
Did you know millions of people worldwide suffer from blood-related conditions that can be life-threatening if left undiagnosed or untreated? Hematologists play a key role in detecting and managing these conditions. They help diagnose and treat a range of complex blood diseases.
A hematologist is a medical specialist who diagnoses and treats blood-related disorders. Companies like Bristol Myers Squibb lead in developing treatments for these conditions. They advance the field of hematology.
Key Takeaways
- Hematologists diagnose and treat blood-related conditions.
- Bristol Myers Squibb is a leading company in hematology treatments.
- Early detection is key for managing blood diseases.
- Hematology is a complex field requiring specialized knowledge.
- Advances in hematology improve treatment options.
Understanding Hematology and Blood Health
Hematology is the study of blood and its disorders. It’s key to keeping us healthy. It deals with diagnosing, treating, and preventing blood diseases.
What is Hematology?
Hematology is a branch of medicine that studies blood. A hematologist is a doctor who specializes in this field. They help patients with blood problems.
Hematologists can diagnose and treat many blood disorders. This includes anemia, bleeding issues, and blood cancers.
The Importance of Blood Health
Blood health is essential for our well-being. It carries oxygen, fights infections, and keeps tissues healthy. Poor blood health can cause anemia, infections, and bleeding disorders.
Understanding blood health and hematology is vital. It helps us prevent and manage blood diseases.
The Role of a Hematologist in Disease Detection
A hematologist plays a key role in diagnosing and treating blood disorders. Hematologists are medical specialists with deep knowledge in blood-related conditions. They have the skills to handle complex blood issues.
Training and Expertise of Hematologists
Hematologists go through a lot of education and training. They finish medical school, then do a residency in internal medicine. After that, they spend more years in fellowship training in hematology. This prepares them to deal with many blood disorders.
They know how to:
- Read complex lab results to find blood disorders.
- Make treatment plans that fit each patient’s needs.
- Manage both short-term and long-term blood issues.
Common Reasons for Hematology Referrals
There are many reasons why people see a hematologist. These include:
- Unexplained bleeding or bruising.
- Abnormal blood test results that suggest a blood disorder.
- Thoughts of blood cancers like leukemia or lymphoma.
Seeing a hematologist early can really help. It can lead to better diagnosis and treatment, improving health outcomes.
Diagnostic Methods Used by Hematologists
Hematologists use many ways to find and treat blood problems. These methods help us make the right diagnosis and plan the best treatment.
Blood Tests and Analysis
Blood tests are key in hematology. They help us check the blood’s parts, like red and white cells and platelets. This way, we can spot any issues.
Complete Blood Counts (CBCs) are often used to find problems like anemia, infections, or leukemia.
More advanced tests can find specific markers or genetic changes linked to blood diseases. For example, molecular diagnostic tests can find genetic problems in leukemia cells. This helps us make a treatment plan just for you.
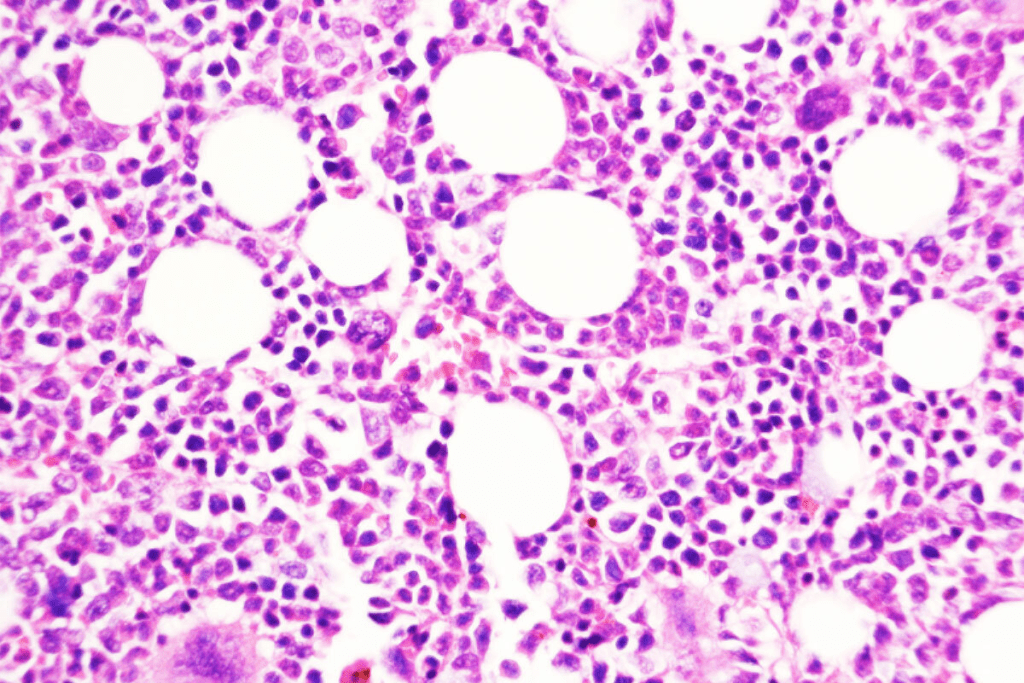
Bone Marrow Examination
Bone marrow tests are very important for diagnosing blood disorders. We take a sample of bone marrow to check how blood cells are made. This helps us find any problems, like cancer cells.
What we learn from these tests helps us understand why you’re sick. It also guides how we should treat you.
Advanced Imaging and Diagnostic Techniques
Advanced imaging is also key in diagnosing and treating blood disorders. Tools like ultrasound, CT scans, and MRI let us see inside the body. This helps us find and understand problems.
These tools are great for finding issues like deep vein thrombosis (DVT). They also help us see how far cancer has spread.
By using all these methods together, we can give accurate diagnoses. Then, we can plan the best treatment for blood disorders.
Common Blood Disorders Detected and Treated by Specialists
It’s key to know about common blood disorders and how specialists treat them. Blood disorders are a big health issue in the United States. They affect millions of people and change their lives.
Overview of Blood Disorder Categories
Blood disorders fall into several types. These include bleeding disorders, clotting disorders, and blood cancers. Bleeding disorders like hemophilia make it hard for blood to clot, causing long bleeding. Clotting disorders lead to blood clots that block blood flow. Blood cancers, like leukemia and lymphoma, mess with blood cell production and can cause serious problems.
Prevalence and Impact in the United States
Blood disorders are common in the United States. Millions of Americans deal with these issues, which strain healthcare and affect their lives. For example, leukemia is a big part of new cancer cases every year. Conditions like deep vein thrombosis (DVT) can be very dangerous if not treated right away.
We need to spread the word about these conditions. This helps catch them early and manage them well. Knowing about blood disorders helps us support patients and doctors in fighting these health issues.
Leukemia: A Major Blood Cancer
Leukemia is a blood cancer that messes with the body’s blood-making process. It happens in the bone marrow, where blood cells are created. Knowing about leukemia helps patients and their families understand diagnosis and treatment.
What is Leukemia?
Leukemia makes too many white blood cells in the bone marrow. This stops normal blood cells from being made. Patients might feel tired, get sick easily, or have bleeding problems.
Leukemia affects blood cell production and causes various symptoms. It messes with the bone marrow, leading to serious problems if not treated quickly.
Types of Leukemia
There are different kinds of leukemia, based on the cells affected and how fast it grows. The main types are:
- Acute Lymphoblastic Leukemia (ALL): A fast-progressing cancer that affects lymphoid cells.
- Chronic Lymphocytic Leukemia (CLL): A slower-progressing cancer that also affects lymphoid cells.
- Acute Myeloid Leukemia (AML): A rapidly progressing cancer that affects myeloid cells.
- Chronic Myeloid Leukemia (CML): A slower-progressing cancer that affects myeloid cells.
Each leukemia type has its own traits and treatment plans. Knowing the exact type is key to finding the right treatment.
| Type of Leukemia | Cell Type Affected | Disease Progression |
| Acute Lymphoblastic Leukemia (ALL) | Lymphoid cells | Fast-progressing |
| Chronic Lymphocytic Leukemia (CLL) | Lymphoid cells | Slow-progressing |
| Acute Myeloid Leukemia (AML) | Myeloid cells | Rapidly progressing |
| Chronic Myeloid Leukemia (CML) | Myeloid cells | Slow-progressing |
Symptoms and Warning Signs of Leukemia
Knowing the symptoms of leukemia is key for early treatment. Leukemia is a blood and bone marrow cancer. It can show symptoms that look like other illnesses, making it hard to spot.
Early Symptoms
In the beginning, leukemia might show signs that seem like other health issues. Early signs include:
- Fatigue: Feeling very tired or weak.
- Weight Loss: Losing weight without trying.
- Fever: Having fevers that don’t have a clear cause.
- Night Sweats: Sweating a lot at night.
These signs are not just for leukemia. But, if they keep happening, you should see a doctor.
Advanced Symptoms
As leukemia gets worse, symptoms get more serious. These include:
- Bone Pain: Feeling pain or tenderness in bones or joints.
- Swollen Lymph Nodes: Lymph nodes getting bigger in the neck, armpits, or groin.
- Enlarged Liver or Spleen: Feeling swollen in the belly because of a big liver or spleen.
- Bleeding or Bruising: Bleeding or bruising easily, like nosebleeds.
These signs mean you need to see a doctor right away.
When to Seek Medical Attention
If you’re feeling symptoms that could be leukemia, get checked out. Catching it early can help a lot.
Here’s a table to help you know when to go to the doctor:
| Symptom | Description | Action |
| Fatigue | Persistent tiredness | Consult a doctor if it lasts more than 2 weeks |
| Bone Pain | Pain or tenderness in bones or joints | Seek medical attention if severe or persistent |
| Unexplained Bleeding | Frequent nosebleeds or easy bruising | Visit a healthcare provider promptly |
Spotting leukemia symptoms and knowing when to see a doctor are key. If you’re worried, talk to a healthcare expert.
Diagnosis and Treatment of Leukemia
Diagnosing leukemia is a journey
with important steps. These steps help decide the best treatment. Accurate diagnosis is key for a good treatment plan.
Diagnostic Process
The first step in diagnosing leukemia is blood tests. Blood tests check for abnormal cell counts. This can show if leukemia is present.
Bone marrow examinations are also vital. They help doctors see how far leukemia has spread. They also figure out the type of leukemia.
- Blood tests to check for abnormal cell counts
- Bone marrow biopsy to assess leukemia cell presence
- Imaging tests to check for any organ damage
Treatment Options
Leukemia treatment varies based on the disease type and stage. Chemotherapy is a common method. It uses drugs to kill leukemia cells.
Other options include:
- Targeted therapy, which targets specific leukemia cell traits
- Immunotherapy, which boosts the immune system against leukemia
- Stem cell transplantation, which replaces damaged bone marrow
We work with patients to find the best treatment. We consider their unique needs and situation.
Hemophilia: A Hereditary Bleeding Disorder
Hemophilia is a condition that affects how blood clots. It leads to prolonged bleeding. This is because the blood can’t clot properly, causing excessive bleeding that can be dangerous.
What is Hemophilia?
Hemophilia is a genetic disorder that makes it hard for blood to clot. It’s usually passed down from parents to their children. The main reason is a gene mutation that affects blood clotting factor proteins.
Normally, when a blood vessel is injured, the body forms a blood clot to stop the bleeding. But in people with hemophilia, this doesn’t happen right. This is because they lack or have low levels of certain clotting factors, leading to prolonged or spontaneous bleeding.
Types of Hemophilia
There are two main types of hemophilia: Hemophilia A and Hemophilia B. Hemophilia A, also known as classic hemophilia, is caused by a deficiency in factor VIII. Hemophilia B, also known as Christmas disease, is caused by a deficiency in factor IX.
- Hemophilia A: This is the most common type, resulting from a deficiency in factor VIII.
- Hemophilia B: Caused by a deficiency in factor IX, it is less common than Hemophilia A.
Both types of hemophilia can lead to similar complications, including joint damage from repeated bleeding into the joints. They can be managed with appropriate treatment.
| Type of Hemophilia | Cause | Clotting Factor Involved |
| Hemophilia A | Deficiency in factor VIII | Factor VIII |
| Hemophilia B | Deficiency in factor IX | Factor IX |
Knowing the type of hemophilia is key to finding the right treatment. Treatment usually involves replacing the missing clotting factor to help the blood clot properly.
“The management of hemophilia has evolved significantly over the years, with the development of recombinant clotting factors and other innovative treatments that have improved the quality of life for individuals with this condition.”
Symptoms and Complications of Hemophilia
It’s important to know the symptoms and complications of hemophilia. This genetic disorder makes it hard for the body to clot blood. It can cause many health problems.
Bleeding Symptoms
The main symptom of hemophilia is prolonged bleeding. This can happen without reason or from small injuries. Bleeding into joints is a big problem, causing pain, swelling, and making it hard to move.
Other symptoms include:
- Nosebleeds that won’t stop
- Bleeding into the skin, causing bruises
- Bleeding into the mouth or gums
- Blood in the urine or stool
The World Federation of Hemophilia says, “Bleeding into joints and muscles can lead to chronic pain and disability if not treated promptly and properly.”
“Early and adequate treatment can significantly reduce the risk of long-term damage.”
Joint Damage and Mobility Issues
Bleeding into joints can cause chronic pain and damage. This can lead to limited mobility and disability. Joint deformity and chronic pain are common, affecting life quality a lot.
Management strategies include physical therapy and sometimes surgery to fix or replace damaged joints.
Internal Bleeding Risks
Internal bleeding is a serious problem with hemophilia. It can be life-threatening if not treated quickly. Bleeding into vital organs like the brain can have severe effects. It can happen on its own or from injury.
| Type of Bleeding | Symptoms | Complications |
| Joint Bleeding | Pain, swelling, limited mobility | Chronic joint pain, disability |
| Internal Bleeding | Variable, depending on location | Life-threatening, organ damage |
| Muscle Bleeding | Pain, swelling | Compartment syndrome, nerve damage |
In conclusion, hemophilia can cause many symptoms and complications. It needs careful management to prevent long-term damage and improve life quality for those affected.
Diagnosis and Management of Hemophilia
Managing hemophilia starts with a correct diagnosis and a treatment plan made just for you. To diagnose hemophilia, we run a series of tests. These tests help us figure out if you have it and how severe it is.
Diagnostic Tests
Tests for hemophilia include blood tests that check clotting factor levels. These tests show if you have hemophilia and how bad it is. We might also do genetic testing to find the cause of the condition.
Blood tests are key in finding out if you have hemophilia. They look at factor VIII or IX levels in your blood. These factors are low in people with hemophilia A or B. The test results tell us how severe your condition is.
Treatment Approaches
Hemophilia treatment has improved a lot. Now, we use recombinant clotting factors to replace what’s missing. We also look at prophylactic treatment to stop bleeding and on-demand treatment for when you bleed.
We make treatment plans just for you. They depend on how bad your hemophilia is, your health history, and your lifestyle. We work with you to create a plan. This includes regular clotting factor infusions, managing bleeding, and physical therapy to keep your joints healthy.
Gene therapy is also being looked at as a treatment for hemophilia. It tries to fix the genetic problem that causes hemophilia. This could be a way to cure it.
Deep Vein Thrombosis (DVT): A Dangerous Blood Clotting Disorder
DVT, or Deep Vein Thrombosis, is when a blood clot forms deep inside the body. It’s a serious health risk that needs quick treatment.
What is DVT?
DVT is a blood clotting disorder in the deep veins of the legs. It can cause pain and swelling. If it breaks loose, it can go to the lungs, which is very dangerous.
Risk Factors for DVT
Several things can make you more likely to get DVT. These include:
- Prolonged Immobility: Long periods without moving, like on long flights or in bed, can cause clots.
- Surgery or Trauma: Surgery or injuries, mainly in the legs or pelvis, can damage veins and raise DVT risk.
- Genetic Predisposition: If your family has a history of blood clotting disorders, you’re more likely to get DVT.
- Cancer: Some cancers can make your blood more likely to clot.
- Obesity: Being overweight or obese can put extra pressure on your leg and pelvis veins.
Knowing these risk factors is key to preventing and catching DVT early. If you’re at risk or have symptoms, see a doctor right away.
Symptoms and Complications of DVT
It’s key to know the symptoms and complications of DVT for early treatment. DVT can cause pain and swelling in the leg. This can really hurt a person’s quality of life.
Recognizing DVT Symptoms
The signs of DVT can differ but often include pain or tenderness in the leg, swelling, and redness or discoloration. Some people might feel warmth or heaviness in their leg. Spotting these signs early is vital to avoid worse problems.
- Pain or tenderness in the leg
- Swelling in the affected limb
- Redness or discoloration
- Warmth or heaviness in the leg
Pulmonary Embolism: A Life-Threatening Complication
Pulmonary embolism (PE) is a serious issue from DVT. It happens when a blood clot moves to the lungs and blocks blood flow. This is a life-threatening problem that needs quick medical help. Signs of PE include shortness of breath, chest pain, and coughing up blood.
Post-Thrombotic Syndrome
Post-thrombotic syndrome (PTS) is another issue from DVT. It leads to chronic pain, swelling, and skin color changes in the affected limb. PTS can really affect a person’s life and may need ongoing care.
We stress the need for early DVT detection and treatment to avoid these problems. Knowing the symptoms and risks of DVT helps patients get help fast. This can lower the chance of serious outcomes.
Diagnosis and Treatment of DVT
Healthcare providers use many tools to diagnose DVT. They do this to start the right treatment. Accurate diagnosis is key to avoiding serious problems and helping patients get better.
Diagnostic Procedures
Several steps are taken to diagnose DVT. Imaging tests are vital to find blood clots. Ultrasound is the most common test for this.
In some cases, venography or CT scans are used too. These help confirm the diagnosis or check for other issues.
Blood tests are also part of the process. They look for clotting disorders or genetic risks for DVT. A detailed medical history and physical exam are also important.
Treatment Options
Treatment for DVT varies based on the patient’s condition and health. The main goal is to stop the clot from getting worse and prevent it from breaking loose.
Anticoagulant medications are the main treatment. They stop new clots and prevent existing ones from growing. In severe cases, thrombolytic therapy might be used to dissolve clots.
For those at high risk, inferior vena cava (IVC) filters might be an option. These filters catch clots before they can travel to the lungs.
Wearing compression stockings is also recommended. They help reduce swelling and prevent long-term problems. Staying active and avoiding long periods of sitting are also key to managing DVT.
Living with Blood Disorders: Quality of Life Considerations
Living with a blood disorder can be tough, but it’s possible to live well. It takes a mix of medical care, lifestyle changes, and emotional support. This approach helps manage the condition effectively.
Coping Strategies
Dealing with a blood disorder means tackling physical and emotional challenges. Stress management techniques like meditation and yoga help. Eating right and exercising regularly also boosts well-being.
Knowing about your condition and treatment options is key. This knowledge lets you make smart choices about your care. It also helps you navigate the healthcare system better.
Support Resources
Having the right support is essential for those with blood disorders. This includes doctors, support groups, counseling, and online resources. Support groups are great for sharing experiences and learning from others.
Family and friends are also important. Teaching them about your condition helps them support you better. They can understand your needs more clearly.
Long-term Management
Managing blood disorders long-term means ongoing medical care. Regular visits to healthcare providers are key. They help adjust treatment plans and catch problems early.
Being proactive is also important. Stick to your treatment plan, watch for symptoms, and make lifestyle changes. This helps avoid complications.
By managing your condition well, you can improve your quality of life. You can lead an active and fulfilling life despite the challenges.
Conclusion
We’ve looked at how important hematologists are in finding and treating blood disorders. This includes leukemia, hemophilia, and deep vein thrombosis. These doctors are key in helping millions of people worldwide.
Hematologists are experts at reading blood tests and creating treatment plans. They help patients understand their conditions better. This knowledge improves patients’ lives and health.
In summary, hematologists are vital in the battle against blood disorders. Their work saves lives and improves health. If you think you have a blood disorder, see a hematologist right away.
FAQ
What is hematology?
Hematology is a part of medicine that focuses on blood and blood-related issues. It aims to diagnose, treat, and prevent blood disorders.
What is a hematologist?
A hematologist is a doctor who specializes in blood disorders. They handle bleeding issues and blood cancers.
What are the common blood disorders detected and treated by hematologists?
Hematologists deal with conditions like leukemia, hemophilia, and deep vein thrombosis (DVT).
What is leukemia?
Leukemia is a blood cancer that affects the blood and bone marrow. It’s marked by abnormal white blood cells.
What are the symptoms of leukemia?
Symptoms include fatigue, weight loss, frequent infections, and easy bleeding or bruising. If these last, see a doctor.
What is hemophilia?
Hemophilia is a bleeding disorder that makes blood clotting hard. It leads to prolonged bleeding and can damage joints.
What is deep vein thrombosis (DVT)?
DVT is a blood clotting disorder in deep veins, often in the legs. It’s dangerous if the clot moves to the lungs.
What are the risk factors for DVT?
Risk factors include immobility, surgery, cancer, and genetic blood clotting issues.
How are blood disorders diagnosed?
Tests like blood tests, bone marrow exams, and imaging help diagnose blood disorders.
What are the treatment options for blood disorders?
Treatments vary by condition and severity. They include medication, surgery, and lifestyle changes.
How can individuals cope with blood disorders?
Living with blood disorders means adopting healthy habits, seeking support, and using resources and support groups.
What is the importance of quality of life considerations for individuals living with blood disorders?
Quality of life is key for those with blood disorders. It affects their well-being and managing their condition.
References
https://www.ncbi.nlm.nih.gov/books/NBK593683
National Center for Biotechnology Information (NCBI). (2023, April 30). Techniques for hematological disorders.










