
blood thinners for afib
Atrial fibrillation (AFib) is a heart condition that affects millions worldwide. It significantly increases the risk of stroke. Doctors often prescribe anticoagulants, like Eliquis (Apixaban), to prevent blood clots.
For patients who have ablation, a procedure to fix a normal heart rhythm, a question comes up. How long should one stay on Eliquis or other atrial fibrillation medications? The time needed on anticoagulant therapy after ablation is key. It helps lower stroke risk while looking at the patient’s overall health.
Key Takeaways
- The use of anticoagulants like Eliquis is crucial for managing stroke risk in AFib patients.
- Ablation is a procedure to correct irregular heart rhythms, but the need for anticoagulants may persist post-procedure.
- The duration of Eliquis treatment after ablation depends on individual patient risk factors.
- Doctors assess the risk of stroke and bleeding to determine the appropriate duration of anticoagulant therapy.
- Patient health and medical history play a significant role in deciding the continuation of Eliquis.
Understanding Cardiac Ablation for Atrial Fibrillation

cardiac ablation procedure
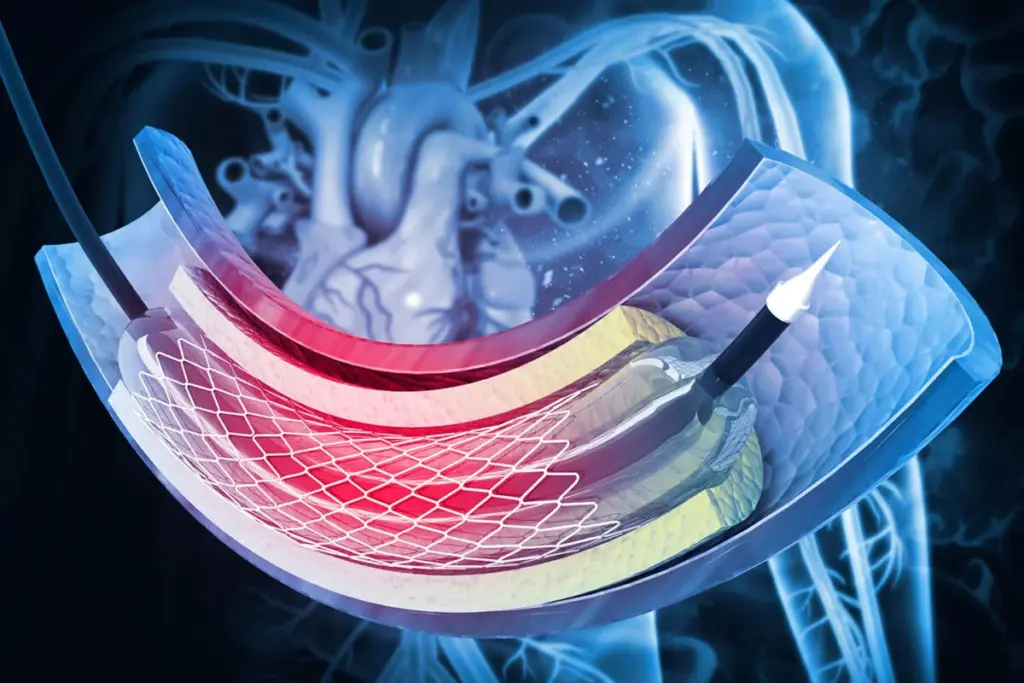
Cardiac ablation is changing how we treat atrial fibrillation. It’s a key treatment for AFib, offering a chance for a cure.
What is Cardiac Ablation?
Cardiac ablation uses energy to destroy abnormal heart pathways. It aims to fix the heart’s rhythm. This improves symptoms and life quality for AFib patients.
Types of Ablation Procedures
There are different cardiac ablation procedures:
- Radiofrequency ablation uses heat to destroy tissue.
- Cryoballoon ablation uses cold to do the same.
- Laser ablation is less common but also works.
Doctors choose the best method based on the patient’s condition and their own experience.
Success Rates and Expectations
Success in cardiac ablation depends on several things. These include the type of AFib, how long it lasts, and any heart disease.
|
Type of AFib |
Success Rate |
|---|---|
|
Paroxysmal AFib |
70-80% |
|
Persistent AFib |
50-70% |
Knowing these factors helps set realistic hopes for patients getting cardiac ablation.
The Risk of Blood Clots After Ablation
blood clots after cardiac ablation
Cardiac ablation for atrial fibrillation (AFib) raises concerns about blood clots. This procedure is effective but carries a risk of blood clots. It’s important to manage this risk carefully.
We will look into why blood clots form after the procedure. We’ll also discuss the stroke risk and what increases clotting risk.
Why Blood Clots Form Post-Procedure
AFib causes the heart to beat too fast and weakly. This slows down the heart’s pumping. Blood can pool in the heart’s upper chamber, leading to clot formation.
Blood clots are a serious complication. They can break loose, travel to the brain, and cause a stroke.
Stroke Risk Following Ablation
The risk of stroke after cardiac ablation is a big concern. Blood clots can form and dislodge, posing a risk. Studies show the risk is highest right after the procedure.
Monitoring and anticoagulation therapy are key to reducing this risk.
Factors That Increase Clotting Risk
Several factors can raise the risk of clotting after cardiac ablation. These include a history of stroke or TIA, high blood pressure, diabetes, and heart failure.
Knowing these risk factors is crucial. It helps in managing and reducing the risk of blood clot formation.
Introduction to Eliquis (Apixaban)
Eliquis Mechanism of Action
Eliquis (Apixaban) is a top choice for treating AFib after cardiac ablation. We’ll look at its role, how it works, and how it compares to other anticoagulants.
How Eliquis Works
Eliquis (Apixaban) is a direct oral anticoagulant (DOAC). It stops blood clots by blocking Factor Xa, a key protein. This reduces stroke and embolism risks in AFib patients.
Its action is precise, targeting Factor Xa. This makes Eliquis effective and easy to use for patients.
Eliquis vs. Traditional Anticoagulants
Eliquis beats traditional anticoagulants like warfarin in many ways. It’s more predictable and doesn’t need blood tests. It also has a lower risk of bleeding.
Here’s a comparison of Eliquis and warfarin:
|
Characteristics |
Eliquis (Apixaban) |
Warfarin |
|---|---|---|
|
Monitoring Required |
No |
Yes |
|
Dosing Frequency |
Twice daily |
Variable, based on INR |
|
Bleeding Risk |
Lower |
Higher |
|
Dietary Restrictions |
No |
Yes |
Dosing Guidelines for Atrial Fibrillation Patients
For AFib patients, Eliquis is taken orally twice a day. The dose is 5 mg. For older patients or those with lower body weight, it’s 2.5 mg twice daily.
Following the dose is key to Eliquis’s success and safety.
Blood Thinners for AFib: Options and Comparisons
blood thinners comparison
Blood thinners are key in lowering stroke risk for AFib patients. The right choice depends on how well they work, their safety, and the patient’s health.
Direct Oral Anticoagulants (DOACs)
DOACs, like Eliquis (apixaban), are popular for AFib treatment. They block thrombin or Factor Xa, important in blood clotting.
- Advantages: They lower stroke risk and have fewer bleeding issues than older meds. No need for regular blood tests.
- Examples: Eliquis (apixaban), Xarelto (rivaroxaban), Pradaxa (dabigatran).
Vitamin K Antagonists (Warfarin)
Warfarin has been around for decades to manage AFib and prevent stroke. It stops Vitamin K-dependent clotting factors in the liver.
- Advantages: It’s good at preventing stroke and has a lot of experience behind it.
- Disadvantages: Needs regular blood tests, has diet limits, and can cause more bleeding.
Comparing Effectiveness and Safety Profiles
- Effectiveness: DOACs are as good as warfarin at stopping strokes.
- Safety: They have a lower risk of serious bleeding.
But, picking between DOACs and warfarin depends on the patient’s health. This includes kidney function, bleeding risk, and other meds they take.
Standard Recommendations for Anticoagulation Duration After Ablation
anticoagulation duration after ablation
Figuring out how long to take anticoagulants like Eliquis (apixaban) after cardiac ablation is key. It depends on your stroke risk, bleeding risk, and how well the ablation worked. These factors are important for managing atrial fibrillation (AFib) well.
Guidelines help doctors make the right choice for anticoagulation therapy. They’re based on studies and expert opinions.
Current Clinical Guidelines
Guidelines say patients should keep taking anticoagulants for 2-3 months after ablation. This helps lower the risk of stroke and other blood clots during this time.
The Minimum 2-3 Month Period
The first 2-3 months are very important. The risk of stroke is still high because the blood vessels might not fully heal right away. There’s also a chance of temporary heart problems.
Variations Based on Medical Society Recommendations
Medical societies might suggest different times for stopping anticoagulants. This depends on the patient’s CHA₂DS₂-VASc score, if arrhythmias come back, or their bleeding risk. Each case is different.
|
Guideline |
Recommended Anticoagulation Duration |
Key Considerations |
|---|---|---|
|
ACC/AHA/Heart Rhythm Society |
At least 2-3 months post-ablation |
Stroke risk, bleeding risk, procedural success |
|
European Heart Rhythm Association |
Minimum 2-3 months; consider longer duration based on individual risk |
CHA₂DS₂-VASc score, presence of comorbidities |
These guidelines stress the need for personalized care. They consider each patient’s unique situation. By following these, doctors can find the right balance for anticoagulation therapy after cardiac ablation.
Factors That Influence How Long to Stay on Eliquis
Eliquis duration factors
Deciding how long to take Eliquis after a heart procedure is important. Doctors look at several things to make sure patients get the best care. This helps patients stay safe and healthy.
CHA₂DS₂-VASc Score and Stroke Risk
The CHA₂DS₂-VASc score helps doctors figure out stroke risk in patients with atrial fibrillation. It considers things like heart failure, high blood pressure, age, diabetes, and more. A higher score means a higher stroke risk, which affects Eliquis treatment.
|
CHA₂DS₂-VASc Score |
Stroke Risk |
Recommendation |
|---|---|---|
|
0-1 |
Low |
Consider stopping Eliquis after successful ablation |
|
2 or more |
Moderate to High |
Likely to continue Eliquis |
Presence of Recurrent Arrhythmias
Recurring heart rhythm problems after ablation are key. If a patient keeps getting atrial fibrillation, they’re at higher risk for stroke. This means they might need to keep taking Eliquis.
Monitoring for recurrent arrhythmias is important. Doctors will check in regularly and might use tests like Holter monitoring. This helps catch any heart rhythm issues early.
Individual Bleeding Risk Assessment
It’s also crucial to think about bleeding risk when deciding on Eliquis treatment. Things like age, past bleeding, kidney health, and other medicines can raise this risk.
Careful consideration of these factors helps doctors weigh the benefits of Eliquis against the risks. This way, they can make the best choice for each patient.
Timeline Scenarios for Eliquis After Ablation
Eliquis treatment duration scenarios
The time you take Eliquis after cardiac ablation can change a lot. It depends on many things about you. We’ll look at the different times you might take Eliquis, from short to long-term or even for life.
Short-Term (2-3 Months) Therapy
Some people might only need Eliquis for a short time. This is if they’re at low risk for stroke and haven’t had AFib come back often.
- Low CHA₂DS₂-VASc score
- Successful ablation with no complications
- Absence of recurrent arrhythmias
Medium-Term (3-12 Months) Therapy
Those at a bit higher risk might need Eliquis for a few years.
- Moderate CHA₂DS₂-VASc score
- Presence of some risk factors for stroke
- Ongoing monitoring for AFib recurrence
Long-Term or Lifelong Therapy Indications
Those at very high risk or with AFib coming back might need Eliquis forever.
- High CHA₂DS₂-VASc score
- History of stroke or transient ischemic attack (TIA)
- Persistent or recurrent AFib
In conclusion, how long you take Eliquis after ablation depends a lot on you. It looks at your risk factors, how well the ablation worked, and if AFib comes back. Doctors use this to decide how long you should take Eliquis.
Monitoring Effectiveness During Eliquis Therapy
It’s important to watch how Eliquis works after a heart procedure. Regular tests help see if the treatment is working right. We’ll talk about how to check Eliquis therapy, including tests, signs of success, and when to see a doctor.
Follow-up Testing After Ablation
After a heart procedure, it’s key to check Eliquis therapy. This might include:
- Regular blood tests to check for signs of bleeding or clotting
- Electrocardiograms (ECGs) to monitor heart rhythm
- Imaging tests to assess cardiac function
These tests help your doctor see if the Eliquis dose is right. They might need to change it.
Signs That Anticoagulation Is Working
Good Eliquis therapy should lower the risk of blood clots and stroke. Look for these signs:
- Absence of stroke or transient ischemic attack (TIA) symptoms
- No evidence of blood clots on imaging tests
- Stable or improved cardiac function
If you notice anything odd, talk to your doctor right away.
When to Consult Your Doctor About Adjustments
If you see any of these, talk to your doctor about changing your Eliquis therapy:
- Signs of bleeding, such as bruising, nosebleeds, or heavy menstrual bleeding
- Symptoms of stroke or TIA, such as weakness, numbness, or difficulty speaking
- Changes in kidney function or other health conditions that may affect Eliquis dosing
Your doctor will look at your situation and suggest changes if needed.
Managing Side Effects and Daily Life on Eliquis
Living with Eliquis is more than just taking medicine. It’s about managing side effects well. Knowing the side effects and how to deal with them is key.
Common Side Effects to Expect
Eliquis can cause common side effects. These include:
- Bleeding, from small bruises to serious hemorrhages
- Nosebleeds that can be hard to stop
- Bruising even with minor injuries
Knowing these side effects helps patients prevent them and get help when needed.
Serious Side Effects Requiring Medical Attention
Though rare, serious side effects can happen. These include:
- Life-threatening bleeding that needs quick medical help
- Allergic reactions like rash, itching, or trouble breathing
It’s crucial to know these serious side effects and get medical help right away.
Practical Tips for Daily Living While on Anticoagulants
Here are some tips for daily life on Eliquis:
- Use a soft-bristled toothbrush and gentle flossing to avoid gum bleeding.
- Stay away from contact sports and activities that could hurt you.
- Be careful with sharp objects like razors or knives.
Following these tips can help lower the risk of bleeding problems.
|
Side Effect |
Prevention Tips |
|---|---|
|
Bleeding |
Avoid sharp objects, use gentle oral care |
|
Nosebleeds |
Use saline nasal sprays, avoid picking nose |
|
Bruising |
Wear protective clothing, avoid tight clothing |
Medication Interactions and Lifestyle Considerations
To get the most out of Eliquis, it’s important to know how it works with other medicines and lifestyle choices.
Foods and Supplements That Interact with Eliquis
Some foods and supplements can affect Eliquis, making it less effective or raising the chance of bleeding. Eating a lot of green leafy veggies, like spinach, can lessen Eliquis’s effect. But, it’s still key to eat the same foods every day to keep the medicine working right.
Supplements that might make bleeding more likely with Eliquis include:
- Fish oil supplements, because they slow down blood clotting
- Ginkgo biloba, which also affects blood clotting
- Vitamin E in big doses, as it might act like a blood thinner
Other Medications to Avoid
It’s crucial to watch out for other medicines that could mess with Eliquis. These might make bleeding more likely or make Eliquis less effective. Some of these include:
|
Medication Category |
Examples |
Potential Interaction |
|---|---|---|
|
Antiplatelet drugs |
Aspirin, clopidogrel |
Increased risk of bleeding |
|
Nonsteroidal anti-inflammatory drugs (NSAIDs) |
Ibuprofen, naproxen |
Increased risk of bleeding |
|
Certain antifungal medications |
Ketoconazole, itraconazole |
Potential increase in Eliquis levels |
Activity and Exercise Recommendations
Staying active is good for patients on Eliquis, as it helps heart health. But, there are some things to watch out for to avoid injuries or bleeding:
General Recommendations:
- Avoid sports or activities that could cause injuries
- Wear protective gear in activities that might hurt you
- Be careful with sharp objects or tools
Knowing about Eliquis’s interactions with other things and living a safe, healthy life can help patients get the most from their treatment. This way, they can enjoy the benefits of Eliquis while staying safe.
What Happens If AFib Recurs After Ablation
AFib coming back after ablation raises big questions about keeping up with blood thinners. It’s key for both patients and doctors to understand what happens next.
Detecting AFib Recurrence
Spotting AFib coming back means watching for symptoms and doing tests. Symptoms like palpitations, shortness of breath, or feeling tired might mean AFib is back. Doctors usually suggest ECGs or Holter monitoring to catch any rhythm problems.
“The key to managing AFib recurrence lies in early detection and prompt intervention,” a top cardiology expert says.
How Recurrence Affects Anticoagulation Decisions
AFib coming back after ablation changes how we think about blood thinners. Doctors might keep or start blood thinners like Eliquis to lower stroke risk.
- Using tools like the CHA₂DS₂-VASc score to check stroke risk.
- Looking at the patient’s health and risk of bleeding.
- Thinking about what the patient wants and their quality of life.
Options for Managing Recurring AFib
Dealing with recurring AFib needs a plan that fits each person. Repeat ablation procedures might be an option. Changing medicines, like blood thinners and heart rhythm drugs, is also common.
Handling recurring AFib means looking at each person’s unique situation. This includes their medical history, what they prefer, and their specific condition.
The Discontinuation Process: Safely Stopping Eliquis
Stopping Eliquis therapy needs a careful look at the patient’s health. It’s important to avoid stroke risks when stopping Eliquis after a heart procedure. We’ll help you understand how to prepare, monitor, and know when to start therapy again.
Preparing to Stop Anticoagulation
Before stopping Eliquis, check the risk of stroke and blood clots. Look at the patient’s CHA₂DS₂-VASc score and bleeding risk. Those at higher stroke risk might need to keep taking Eliquis.
Monitoring After Discontinuation
Watch for stroke or blood clot signs after stopping Eliquis. Regular doctor visits are key. Look out for sudden weakness, confusion, or trouble speaking.
|
Monitoring Period |
Recommended Actions |
|---|---|
|
First Week |
Check for signs of bleeding or thromboembolic events |
|
1-3 Months |
Regular follow-up appointments to assess stroke risk |
|
After 3 Months |
Continue monitoring for signs of AFib recurrence |
Signs That Warrant Resuming Therapy
If you feel palpitations, shortness of breath, or chest pain after stopping Eliquis, get help fast. Starting therapy again might be needed to prevent stroke or other problems.
Stopping Eliquis safely means being ready, watching closely, and knowing when to start therapy again. Working with doctors helps reduce risks when stopping anticoagulation therapy.
Shared Decision-Making with Your Healthcare Team
Your healthcare team is key in managing anticoagulation therapy after ablation. They help you navigate the complex world of atrial fibrillation. This is done by considering your unique needs, preferences, and medical history.
Questions to Ask Your Electrophysiologist
It’s important to have open discussions with your electrophysiologist. Ask them questions like:
- What are the specific risks and benefits associated with continuing or stopping anticoagulation therapy in my case?
- How will my CHA₂DS₂-VASc score influence my anticoagulation treatment plan?
- What are the signs and symptoms I should watch for that may indicate a need to adjust my therapy?
The American Heart Association stresses the importance of patient engagement and education in managing atrial fibrillation.
“Patients who are actively involved in their care tend to have better health outcomes.”
Balancing Quality of Life with Safety
Managing anticoagulation therapy involves balancing stroke risk and quality of life. Your healthcare team can help you understand the benefits and risks of different treatments.
|
Consideration |
Factors to Evaluate |
|---|---|
|
Stroke Risk |
CHA₂DS₂-VASc score, history of stroke or TIA |
|
Bleeding Risk |
HAS-BLED score, history of bleeding events |
|
Quality of Life |
Lifestyle factors, medication adherence, potential side effects |
Creating a Personalized Anticoagulation Plan
A personalized anticoagulation plan considers your unique risk factors, medical history, and preferences. Working with your healthcare team, you can create a plan that fits your needs.
As we work together on anticoagulation therapy, it’s crucial to regularly review and adjust your plan. This ensures you receive the best and safest care.
Conclusion: Making Informed Decisions About Your Anticoagulation Therapy
As we wrap up our talk on managing atrial fibrillation (AFib) with anticoagulation therapy, it’s clear that making smart choices is key. Knowing how anticoagulants like Eliquis (apixaban) work and how long they last is very important.
We’ve looked at the good and bad sides of anticoagulation therapy. We’ve seen why it’s important to keep an eye on things and why a plan that fits you is best. By thinking about your own risks and health, you can work with your doctor to find the right treatment for you.
Being informed about your anticoagulation therapy lets you take charge of your AFib care. By staying up to date and working with your healthcare team, you can get the best results and live a better life.
FAQ
What is cardiac ablation and how does it relate to AFib management?
Cardiac ablation is a procedure that uses energy to destroy abnormal heart pathways. It aims to fix the heart rhythm in AFib patients. This can reduce symptoms and improve life quality.
Why are blood thinners necessary after cardiac ablation?
Blood thinners prevent blood clots after ablation. This is crucial to avoid strokes, especially in AFib patients.
How does Eliquis (Apixaban) work as an anticoagulant?
Eliquis stops blood clotting by blocking Factor Xa. This lowers stroke risk in AFib patients.
What are the advantages of Eliquis over traditional anticoagulants like warfarin?
Eliquis has a more stable effect, fewer diet rules, and less need for blood tests. It also has a lower risk of bleeding than warfarin.
How long should I stay on Eliquis after ablation?
Eliquis treatment time varies based on your health and risk factors. Your doctor will decide based on your condition.
What factors influence the decision to continue or stop Eliquis therapy?
Decisions are based on ablation success, AFib recurrence, and stroke risk. Regular check-ups with your doctor are key.
Can I stop taking Eliquis if my AFib is cured after ablation?
Stopping Eliquis should be discussed with your doctor. They will consider your overall health and stroke risk.
How will I know if Eliquis is working effectively?
Look for no strokes or clots. Regular tests as advised by your doctor will show if Eliquis is working.
What are the common side effects of Eliquis, and how can they be managed?
Side effects include bleeding and bruising. Report any issues to your doctor. They can adjust your treatment as needed.
Are there any foods, supplements, or medications that interact with Eliquis?
Some drugs and supplements can affect Eliquis. Tell your doctor about any you’re taking to avoid problems.
How does AFib recurrence after ablation affect my anticoagulation therapy?
If AFib comes back, your doctor may change your treatment. They’ll consider your stroke risk and other factors.
What is the process for safely discontinuing Eliquis?
Stopping Eliquis should be done with your doctor’s guidance. They’ll watch for clotting or AFib signs after stopping.
How can I create a personalized anticoagulation plan with my healthcare team?
Talk about your health, risks, and lifestyle with your doctor. This ensures your treatment fits your needs.
Reference
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/28777364/








