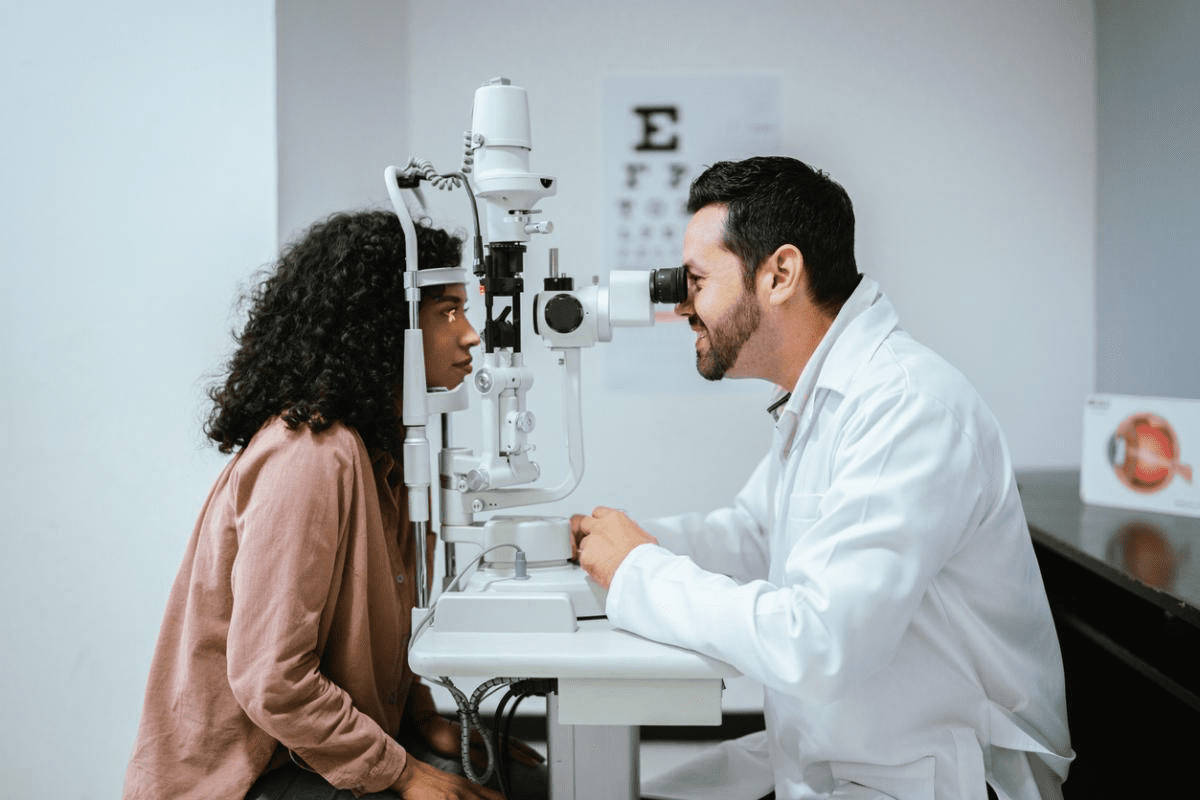
Autoimmune eye diseases represent a significant spectrum of conditions. The immune system attacks ocular tissues, causing inflammation. This can lead to vision-threatening complications. We are committed to helping patients understand these complex conditions.Is bloodshot eyes autoimmune disease related? Explore the top 7 causes, key symptoms, and effective treatments for relief.
The immune system’s attack on delicate structures like the retina and optic nerve can cause various autoimmune eye disorders. It’s important to understand these diseases for prompt diagnosis and effective treatment.
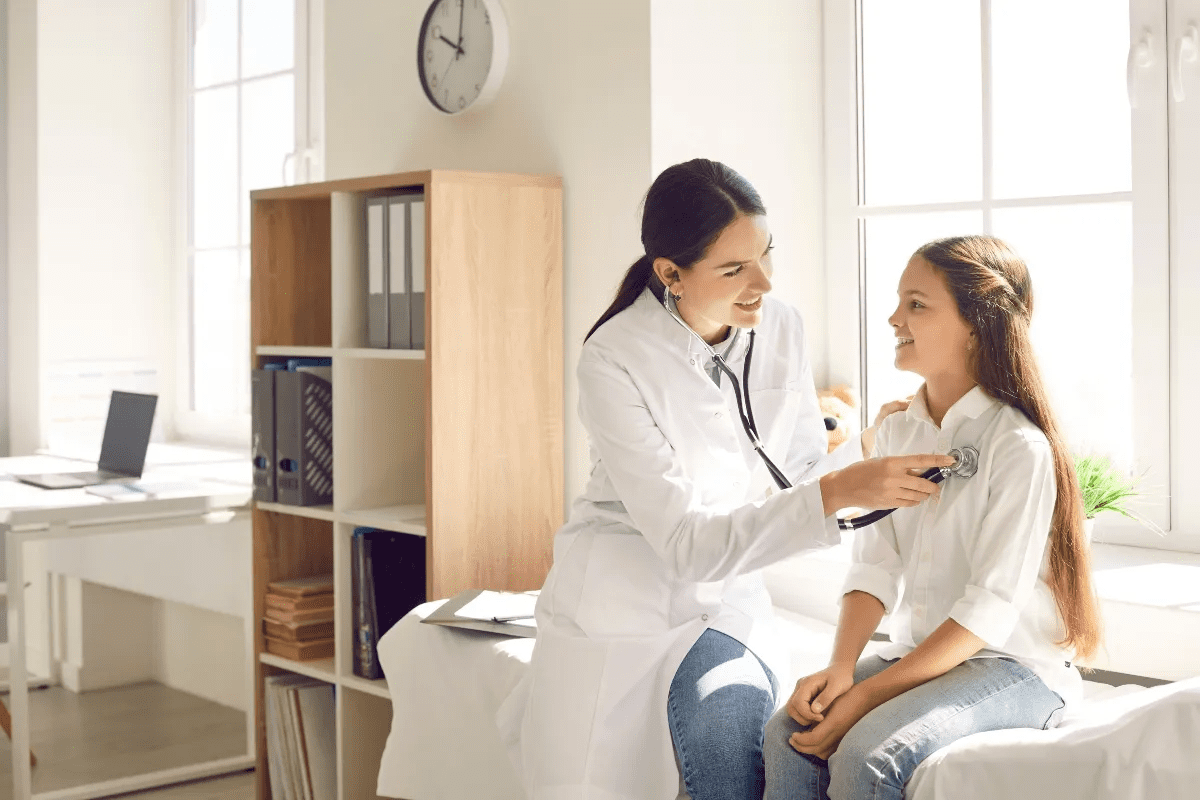
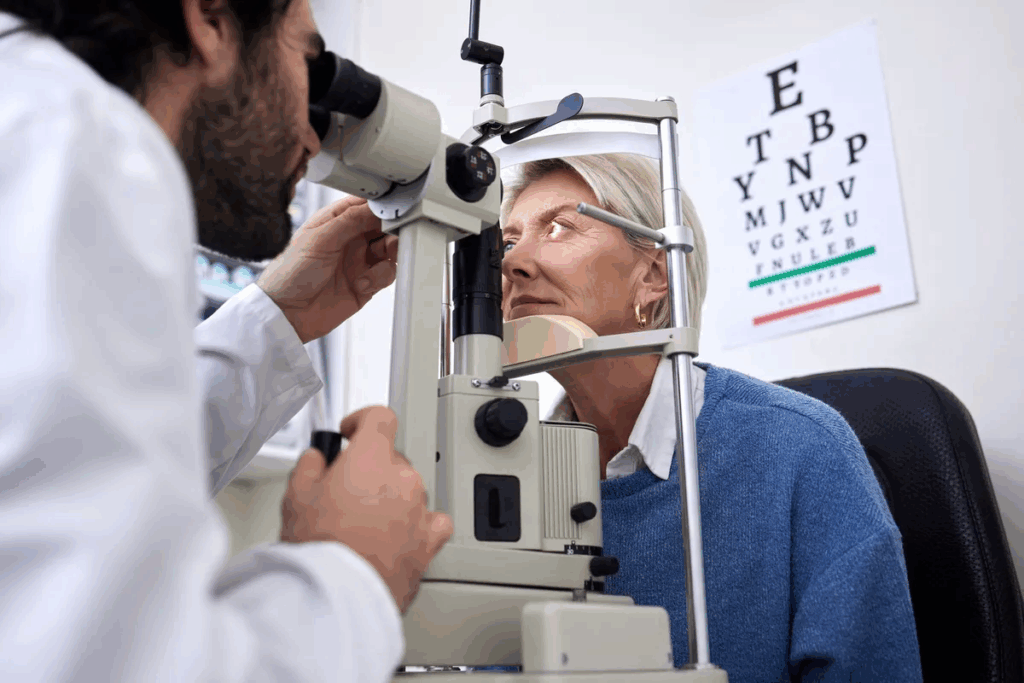
At Liv Hospital, we focus on the patient. We follow international medical standards. This ensures patients get accurate diagnosis and cutting-edge treatment for their specific condition.
Key Takeaways
- Autoimmune eye diseases are a group of conditions that affect the eyes.
- The immune system’s attack on ocular tissues leads to inflammation and vision problems.
- Prompt diagnosis and treatment are key to prevent vision loss.
- Liv Hospital follows a patient-centered approach to diagnose and treat autoimmune eye diseases.
- International medical standards are followed to ensure effective treatment.
Understanding Autoimmune Eye Diseases
Autoimmune eye diseases are complex conditions where the immune system attacks the eye’s tissues by mistake. This can cause inflammation, redness, and vision problems.
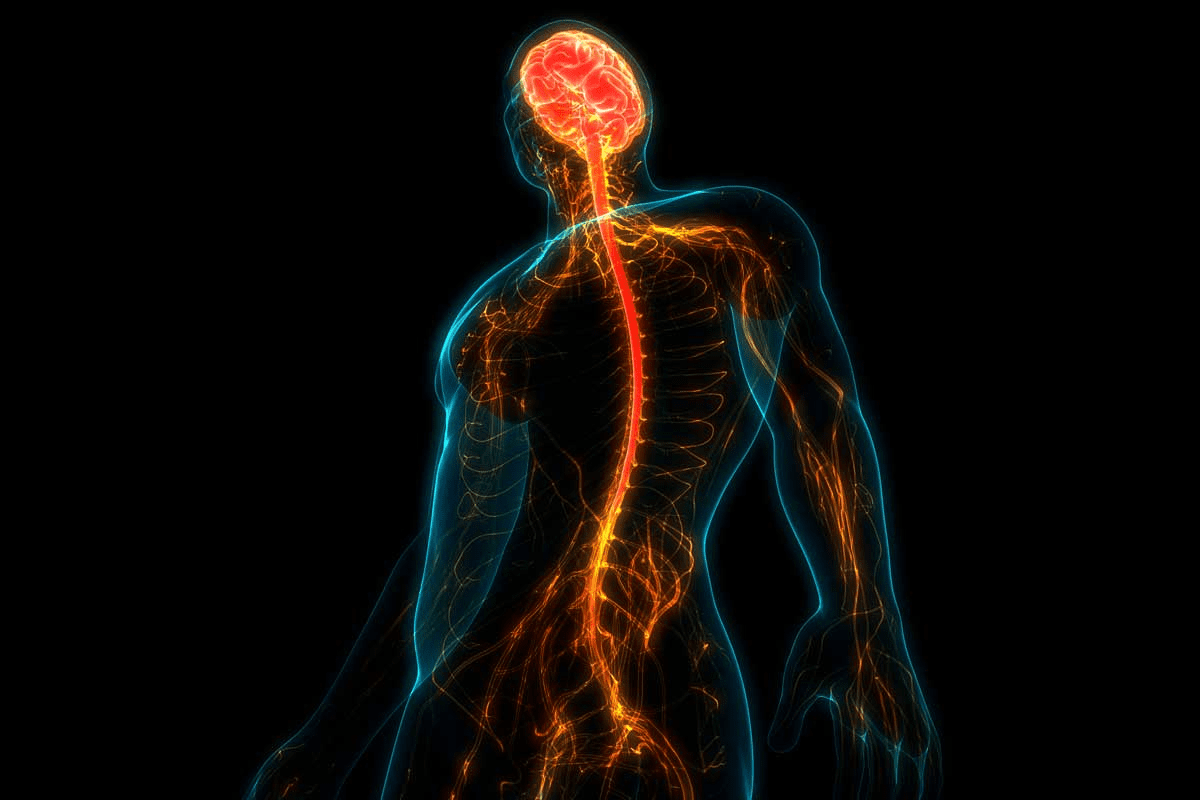
How the Immune System Attacks Ocular Tissues
In autoimmune eye diseases, the immune system goes wrong and attacks the eye’s tissues. This can cause inflammation and damage to parts like the uvea, retina, or optic nerve.
Bloodshot eyes are a common early sign of these conditions. This happens because the immune system’s attack causes more blood flow and swelling in the conjunctiva.
Risk Factors for Developing Autoimmune Eye Conditions
Several factors can increase the risk of getting autoimmune eye conditions. Genetics play a big role, as people with a family history of autoimmune diseases are more likely to get them.
About 50 percent of people with uveitis, a common autoimmune eye disorder, also have systemic autoimmune diseases. Knowing these risk factors is key for early diagnosis and treatment.
Autoimmune Disease | Association with Eye Conditions | Common Eye Symptoms |
Ankylosing Spondylitis | High association with uveitis | Eye pain, redness, vision problems |
Sarcoidosis | Can cause uveitis and other eye inflammation | Blurred vision, eye pain, sensitivity to light |
Behcet’s Disease | Often involves uveitis and retinal vasculitis | Eye pain, vision loss, retinal damage |
Bloodshot Eyes and Autoimmune Disease: The Critical Connection

Bloodshot eyes can signal early signs of autoimmune eye conditions. These conditions affect both the front and back parts of the eye. We’ll look into how autoimmune diseases impact the eyes, causing redness and inflammation.
Why Inflammation Causes Red Eyes in Autoimmune Conditions
In autoimmune diseases, the immune system attacks the body’s own tissues. This leads to inflammation in parts like the eyes. The increased blood flow to these areas makes the eyes appear red or bloodshot.
Conditions like Sjögren’s syndrome, lupus, and rheumatoid arthritis can cause dry eye and inflammation. This results in redness and discomfort.
Dry eye is common in these conditions. It happens when tear production drops or quality changes. This can cause discomfort, blurred vision, and even damage to the cornea.
The inflammation from autoimmune diseases can make dry eye symptoms worse. This makes the eyes look red and irritated.
Distinguishing Autoimmune Redness from Other Causes
Bloodshot eyes can be a sign of autoimmune diseases, but they can also be caused by allergies, infections, or environmental irritants. To figure out if red eyes are due to an autoimmune condition, it’s important to look at other symptoms and get a detailed eye exam.
Autoimmune redness often lasts longer and may come with pain, light sensitivity, or vision changes. On the other hand, redness from allergies or irritants might go away faster and may itch or have discharge. A thorough medical evaluation is needed to tell these causes apart and find the right treatment.
Uveitis: Inflammation of the Eye’s Middle Layer
Uveitis is a common eye condition linked to autoimmune diseases. It affects the middle layer of the eye, including the iris, ciliary body, and choroid. If not treated, it can cause serious vision problems.
We will look at the different types of uveitis, their symptoms, and how they relate to diseases like ankylosing spondylitis. Knowing this helps in diagnosing and treating the condition effectively.
Types and Symptoms of Uveitis
Uveitis is classified based on the affected part of the uvea and its duration. The main types are:
- Anterior Uveitis: Inflammation of the iris and ciliary body, often causing eye pain, redness, and sensitivity to light.
- Intermediate Uveitis: Affects the ciliary body and vitreous, leading to floaters and blurred vision.
- Posterior Uveitis: Involves the choroid and retina, causing vision loss and flashes of light.
- Panuveitis: Inflammation of all layers of the uvea, resulting in a mix of symptoms.
Symptoms vary by type but often include eye pain, redness, sensitivity to light, blurred vision, and floaters. Quick medical care is needed to avoid complications.
Connection to Ankylosing Spondylitis and Other Systemic Diseases
Uveitis is often linked to autoimmune diseases, like ankylosing spondylitis. Other conditions associated with uveitis include psoriatic arthritis, inflammatory bowel disease, and sarcoidosis.
Systemic Disease | Association with Uveitis |
Ankylosing Spondylitis | Strong association; uveitis is a common extra-articular manifestation. |
Psoriatic Arthritis | Uveitis can occur, more in patients with severe disease. |
Inflammatory Bowel Disease | Uveitis is seen in patients with Crohn’s disease and ulcerative colitis. |
Sarcoidosis | Granulomatous uveitis is a hallmark of ocular sarcoidosis. |
Corticosteroid and Immunosuppressive Treatments
Treatment for uveitis aims to reduce inflammation and prevent tissue damage. Corticosteroids are often the first choice, given topically, by injection, or orally. This depends on the severity and location of the inflammation.
If corticosteroids don’t work or are not tolerated, immunosuppressive therapies are used. These include medications like methotrexate, azathioprine, and biologic agents such as TNF-alpha inhibitors.
It’s important to have a treatment plan tailored to the individual. The response to treatment can vary a lot. Regular check-ups with an ophthalmologist are key to adjust treatments and manage side effects.
Sjögren’s Syndrome: Chronic Dryness and Inflammation
We look at Sjögren’s syndrome, where the immune system attacks moisture glands. This autoimmune disease causes chronic dryness and inflammation. It mainly affects the eyes and mouth.
Dry Eyes, Mouth, and Other Hallmark Symptoms
Sjögren’s syndrome is known for dry eyes and mouth. People feel grittiness or sand in their eyes and have blurred vision. They also struggle to swallow dry foods.
Autoimmune Attack on Moisture-Producing Glands
The immune system attacks glands in Sjögren’s syndrome. This leads to inflammation and less gland function. As a result, there’s less tear and saliva production, causing dryness.
The exact cause of Sjögren’s syndrome is not known. It’s thought to be a mix of genetics and environmental factors.
Artificial Tears and Systemic Medications for Management
Managing Sjögren’s syndrome focuses on easing symptoms and preventing problems. Artificial tears are key for dry eyes, providing relief and comfort. Sometimes, systemic medications like immunosuppressants or biologics are used to fight inflammation and control the immune system.
Treatment Approach | Description | Benefits |
Artificial Tears | Lubricating eye drops to alleviate dryness | Immediate relief, improved eye comfort |
Systemic Medications | Immunosuppressants or biologics to reduce inflammation | Reduced glandular inflammation, potentially increased tear production |
Punctal Occlusion | Procedure to block tear ducts | Conserves tears, enhances eye moisture |
Understanding Sjögren’s syndrome helps healthcare providers create effective treatment plans. This improves the quality of life for those affected.
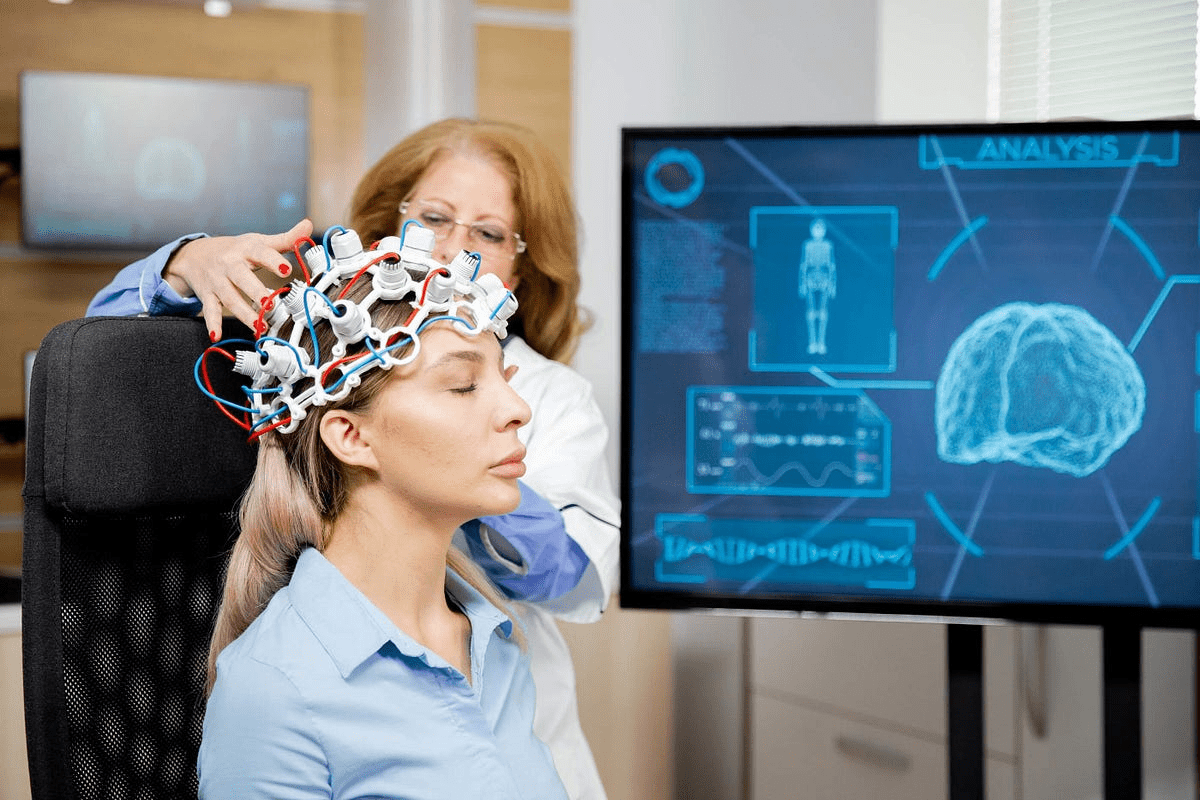
Optic Neuritis: Inflammation of the Optic Nerve
The optic nerve is key to our vision. When it gets inflamed, it’s called optic neuritis. This condition needs quick medical help. It causes vision loss and pain.
We’ll look at the symptoms, its link to multiple sclerosis, and treatment options.
Vision Loss and Pain Symptoms
Optic neuritis often starts with sudden vision loss in one eye. It also brings pain, mainly when moving the eye. The loss of vision can be mild or severe.
The Multiple Sclerosis Connection: Why 75% of MS Patients Develop It
Optic neuritis is closely tied to multiple sclerosis (MS). About 75% of MS patients will get optic neuritis. MS attacks the central nervous system, and optic neuritis is a common sign.
Knowing this link helps in diagnosing and treating MS.
Steroid Treatments and Visual Recovery Expectations
Corticosteroids are used to treat optic neuritis. Intravenous corticosteroids help speed up vision recovery. But, how much vision comes back varies.
Some people see fully again, while others may have lasting vision problems.
Early treatment is key to better outcomes for optic neuritis patients. Understanding symptoms, its MS link, and treatments helps doctors give better care.
Graves’ Ophthalmopathy: Thyroid-Related Eye Disease
Graves’ ophthalmopathy is an autoimmune condition that affects the tissues around the eye. It causes inflammation and distressing symptoms. This disease can significantly impact one’s quality of life, affecting both the appearance and function of the eyes.
Bulging Eyes, Lid Retraction, and Vision Changes
The symptoms of Graves’ ophthalmopathy vary among individuals. Common symptoms include bulging eyes (exophthalmos), lid retraction, and vision changes. These symptoms occur due to inflammation and swelling of tissues behind and around the eye, pushing the eyeball forward.
Some patients may experience mild symptoms like redness and dryness. Others may have more severe symptoms, including double vision and vision loss. Understanding these symptoms is key for early diagnosis and effective management.
How Thyroid Autoimmunity Affects Orbital Tissues
In Graves’ ophthalmopathy, the immune system mistakenly attacks the tissues around the eye. This includes the eyelids, eye socket, and lacrimal gland. The autoimmune response leads to inflammation and swelling, causing the characteristic bulging of the eyes.
The thyroid autoimmunity associated with Graves’ disease triggers this inflammation. The exact mechanisms are complex, involving genetic predisposition and environmental factors.
Aspect | Description |
Autoimmune Response | Immune system attacks orbital tissues |
Inflammation | Swelling and redness around the eyes |
Tissue Damage | Potential for permanent damage if untreated |
Treatment Options from Lubricants to Orbital Decompression
Treating Graves’ ophthalmopathy requires a multifaceted approach. Treatments are tailored to the severity of symptoms and the individual’s overall health. Initial treatments often include lubricants to alleviate dryness and irritation.
For more severe cases, treatments may involve corticosteroids to reduce inflammation, or even orbital decompression surgery to relieve pressure on the eyeball and improve eye movement. Other options might include radiation therapy or immunosuppressive medications.
We work closely with patients to develop a personalized treatment plan. Our goal is to alleviate symptoms, improve eye health, and enhance quality of life.
Scleritis: Inflammation of the Eye’s Protective Outer Layer
Scleritis causes a lot of pain and redness. It’s a serious condition that affects the sclera, the white outer layer of the eye. If not treated, it can harm your vision.
Severe Pain and Redness Symptoms
Scleritis is known for severe pain and redness. The pain feels deep and boring. It can make everyday tasks hard.
The redness comes from inflammation of the sclera. It can turn purplish.
Scleritis symptoms include:
- Pain that can be localized to the eye or radiate to the surrounding areas
- Redness and swelling of the sclera
- Sensitivity to light (photophobia)
- Tearing of the eye
- Potential vision disturbances
Association with Rheumatoid Arthritis and Other Conditions
Scleritis is often linked to rheumatoid arthritis. This disease mainly affects joints but can also harm the eyes. It’s also connected to lupus and granulomatosis with polyangiitis.
Knowing the connection between scleritis and these diseases is key. It helps find the root cause of eye inflammation.
Anti-Inflammatory and Immunosuppressive Treatment Approaches
Treatment for scleritis includes anti-inflammatory and immunosuppressive therapies. These aim to reduce inflammation and pain. NSAIDs are often the first choice, but corticosteroids or immunosuppressive drugs may be needed for severe cases.
Biologic agents might be used in some cases. The right treatment depends on the scleritis’s severity, any underlying diseases, and the patient’s health.
It’s vital to work with healthcare providers. They can create a treatment plan that covers both the eye and any systemic diseases.
Behçet’s Disease: Multisystem Disorder with Ocular Involvement
Behçet’s disease is a complex condition that affects many parts of the body, including the eyes. It causes a range of symptoms, like oral and genital ulcers, skin lesions, and eye inflammation. We will look at how Behçet’s disease affects the eyes, its causes, and treatment options.
Recurrent Eye Inflammation and Ulceration Patterns
Ocular involvement in Behçet’s disease can lead to serious complications, such as uveitis and retinal vasculitis. These conditions can cause severe inflammation and may lead to vision loss if not managed properly. The pattern of eye inflammation can vary, with some patients experiencing recurring episodes of uveitis or retinal vasculitis.
Common Ocular Manifestations:
- Uveitis
- Retinal vasculitis
- Retinal vein occlusion
- Optic neuritis
Genetic and Environmental Triggers
The exact cause of Behçet’s disease is not fully understood. It is believed to involve a mix of genetic and environmental factors. Certain genetic markers, like HLA-B51, increase the risk of developing the disease. Environmental triggers, including infections, may also trigger the onset of Behçet’s disease in susceptible individuals.
“The pathogenesis of Behçet’s disease is complex and multifactorial, involving an interplay between genetic predisposition and environmental factors.” –
Expert Opinion
Immunomodulatory Therapies and Visual Prognosis
Treatment for Behçet’s disease often involves immunomodulatory therapies to reduce inflammation and prevent eye complications. Corticosteroids and immunosuppressive agents are commonly used. Thanks to these therapies, the visual prognosis for patients with Behçet’s disease has improved. Regular monitoring is key to prevent long-term damage.
Treatment Options | Description | Benefits |
Corticosteroids | Reduce inflammation | Rapid control of acute inflammation |
Immunosuppressive Agents | Suppress immune system activity | Long-term control of disease activity |
Biologic Agents | Target specific molecules involved in inflammation | Effective for refractory cases |
We stress the importance of a complete treatment plan for managing Behçet’s disease and its eye manifestations. Understanding the disease’s complexities and using the right therapies can help patients achieve better outcomes and reduce the risk of vision loss.
Diagnosing and Managing Autoimmune Eye Diseases
Diagnosing autoimmune eye diseases needs a detailed and multi-faceted approach. Finding an underlying inflammatory process early is key. This is because many eye problems can be treated or prevented if caught in time. We will explore how to diagnose and manage these diseases, focusing on the role of specialized tests, imaging, and teamwork between eye doctors and rheumatologists.
Specialized Tests and Imaging Techniques
Diagnosing autoimmune eye diseases involves several specialized tests and imaging methods. Optical Coherence Tomography (OCT) gives high-resolution images of the retina, spotting inflammatory changes or damage. Fluorescein angiography is also vital, as it checks the retina’s blood vessels for leaks or other signs of disease.
Other tools include ultrasound biomicroscopy for detailed images of the eye’s front part and blood tests to find specific autoantibodies. These tests help diagnose and track autoimmune eye diseases.
Collaborative Care Between Ophthalmologists and Rheumatologists
Managing autoimmune eye diseases well often needs teamwork between eye doctors and rheumatologists. Ophthalmologists deal with eye disorders, while rheumatologists handle autoimmune diseases affecting muscles and other body parts. Together, they offer full care, tackling both eye and body issues.
This team effort ensures patients get coordinated treatment, like immunosuppressive drugs and biologic agents. This helps manage eye symptoms and the underlying disease. The treatment plan is regularly checked and adjusted based on the patient’s progress and response.
Conclusion: Living Well with Autoimmune Eye Conditions
Understanding and managing autoimmune eye diseases can greatly improve life quality. These conditions may not have a cure, but proper treatment can manage symptoms. This helps prevent permanent eye damage.
Managing these diseases requires a detailed plan. This includes specialized tests and imaging. It also involves working closely with ophthalmologists and rheumatologists. This approach helps reduce complications and improves treatment results.
Effective management helps people stay independent and enjoy a better life. It’s key to seek medical help if symptoms get worse. This ensures timely and best care for those with autoimmune eye diseases.
FAQ
What are autoimmune eye diseases?
Autoimmune eye diseases happen when the immune system attacks the eye’s tissues. This leads to inflammation and damage. Examples include uveitis, scleritis, and optic neuritis.
How do autoimmune eye diseases affect vision?
These diseases can cause many vision problems. Symptoms include blurred vision, double vision, and even blindness. The severity of the inflammation determines the impact on vision.
What is the connection between bloodshot eyes and autoimmune diseases?
Bloodshot eyes can be a sign of autoimmune eye diseases. This is because inflammation in the eye occurs. The redness is due to the immune system attacking the eye’s tissues.
What is uveitis, and how is it treated?
Uveitis is inflammation in the eye’s middle layer. Treatment includes corticosteroids and immunosuppressive therapies. These help reduce inflammation and prevent damage.
How does Sjögren’s syndrome affect the eyes?
Sjögren’s syndrome causes chronic dryness and inflammation in the eyes. This is because the immune system attacks moisture-producing glands. Treatment includes artificial tears and systemic medications.
What is the link between optic neuritis and multiple sclerosis?
Optic neuritis is often linked to multiple sclerosis. About 75% of those with multiple sclerosis develop optic neuritis. It can cause vision loss and pain.
How is Graves’ ophthalmopathy related to thyroid autoimmunity?
Graves’ ophthalmopathy is caused by thyroid autoimmunity affecting the orbital tissues. Symptoms include bulging eyes and vision changes. Treatment options range from lubricants to orbital decompression.
What are the symptoms of scleritis, and how is it treated?
Scleritis causes severe pain and redness due to inflammation of the eye’s outer layer. Treatment involves anti-inflammatory and immunosuppressive approaches. It’s often associated with conditions like rheumatoid arthritis.
What is Behçet’s disease, and how does it affect the eyes?
Behçet’s disease is a disorder that can cause eye inflammation and ulceration. Treatment involves immunomodulatory therapies. This helps manage symptoms and improve vision.
How are autoimmune eye diseases diagnosed?
Diagnosing these diseases requires specialized tests and imaging. It’s important for ophthalmologists and rheumatologists to work together. This ensures accurate diagnosis and effective management.
Can autoimmune eye diseases be managed effectively?
Yes, with the right treatment and care, these diseases can be managed. Treatment plans are tailored to each individual’s needs. This improves the quality of life for those affected.
What are the risk factors for developing autoimmune eye conditions?
Risk factors include genetic predisposition, environmental triggers, and other autoimmune diseases. Understanding these can help in early detection and management.
How does inflammation affect the eye in autoimmune diseases?
Inflammation from the immune system’s attack can lead to various eye conditions. This includes uveitis, scleritis, and optic neuritis. It can cause vision problems.
References
National Center for Biotechnology Information. Autoimmune Eye Diseases: Symptoms, Causes, and Treatment. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC8593335/