Last Updated on November 13, 2025 by
Recent advances in transfusion medicine for kids have set clear hemoglobin levels. These levels balance safety and outcomes for children. It’s key to find the right hemoglobin level for transfusion in pediatric care.

The TRIPICU study suggests a restrictive transfusion strategy. It recommends a threshold of 7 g/dL for stable kids. This guideline is widely followed, making sure kids get transfusions only when needed and reducing risks.
At top hospitals like LivHospital, these rules are followed closely. They aim for high-quality care and keep improving in every transfusion decision for kids.
Key Takeaways
- Pediatric hemoglobin thresholds for transfusion vary based on clinical condition.
- A general threshold of 7 g/dL is recommended for hemodynamically stable patients.
- The TRIPICU study supports a restrictive transfusion strategy.
- Evidence-based protocols ensure high-quality care in pediatric transfusion decisions.
- Leading hospitals consistently apply these guidelines to improve patient outcomes.
Understanding and Blood Transfusion Definition
Hemoglobin is key in delivering oxygen to our bodies. It’s a protein in red blood cells. In kids, knowing their hemoglobin levels helps decide if they need a blood transfusion.

The Critical Role of Hemoglobin in Pediatric Health
Hemoglobin is vital for kids’ health. It makes sure tissues and organs get enough oxygen. Low hemoglobin, or anemia, can cause fatigue, weakness, and slow growth.
In serious cases, anemia might need a blood transfusion. This helps tissues get more oxygen.
Deciding to transfuse blood is a big decision. It’s based on the child’s health, hemoglobin level, and symptoms of low oxygen.
How Hemoglobin Levels Are Measured and Interpreted in Children
Kids’ hemoglobin levels are checked with a complete blood count (CBC) test. This test looks at all parts of blood, including hemoglobin. It’s important to consider the child’s age when looking at these levels.
For example, babies have higher hemoglobin levels than older kids. Knowing this helps doctors understand hemoglobin levels better. It helps them decide if a blood transfusion is needed.
Healthcare providers look at hemoglobin levels and the child’s overall health. This helps them decide when a blood transfusion is necessary for kids.
The 7 g/dL Threshold: Standard Guideline for Stable Pediatric Patients
Recent studies, like the TRIPICU trial, have confirmed the 7 g/dL hemoglobin threshold as key for transfusions in stable kids. This level is part of a careful approach to transfusions. It aims to cut down on unnecessary transfusions and their risks.

Evidence Supporting the Restrictive Transfusion Approach
The 7 g/dL threshold for transfusions is backed by strong evidence. Research shows it lowers transfusion numbers without raising risks in stable kids.
The TRIPICU study is a major piece of evidence. It’s a big trial that looked at liberal versus restrictive transfusion in sick kids. It found that being more careful with transfusions cuts down on them. But it doesn’t harm the kids’ health.
“The TRIPICU study showed that being careful with transfusions is just as safe as being more liberal in sick kids. It lowers the need for red blood cell transfusions.”
Key Studies That Established the 7 g/dL Benchmark
Many studies have helped set the 7 g/dL benchmark for transfusions in kids. These include:
- The TRIPICU study proved the safety and success of careful transfusion strategies.
- Observational studies that linked hemoglobin levels to outcomes in kids.
- Meta-analyses that combined data from various studies to confirm the 7 g/dL threshold.
Together, these studies support using a 7 g/dL hemoglobin threshold for transfusions in stable kids. They help find the right balance between enough oxygen and the risks of blood transfusions.
When Higher Hemoglobin Thresholds Are Necessary
For stable kids, a hemoglobin level of 7 g/dL is usually okay. But some kids need more because of their health issues. This includes kids who are very sick, have heart problems, or have had a bone marrow transplant.
Critically Ill Children: 8-10 g/dL Threshold
Kids who are very sick need more hemoglobin, usually 8-10 g/dL. They need more oxygen because they are very sick. They might have sepsis or other serious problems that affect how well their body gets oxygen.
Keeping their hemoglobin higher helps make sure they get enough oxygen to their body.
Congenital Heart Disease Patients: 9-13 g/dL Threshold
Kids with heart problems might need even more hemoglobin, from 9-13 g/dL. The type of heart problem they have affects how much hemoglobin they need. For example, kids with certain heart defects might need more hemoglobin to carry enough oxygen.

Post-Hematopoietic Stem Cell Transplant: 8-9 g/dL Threshold
After a bone marrow transplant, kids need 8-9 g/dL of hemoglobin. They are at risk for serious problems like graft-versus-host disease and infections. Keeping their hemoglobin levels right is key to helping them get better and avoid bad outcomes.
In short, while most kids need 7 g/dL of hemoglobin, some need more. Knowing this helps doctors decide when to give blood transfusions. This can really help kids get better.
5 Clinical Signs That Indicate Need for Transfusion Despite Hemoglobin Level
When deciding if a blood transfusion is needed in kids, doctors look at more than just hemoglobin levels. They also check for clinical signs. These signs can show that a transfusion is needed, even if the hemoglobin level is okay. Let’s look at these important signs that help doctors decide on transfusions for kids.
Tachycardia and Hemodynamic Instability
An elevated heart rate, or tachycardia, is a key sign. It means the heart is working harder because of low oxygen. This could mean the hemoglobin level is too low. Also, if blood pressure keeps changing, it’s a sign that a transfusion is needed to keep tissues oxygenated.
Respiratory Distress and Increased Oxygen Requirements
Signs like fast breathing, retractions, or grunting show the body is struggling to get enough oxygen. If a child needs more oxygen, it’s a big sign. These signs mean the current hemoglobin level might not be enough, so a transfusion might be needed.
Lethargy and Altered Mental Status
Lethargy or changes in mental status can mean the brain isn’t getting enough oxygen. If the hemoglobin level is too low, it can cause these problems. This is a serious sign that might mean a transfusion is needed, even if other signs aren’t bad.
Persistent Lactic Acidosis
Lactic acidosis that doesn’t go away is a sign of not enough oxygen in the body. High lactate levels mean the current hemoglobin level is not enough. This could mean a blood transfusion is needed to get more oxygen to the tissues and fix the acidosis.
These signs show why a full check-up is key when deciding on blood transfusions for kids. By looking at both hemoglobin levels and clinical signs, doctors can make the best choices for their patients.
Beyond Numbers: Key Factors That Influence Transfusion Decisions
Blood transfusions in kids are more than just numbers. We look at many factors to understand a child’s health fully. This helps us decide if a transfusion is needed.
Assessing Tissue Oxygenation in Pediatric Patients
Checking if tissues get enough oxygen is key. This ensures organs work properly. Tissue oxygenation is vital for a child’s health.
We check oxygen levels through different signs. These include:
- Heart rate and blood pressure monitoring
- Lactate levels, which show if tissues are getting enough oxygen
- Mixed venous oxygen saturation (SvO2)
These signs help us see if a child needs a transfusion.
Consideration of Underlying Pathology
The patient’s underlying condition also matters. Different diseases affect transfusion needs differently. For example, kids with congenital heart disease might need more blood.
Here are some conditions we look at:
- Congenital heart disease, which may require higher hemoglobin thresholds
- Critical illness, where the patient’s condition can rapidly evolve
- Post-hematopoietic stem cell transplant, where transfusion needs can be complex
Knowing the patient’s condition helps us choose the right transfusion. Clinical guidelines agree that the condition is key to a good transfusion plan.
“The decision to transfuse must be based on a complete look at the patient’s health, including their underlying condition and current state.”
By looking at oxygen levels and the patient’s condition, we make better transfusion choices. This helps kids get better faster.
Risks vs. Benefits: Why Transfusion Thresholds Matter
Deciding to give blood to kids is a careful choice. It’s about finding the right balance. Transfusion thresholds help make sure blood is given when it’s really needed. This way, we avoid risks that aren’t necessary.
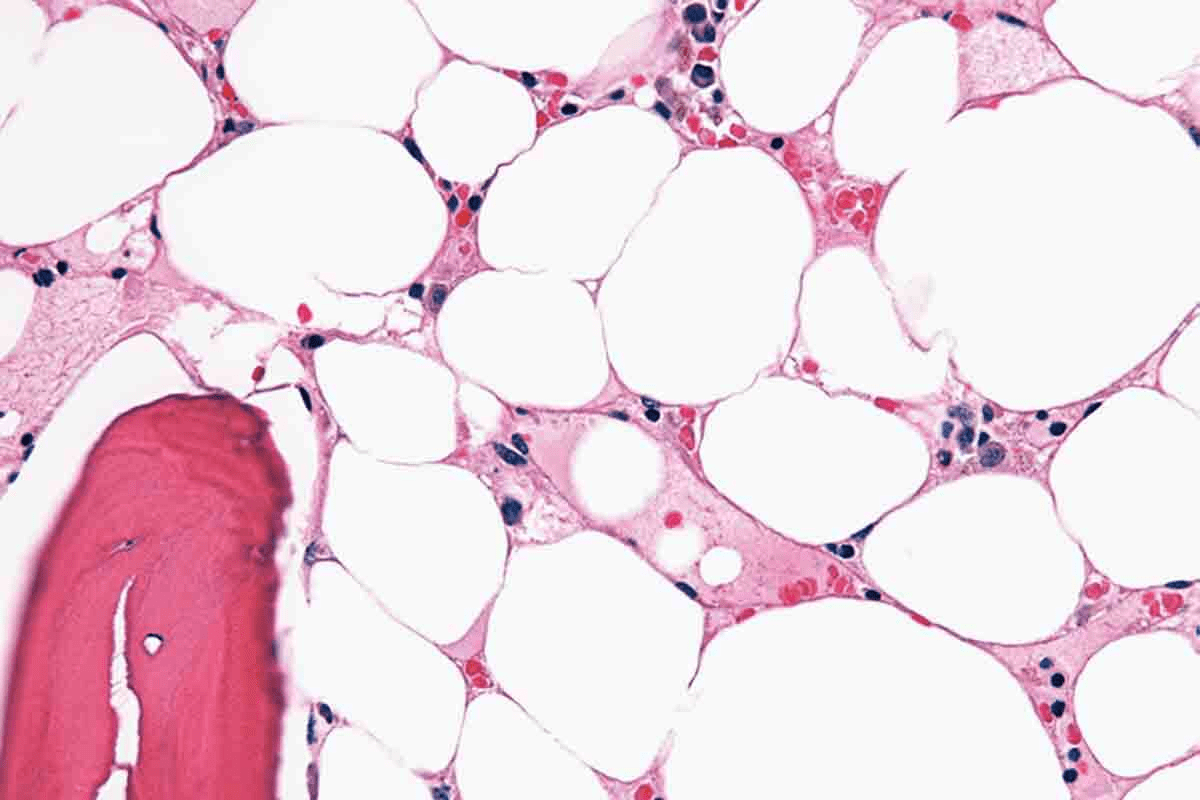
Potential Complications of Unnecessary Transfusions
Too many blood transfusions can harm kids. They might get lung problems, heart issues, or even infections. Also, getting blood too often can lead to iron overload, which is very bad.
Too much blood can also weaken the immune system. This makes kids more likely to get sick. It might even make cancer come back in some cases. So, it’s key to follow the right rules for giving blood.
Benefits of Appropriate Transfusion Timing
But giving blood at the right time can really help kids. It keeps their blood healthy, helping their bodies work better. This is good for their recovery and helps their organs function well.
In very sick kids, blood transfusions can be a lifesaver. They help keep the heart and lungs working right. They also prevent problems like tiredness and slow growth in kids.
Healthcare teams need to think carefully about when to give blood. They should follow the rules for transfusions. This way, kids get the blood they need without facing too many risks. It’s all about giving the best care possible to each child.
Practical Implementation: Blood Infusion Rates and Monitoring Protocols
When we give blood transfusions to kids, we have to think about how fast to give it and how to watch them. We need to make sure it’s safe and works well. At the same time, we have to be careful not to cause any bad reactions.
Calculating Appropriate Transfusion Volume
To figure out how much blood to give, we use a formula. It’s: weight (kg) x increment in Hb (g/dL) x 3/(Hct of blood product). For example, if a 10 kg kid needs a 3 g/dL increase in hemoglobin, using blood with a 60% hematocrit, we calculate: 10 kg x 3 g/dL x 3/0.6 = 150 mL. It’s important to know the blood product’s hematocrit because it can change.
The speed at which we give the blood is also key. We start slow, at 0.5-1 mL/min for the first 15 minutes to watch for any bad reactions. If it goes well, we can speed it up. For kids, a good rate is 2-4 mL/kg/hour, but we adjust based on how they’re doing and how they react.
Essential Monitoring During and After Transfusion
Watching the patient closely during and after the transfusion is very important. We look for signs of bad reactions, like fever, chills, rash, or changes in their vital signs. We check their vital signs before, during, and after the transfusion.
- Watch for signs of too much fluid, which can be a problem for kids with heart or kidney issues.
- Look for signs of hemolysis or other bad reactions.
- See how well the patient is doing with the transfusion.
After the transfusion, we keep an eye on their hemoglobin levels and overall health. This helps us make sure the transfusion worked as planned. We can then adjust plans based on how they did.
By carefully planning how much blood to give and watching patients closely, we can make sure blood transfusions are safe and effective for kids.
Conclusion: Evidence-Based Approach to Pediatric Transfusion Decisions
An evidence-based approach is key to better patient care in pediatric transfusions. We talked about how important hemoglobin levels are in deciding when a child needs a blood transfusion. We looked at the recommended levels for different situations.
For stable kids, a hemoglobin level of 7 g/dL is the standard. But, kids who are very sick or have heart problems might need levels between 8-13 g/dL. We also discussed signs that show a child needs a transfusion, even if their hemoglobin is okay. These signs include a fast heart rate, trouble breathing, and feeling very tired.
When deciding on transfusions, we must look at more than just hemoglobin levels. We need to think about how well tissues are getting oxygen and the child’s overall health. By using evidence and carefully choosing when to transfuse, we can reduce risks. This way, we make sure kids get the best care possible.
FAQ’s:
What is the recommended hemoglobin threshold for pediatric transfusion?
For kids, the hemoglobin threshold for transfusion depends on their health. Generally, it’s 7 g/dL for those who are stable.
Why is a blood transfusion necessary for low hemoglobin levels?
When hemoglobin is low, a transfusion is needed. It boosts red blood cells and oxygen to tissues. This helps with fatigue, shortness of breath, and dizziness.
What are the clinical signs that indicate the need for transfusion despite a hemoglobin level?
Signs needing a transfusion include a fast heart rate, unstable blood pressure, and trouble breathing. Also, needing more oxygen, feeling tired, and changes in mental state are signs.
How is the appropriate transfusion volume calculated?
To figure out the right amount of blood, consider the patient’s weight, hemoglobin level, and how much more hemoglobin is needed.
What are the possible complications of unnecessary transfusions?
Unnecessary transfusions can lead to lung problems, blood overload, and higher risks of infections and allergic reactions.
What factors beyond hemoglobin levels influence transfusion decisions?
Decisions on transfusions also look at tissue oxygen, the underlying condition, and the patient’s overall health.
When are higher hemoglobin thresholds necessary for transfusion?
Kids who are very sick, have heart issues, or have had a stem cell transplant might need higher hemoglobin levels. These are usually 8-13 g/dL.
How are hemoglobin levels measured and interpreted in children?
Hemoglobin levels are checked through blood tests. The results are looked at with the patient’s age, health, and lab findings to decide on transfusions.
What is the importance of clinical judgment in transfusion decisions?
Clinical judgment is key in deciding on transfusions. It combines lab results with symptoms to ensure the best care for the patient.
What is the benefit of a restrictive transfusion approach?
Using a hemoglobin threshold of 7 g/dL for transfusions helps avoid unnecessary blood use. It reduces risks and saves blood resources.
References
- Valentine, S. L., et al. (2018). Consensus recommendations for red blood cell transfusion practices in critically ill children. Pediatric Critical Care Medicine, 19(6), 617-621. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6126913/