer and its treatment
Lifestyle and Modifiable Risk Factors
Lifestyle choices are key in developing vascular occlusions. Risk factors like smoking, diet, exercise, and obesity can be changed. By making these changes, people can lower their risk of occlusive vascular diseases.
- Smoking cessation
- Dietary changes to reduce cholesterol and blood pressure
- Increased physical activity
Genetic and Non-modifiable Risk Factors
Some risk factors can’t be changed, but knowing about them is important. Genetic predispositions, age, and gender are examples. Family history of heart disease is also a factor.
Healthcare providers can create better prevention and treatment plans by understanding these causes and risk factors. A detailed approach is key to reducing the impact of occlusive vascular diseases.
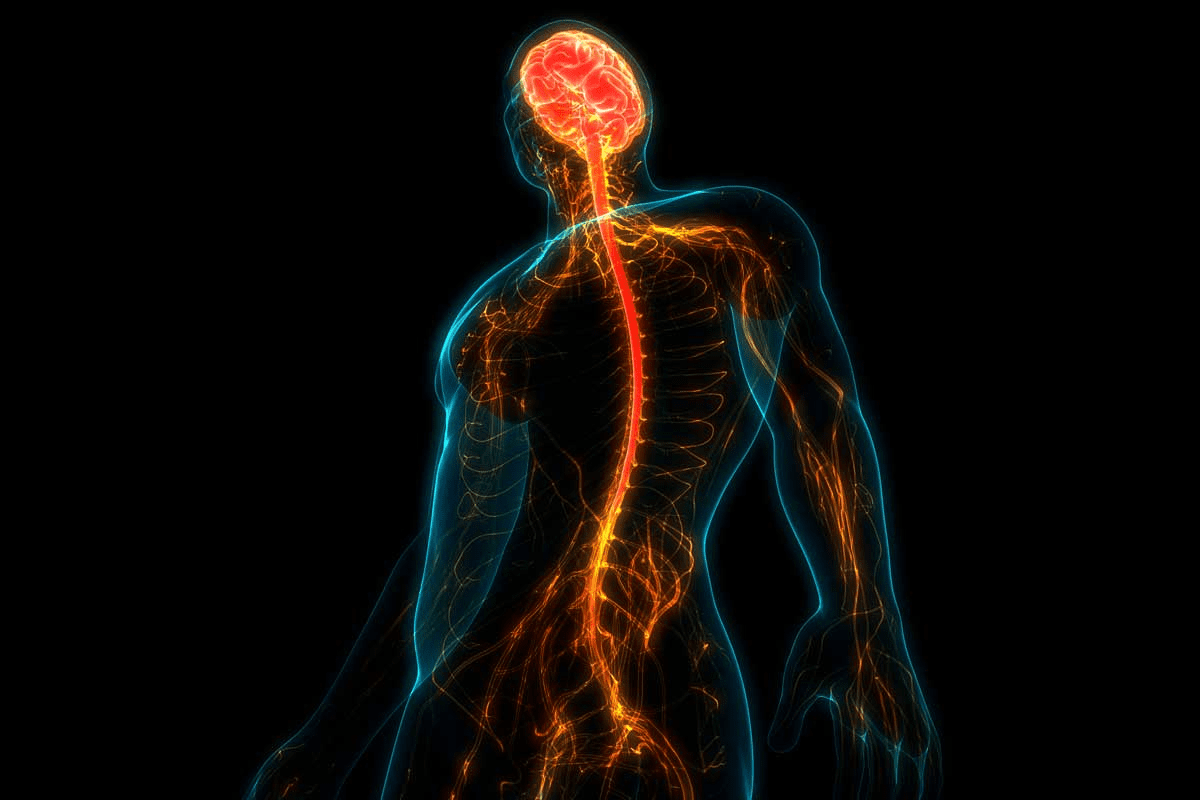
Major Occlusive Vascular Diseases
Occlusive vascular diseases are a big health threat worldwide. They cause millions of deaths each year. These diseases happen when a blood vessel gets blocked, leading to serious health crises. We will look at the main types of occlusive vascular diseases and how they affect health.
Coronary Artery Occlusion and Myocardial Infarction
Coronary artery occlusion is a dangerous disease. It happens when a coronary artery gets blocked, usually by atherosclerosis or thrombosis. This leads to a heart attack. Coronary occlusion is the leading cause of death in both men and women, showing the need for quick medical help.
“The most common cause of death in the industrialized world is coronary artery disease, and the most common cause of coronary artery disease is atherosclerosis,” highlighting the critical link between occlusive conditions and cardiovascular health.
Cerebrovascular Occlusion and Stroke
Cerebrovascular occlusion happens when a blood vessel to the brain gets blocked, causing a stroke. This can lead to serious brain damage, like paralysis, speech problems, and memory loss. Prompt treatment is key to reduce brain damage and improve results.
The effects of cerebrovascular occlusion can be very bad. It’s vital to spot risk factors and symptoms early. We must stress the need for quick medical action to manage strokes well.
Peripheral Arterial Occlusive Disease
Peripheral arterial occlusive disease (PAOD) is when arteries outside the heart and brain get blocked, usually in the legs. This can cause pain when walking, pain at rest, and tissue loss if it gets worse. PAOD can greatly lower quality of life.
Handling PAOD needs a full plan, including lifestyle changes, medicine, and sometimes surgery. We must tackle the root causes and risk factors to stop the disease from getting worse.
Clinical Manifestations of Occlusive Disorders
It’s important to know the symptoms of occlusive disorders early. This helps in getting the right treatment quickly. These conditions can affect many parts of the body, causing different symptoms.
Arterial Occlusion Symptoms
Arterial occlusions happen when an artery gets blocked. This can lead to tissue damage. The symptoms include:
- Pain in the affected limb or area, often severe and sudden
- Coldness or pallor of the skin due to reduced blood flow
- Numbness or tingling sensations as nerve function is compromised
- Weakness or loss of function in the affected area
For example, a blockage in the coronary artery can cause chest pain, shortness of breath, and fatigue. These are serious symptoms that need immediate medical help.
Venous Occlusion Presentations
Venous occlusions happen when veins get blocked. They have different symptoms than arterial occlusions. Common symptoms include:
- Swelling in the affected limb due to fluid accumulation
- Pain or discomfort, often described as aching or heaviness
- Warmth or redness of the skin over the affected vein
Deep vein thrombosis (DVT) is a big concern in venous occlusions. It can lead to pulmonary embolism if the clot breaks loose.
Emergency Warning Signs of Occlusive Events
Some occlusive events are medical emergencies. They need quick recognition and action. Warning signs include:
- Sudden severe chest pain or discomfort, potentially radiating to the arm, neck, or jaw
- Sudden weakness or numbness in the face, arm, or leg, often on one side of the body
- Difficulty speaking or understanding speech, indicating a possible stroke
- Sudden vision changes, including double vision or loss of vision in one or both eyes
Spotting these emergency signs is key for quick action and possibly saving a life.
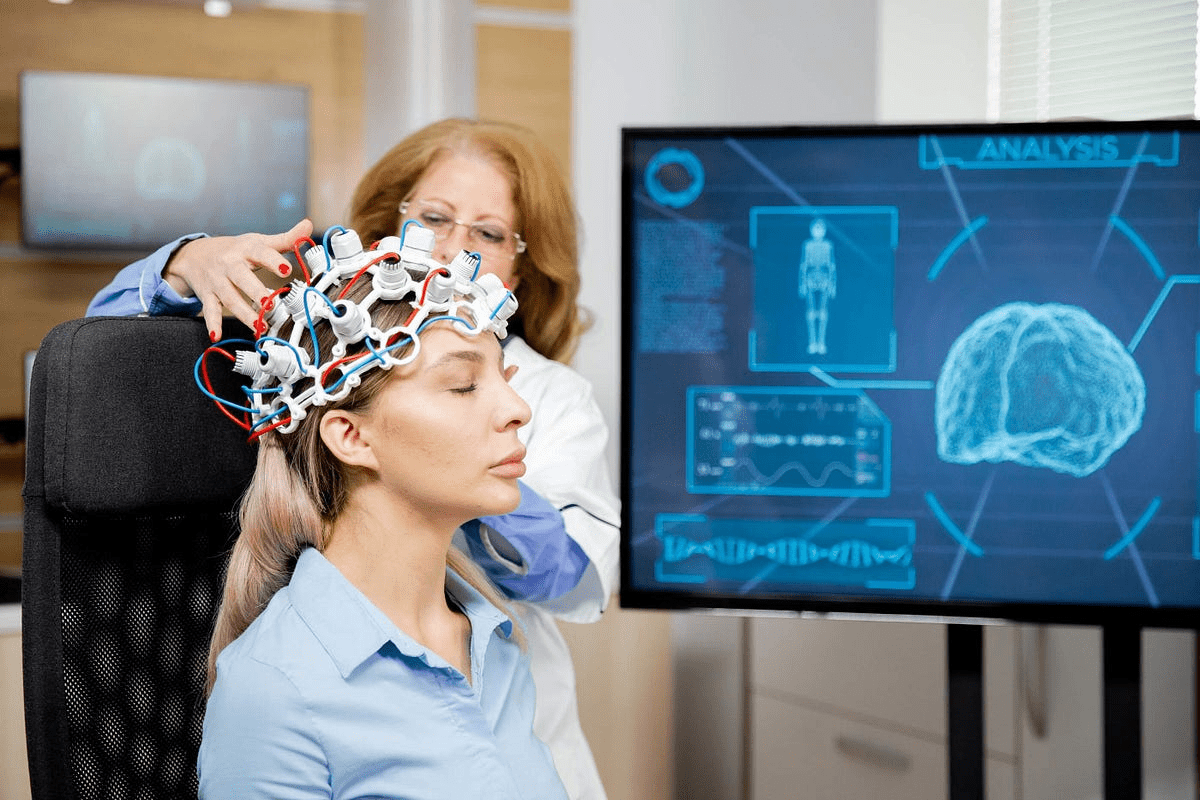
Diagnostic Approaches for Detecting Occlusions
Diagnosing occlusions needs a mix of advanced imaging and lab tests. We use different methods to find occlusions quickly and treat them well.
Non-invasive Imaging Techniques
Non-invasive imaging is key in finding occlusions. Tools like ultrasound, computed tomography (CT) scans, and magnetic resonance imaging (MRI) show the blocked area without surgery.
Ultrasound is great for checking vascular occlusions, like in carotid and peripheral arteries. It shows blood flow and how blocked the area is.
Invasive Diagnostic Procedures
Sometimes, we need to go inside the body to confirm an occlusion. Angiography is one method. It uses a contrast agent to see the blockage on X-ray images.
Coronary angiography is vital for finding blockages in heart arteries. These blockages can cause heart attacks if not treated.
Laboratory Tests and Biomarkers
Laboratory tests and biomarkers help diagnose occlusions. For example, cardiac biomarkers like troponin help spot heart attacks from artery blockages.
Other tests might check for d-dimer to find deep vein thrombosis or pulmonary embolism.
Diagnostic Method | Application | Benefits |
Ultrasound | Vascular occlusions | Non-invasive, provides blood flow information |
CT Scan | Vascular and coronary occlusions | High-resolution images, quick results |
Angiography | Coronary and peripheral artery occlusions | Detailed vascular imaging, guides interventions |
By using these methods together, we can find occlusions accurately. Then, we create treatment plans that fit each patient’s needs.
Treatment Strategies for Occlusive Conditions
Understanding the best ways to treat occlusive conditions is key to better patient care. The right treatment depends on the blockage’s severity and location, and the patient’s health.
There are three main ways to treat occlusive conditions: medicines, interventional procedures, and surgery. Each method has its own benefits and risks, which we’ll explore.
Pharmacological Management
Medicines are often the first step in treating occlusive conditions. These drugs help prevent clots, dissolve them, or manage symptoms.
- Anticoagulants: These prevent new clots and help with deep vein thrombosis.
- Antiplatelet agents: These stop platelets from forming clots and are used for coronary artery disease.
- Thrombolytics: These dissolve clots, used in emergencies like acute ischemic stroke.
For example, in coronary occlusion, aspirin and heparin are used to stop more clots and manage the condition.
Interventional Procedures
Interventional procedures are less invasive ways to open blocked vessels. They’re used when medicines don’t work or the blockage is severe.
Percutaneous coronary intervention (PCI) is a common procedure for coronary artery occlusions. It uses a balloon angioplasty to widen the artery and may include a stent to keep it open.
“Percutaneous coronary intervention has revolutionized the treatment of coronary artery disease, providing a highly effective way to restore blood flow to the heart.”
Medical Expert, Cardiologist
Surgical Approaches for Occlusive Disease
Surgery is considered when other treatments fail. Surgical revascularization is a method to bypass blocked blood vessels, restoring blood flow.
Treatment Option | Description | Indications |
Coronary Artery Bypass Grafting (CABG) | Surgical procedure to bypass blocked coronary arteries | Complex coronary artery disease, failed PCI |
Carotid Endarterectomy | Surgical removal of plaque from the carotid artery | Significant carotid artery stenosis |
Bypass Surgery for Peripheral Artery Disease | Surgical creation of a detour around a blocked peripheral artery | Severe peripheral artery disease |
In conclusion, treating occlusive conditions needs a personalized approach. It considers the occlusion’s specifics and the patient’s health. Knowing the different treatments helps healthcare providers give the best care for patients with occlusive disorders.
Complications and Prognosis of Occlusive Disorders
It’s important to know the complications of occlusive disorders for good patient care. These disorders can cause a lot of harm if not treated right.
Short-term Complications
Short-term problems from occlusive disorders can be very serious. For example, a blockage in the heart’s artery can cause a heart attack. “The timely restoration of blood flow is critical to prevent irreversible damage.” A blockage in the brain’s artery can lead to a stroke, causing sudden brain damage.
These emergencies need quick medical help to avoid lasting harm or death. How severe these problems are can affect how well a patient will do and what treatment they need.
Long-term Sequelae and Disability
People who survive occlusive events often face lasting effects that can change their life a lot. For instance, someone who had a stroke might have brain damage that affects their thinking or movement.
How bad these long-term effects are depends on the severity of the event, how well it was treated, and the person’s health.
Factors Affecting Prognosis and Recovery
The outlook for people with occlusive disorders depends on many things. “The severity of the occlusion, the patient’s age, and the presence of comorbid conditions all play a role in determining outcomes.” How well the treatment works and if the patient follows the treatment plan also matters a lot.
Studies show that people with heart artery disease who get timely and right treatment do better. This includes making lifestyle changes and taking medicine.
“Early intervention and complete management are key to better results for patients with occlusive disorders.”
We know that the outcome for occlusive disorders depends on how bad the condition is and how well it’s treated. By understanding these, doctors can give care that really helps patients.
Conclusion
Understanding occlusion is key in medicine. It helps doctors diagnose and treat many health issues. The term “occlusion medical term” means a blockage in a vessel, organ, or structure in the body.
We’ve looked at the different types of occlusions, their causes, symptoms, and how to treat them. Knowing about occlusion is important for health care.
Occlusive conditions can be very serious if not treated quickly. We talked about how early treatment can greatly help patients. By knowing what occlusive means, doctors can give better care and improve patients’ lives.
In short, understanding medical occlusion is essential for good patient care. Recognizing signs and symptoms and using the right treatments can prevent complications. This improves patient outcomes.
FAQ
What is occlusion in medical terms?
In medicine, occlusion means a blood vessel is blocked. This can be very serious. It happens in places like the heart, brain, and legs.
What is the difference between occlusion and stenosis?
Occlusion is when a blood vessel is completely blocked. Stenosis is when it’s narrowed. Both can slow blood flow. But occlusion is worse and can harm tissues or organs.
What are the causes of vascular occlusions?
Vascular occlusions can come from a few sources. Atherosclerosis, which is hardening of the arteries, is one. Lifestyle choices like smoking and not moving enough also play a part. Genetics can influence the risk too.
What are the symptoms of arterial occlusion?
Symptoms include pain, numbness, and weakness in a limb. If it’s bad, it can cause gangrene or organ failure.
How is occlusion diagnosed?
Doctors use tests like ultrasound and MRI to find occlusions. They might also do angiography. Blood tests help too.
What are the treatment options for occlusive conditions?
Doctors can treat occlusions with medicine, procedures like angioplasty, or surgery. It depends on the case.
What is the prognosis for patients with occlusive disorders?
How well a patient does depends on the severity and treatment. Early action and good health help a lot.
Can occlusive conditions be prevented?
Some risks can’t be changed, but lifestyle choices help. Quitting smoking, exercising, and eating well can lower the risk.
What is the role of platelet aggregation in occlusive events?
Platelet clumps are key in occlusive events. Knowing how they work helps find better treatments.
What are the emergency warning signs of occlusive events?
Look out for sudden chest pain, trouble speaking or swallowing, and severe limb pain or numbness. Get help fast if you see these signs.
References
National Center for Biotechnology Information. Occlusion: Medical Definition of Blocked Blood Vessels. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7028373/