Last Updated on November 20, 2025 by Ugurkan Demir
As the world’s population gets older, bone marrow failure syndromes like myelodysplastic syndrome (MDS) are becoming a big health worry for seniors. These issues bring special challenges for doctors to diagnose and treat.
At Liv Hospital, we know how important it is to tackle the challenges of bone marrow failure in the elderly with care that’s tailored to each person. Our team works together to give the best care possible to those who need it most.
Elderly patients with myelodysplastic syndrome face different outcomes based on how severe their disease is and other factors. It’s key to understand MDS and its effects to help improve their life expectancy and quality of life.
Key Takeaways
- Understanding bone marrow failure is key for caring for elderly patients.
- MDS prognosis varies a lot among elderly patients.
- Personalized care improves outcomes for older adults.
- Disease severity greatly affects survival chances.
- Teamwork is vital for managing MDS well.
Understanding Bone Marrow Function and Failure
It’s important to know how bone marrow works to understand health problems it can cause, like in older adults. Bone marrow is the soft tissue in some bones that makes blood cells. When it doesn’t work right, it can lead to serious health issues.
Normal Bone Marrow Function
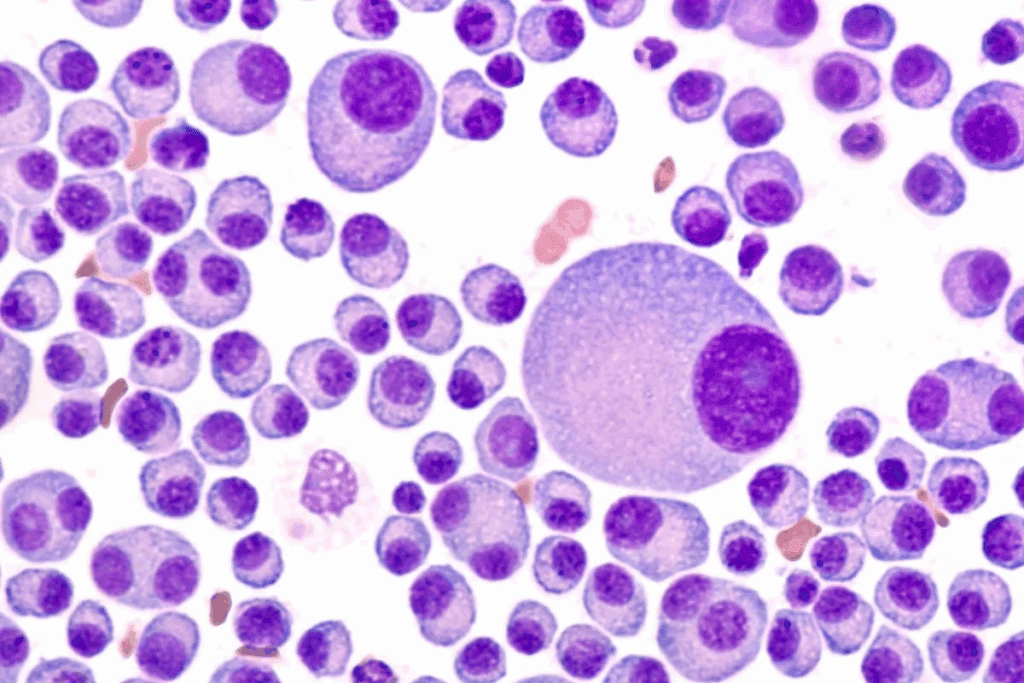
Bone marrow is key for making blood cells, a process called hematopoiesis. It turns stem cells into red and white blood cells and platelets. This is vital for carrying oxygen, fighting off infections, and stopping bleeding.
For bone marrow to work well, it needs to balance making new stem cells and turning them into blood cells. This balance keeps the body supplied with the right amount of blood cells.
How Bone Marrow Failure Develops
Bone marrow failure happens when it can’t make enough blood cells. This leads to problems like aplastic anemia and myelodysplastic syndromes. It can be caused by genetic issues, toxins, or infections.
The process of bone marrow failure is complex. It involves many cellular and molecular changes. For example, myelodysplastic syndromes make it hard for the bone marrow to make blood cells, raising the risk of leukemia.
| Condition | Description | Common Symptoms |
| Aplastic Anemia | A condition where the bone marrow fails to produce blood cells. | Fatigue, infections, bleeding. |
| Myelodysplastic Syndromes | A group of disorders caused by poorly formed or dysfunctional blood cells. | Anemia, infections, bruising. |
It’s vital to understand how bone marrow failure happens to find good treatments, mainly for the elderly. They are more likely to get these problems because their bone marrow doesn’t work as well with age.
Bone Marrow Failure in the Elderly: An Overview
Bone marrow failure in the elderly is a complex condition. It’s important to understand its epidemiology. As we age, the risk of developing bone marrow failure increases.
Prevalence and Incidence Rates
Aplastic anemia is a rare disorder with a bimodal age distribution. It affects 0.6 to 6.1 cases per million individuals. Myelodysplastic syndromes (MDS), another condition, are more common in older adults.
Studies show MDS incidence increases with age, after 60. It’s most diagnosed in those 70 to 80 years old. This highlights the need for awareness and understanding of MDS in the elderly.
| Age Group | Incidence Rate of MDS (per 100,000) |
| 60-69 | 15-20 |
| 70-79 | 30-40 |
| 80+ | 50-60 |
Age-Related Risk Factors
Older age is a significant risk factor for MDS and other bone marrow failure disorders. Our bone marrow undergoes natural changes with age, increasing the risk. Older adults also have more comorbidities and exposure to toxins, raising the risk further.
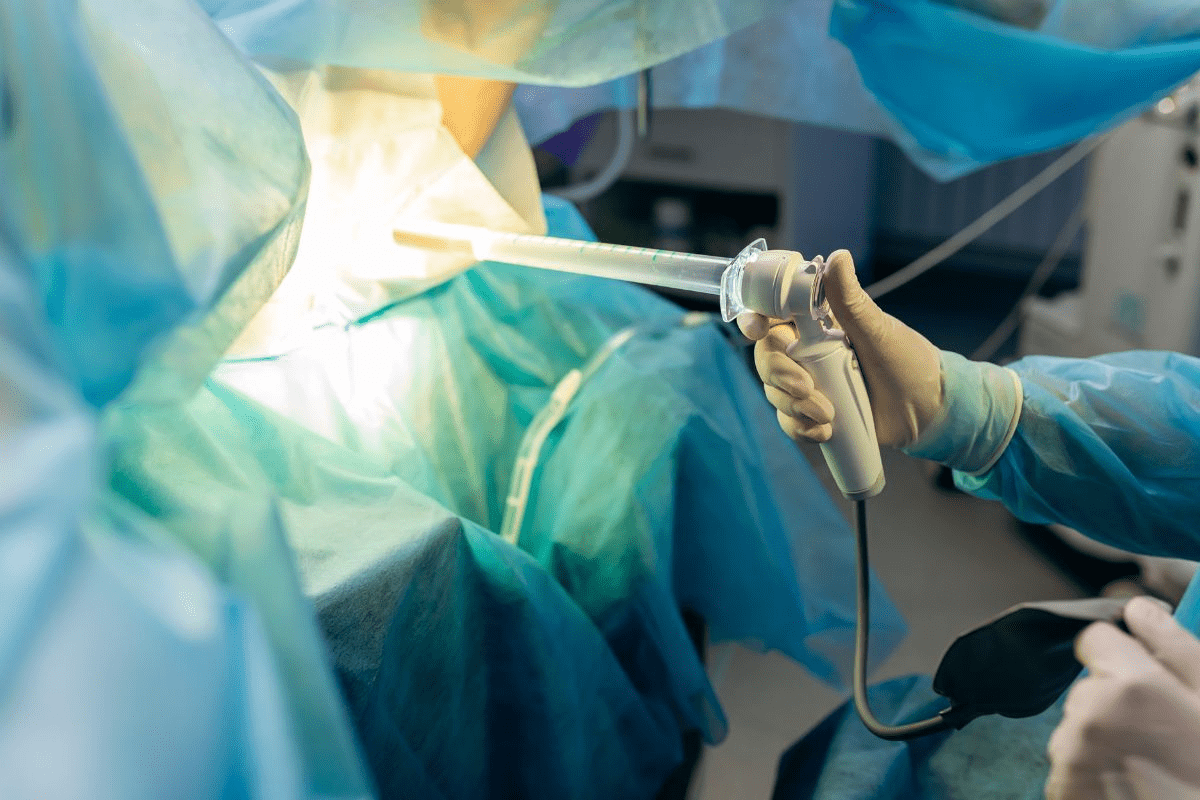
The image below illustrates the complex relationship between age and bone marrow failure.
Understanding age-related risk factors for bone marrow failure is key. Recognizing the complex interplay between age, comorbidities, and environmental exposures helps in managing care for elderly patients with bone marrow failure.
Essential Fact #1: Increased Disease Severity in Older Adults
The severity of bone marrow failure grows more in older adults. This shows up in different ways. As we get older, our bone marrow makes fewer healthy blood cells. This makes bone marrow failure worse.
Clinical Manifestations in Geriatric Patients
Older patients with bone marrow failure show more symptoms. These include tiredness, infections, and bleeding problems. This is because they don’t make enough blood cells.
Studies show that older adults with aplastic anemia have more severe platelet problems. Platelets are important for blood to clot.
Severe Thrombocytopenia at Diagnosis
Older adults face big risks from severe platelet problems. This makes bleeding worse and makes treatment harder. Our data show that elderly patients with aplastic anemia don’t respond as well to first treatments.
| Age Group | Severity of Thrombocytopenia | Response to First-Line Therapy |
| Younger Adults (<60) | Mild to Moderate | Higher Response Rate |
| Older Adults (≥60) | Severe | Lower Response Rate |
The table shows that older adults face more severe platelet issues and lower treatment success. This shows we need special care for older patients with bone marrow failure.
It’s key to understand these differences for better treatment plans. We must think about the special challenges older adults face. This includes other health issues and a reduced ability to recover.
“The management of bone marrow failure in older adults requires a complete approach. We must consider the disease’s severity, the patient’s health, and the risk of treatment side effects.” -Expert Opinion
By recognizing the increased severity in older adults, we can improve their care. This helps those who are most vulnerable.
Essential Fact #2: Myelodysplastic Syndrome (MDS) in Elderly Patients
Elderly people are more likely to get MDS, a condition that affects blood cell production. As we get older, the chance of getting MDS goes up. This makes it a big worry for older adults.
MDS Pathophysiology in Aging Populations
MDS in older adults is caused by a mix of genetic changes, environmental factors, and changes in the bone marrow. Aging leads to more genetic changes in blood-making cells, which can cause MDS.
Studies show that aging changes the bone marrow in several ways. These include:
- Changes in how genes work
- Shorter telomeres
- More oxidative stress
- Worse DNA repair
These changes make it easier for MDS to develop. The mix of these factors and the patient’s genes decides how likely and severe MDS will be.
Common Subtypes in Seniors
MDS is a group of disorders with different types. In older adults, some common types are:
| Subtype | Characteristics | Prognosis |
| Refractory Cytopenia with Unilineage Dysplasia (RCUD) | Dysplasia in one myeloid lineage | Variable, depending on cytogenetics |
| Refractory Anemia with Ring Sideroblasts (RARS) | Presence of ring sideroblasts | Generally better prognosis |
| Refractory Cytopenia with Multilineage Dysplasia (RCMD) | Dysplasia in multiple lineages | Variable, often worse than RCUD |
Knowing these subtypes helps doctors predict how well a patient will do and choose the right treatment. A leading expert says,
“The way we classify MDS has changed to include molecular features. This helps us make more accurate diagnoses and plan treatment better.”
When treating MDS, we must look at each patient’s unique situation. The mix of MDS, age, and other health issues means we need a care plan that’s tailored to each person.
Essential Fact #3: Poorer Treatment Response Rates
Bone marrow failure in older adults often leads to poorer outcomes. This is because treatments may not work as well as they do in younger people. Elderly patients face big challenges in getting better from this condition.
First-Line Therapy Response Statistics
First treatments for bone marrow failure, like immunosuppressive therapy (IST) for aplastic anemia, don’t work as well in older adults. Research shows that older people tend to have lower success rates than younger ones.
| Age Group | Response Rate to IST |
| 18-40 years | 60-70% |
| 41-60 years | 40-60% |
| 61+ years | 20-40% |
The table shows that success rates with IST go down as age increases. This means older patients might need different or extra treatments.
Factors Contributing to Reduced Efficacy
Several things make treatments less effective in older adults with bone marrow failure. These include:
- Comorbidities: Older adults often have more health issues that make treatment harder.
- Age-related decline in physiological reserve: As we get older, our bodies can’t bounce back as well from treatment stress.
- Pharmacokinetic changes: How our bodies handle drugs changes with age, which can make treatments less effective or more toxic.
Knowing these factors helps doctors create better treatment plans for older patients with bone marrow failure.
Essential Fact #4: Age as an Independent Risk Factor for Mortality
Older adults with bone marrow failure face higher mortality risks than younger people. As we get older, our bodies recover less from diseases and treatments. This makes age a key factor in how well patients with bone marrow failure do.
Survival Statistics by Age Group
Survival rates for bone marrow failure patients differ by age. Older patients usually have worse survival chances. For example, those over 75 with myelodysplastic syndrome (MDS) have a much lower life expectancy than younger patients.
- Patients under 60: Generally have better survival rates, with some studies indicating a median survival of over 5 years.
- Patients between 60-75: Experience a decline in survival rates, with median survival ranging from 2-5 years.
- Patients over 75: Face the poorest survival outcomes, with median survival often less than 2 years.
Life Expectancy Considerations
When looking at pre-leukemia life expectancy and MDS disease and life expectancy, many factors come into play. These include age, overall health, and the disease’s specifics. Older patients often have other health issues and less energy, making treatment harder and life expectancy shorter.
Life expectancy for patients with myelodysplastic disorders varies a lot. For example, those with lower-risk MDS might live several years to over a decade, depending on their age and health at diagnosis. But those with higher-risk MDS or who develop acute myeloid leukemia (AML) have a much worse outlook, with life expectancy in months, not years.
We must think about these factors when talking about treatment and prognosis with elderly patients. We need to make sure we provide care that fits their unique needs and situations.
Essential Fact #5: Elevated Risk of Disease Progression
Bone marrow failure in the elderly comes with a higher risk of disease getting worse. This is true, mainly for those with myelodysplastic syndrome (MDS). As people get older, MDS can turn into more serious forms, making treatment harder.
MDS Evolution in Elderly Patients
MDS is a set of disorders where blood cells don’t form right. In older adults, MDS can get worse faster because of bone marrow decline. This makes managing the disease even tougher.
Key factors contributing to MDS evolution include:
- Genetic mutations accumulated over time
- Age-related changes in the bone marrow microenvironment
- Presence of comorbidities
Progression to Acute Myeloid Leukemia
One big worry with MDS is it can turn into acute myeloid leukemia (AML). Older patients face a higher risk of this, which often means a worse outlook.
| Age Group | Risk of Progression to AML |
| 60-69 years | 20-30% |
| 70-79 years | 30-40% |
| 80+ years | 40-50% |
It’s key to understand the risk of disease getting worse for MDS in the elderly. We need to think about each patient’s health, other health issues, and what they want when planning treatment.
Essential Fact #6: Treatment Limitations and Guidelines for Elderly Patients
Elderly patients with bone marrow failure face unique challenges. Their frailty and comorbidities make treatment tricky. It’s key to weigh the risks and benefits of each option carefully.
Impact of Frailty and Comorbidities
Frailty and comorbidities greatly affect treatment choices for elderly MDS patients. These conditions make it hard for them to handle intense treatments. So, we must check their health before starting any treatment.
We use geriatric assessments to look at their physical health, comorbidities, and support system. This helps us create treatment plans that fit their needs.
Cautious Use of Anti-Thymocyte Globulin (ATG) in Patients Over 60
Anti-Thymocyte Globulin (ATG) is a treatment for some MDS patients. But, using it in those over 60 is cautious due to side effects and reduced tolerance.
Older patients on ATG face higher risks of infections and complications. So, we carefully consider the benefits against these risks when deciding on ATG for the elderly.
| Treatment Considerations | Patients Under 60 | Patients Over 60 |
| ATG Use | Generally well-tolerated | Cautious use due to possible side effects |
| Bone Marrow Transplantation | Often considered | Limited by frailty and comorbidities |
| Supportive Care | Used as needed | Frequently emphasized due to treatment limitations |
Bone Marrow Transplantation Considerations
Bone marrow transplantation can cure MDS, but it’s tough for elderly patients. Their frailty and comorbidities limit its use. We look at their health and ability to handle the transplant.
In some cases, we might use reduced-intensity conditioning for elderly patients. This is decided on a case-by-case basis, considering their health and risks.
By carefully considering these factors and tailoring treatment plans, we can improve care for elderly patients with bone marrow failure.
Essential Fact #7: Need for Personalized, Multidisciplinary Care
Older adults with bone marrow failure need personalized, multidisciplinary care. As we age, our health needs get more complex. We need a care plan that covers the disease and the person’s overall well-being.
Comprehensive Geriatric Assessment
A geriatric assessment is key for elderly patients with bone marrow failure. It looks at physical, emotional, and social needs. This gives a full picture of the patient’s health.
For example, a patient with MDS might need a care plan that balances treatment with quality of life. A geriatric assessment helps find the best treatment and support for each patient.
Balancing Disease Management and Quality of Life
Elderly patients with bone marrow failure face a tough balance. We must weigh treatment options against quality of life. We consider the patient’s health, life expectancy, and personal wishes.
For instance, when treating MDS in the elderly, we must think about the benefits and risks. Sometimes, supportive care like blood transfusions is better than aggressive treatments.
Supportive Care Strategies
Supportive care is essential for managing bone marrow failure in the elderly. It includes blood transfusions, antibiotics, and growth factor support. These help manage symptoms and prevent complications.
We also consider the patient’s pre-leukemia life expectancy when planning treatment. By providing good supportive care, we can improve the quality of life and reduce risks.
Common blood disorders in the elderly, like anemia and thrombocytopenia, need careful management. Understanding these disorders and providing personalized care helps elderly patients with bone marrow failure.
Conclusion: Navigating Care Decisions for Elderly Patients with Bone Marrow Failure
Understanding bone marrow failure in the elderly is key to better care and outcomes. Myelodysplastic syndrome in older patients often has a tough prognosis. This is due to age and other health issues.
The challenges of bone marrow failure in older adults need a detailed approach. Knowing the facts helps healthcare teams make better decisions. They consider how MDS disease affects life expectancy.
Personalized, team-based care is essential for managing bone marrow failure in the elderly. This method helps balance treating the disease with improving quality of life. By focusing on each patient’s needs, we can improve their well-being.
FAQ
What is bone marrow failure, and how does it affect the elderly?
Bone marrow failure happens when the bone marrow can’t make enough blood cells. This leads to health problems. For older adults, it can cause anemia, infections, and bleeding issues, affecting their life quality.
What are the common causes of bone marrow failure in older adults?
Causes include myelodysplastic syndromes (MDS), aplastic anemia, and exposure to harmful chemicals or radiation. Age also plays a role as the bone marrow function declines with age.
How is myelodysplastic syndrome (MDS) diagnosed and treated in elderly patients?
Doctors use blood tests, bone marrow biopsies, and genetic tests to diagnose MDS. Treatment depends on the MDS type and severity. It can range from supportive care to chemotherapy and bone marrow transplants, considering the patient’s health and age.
What is the prognosis for elderly patients with myelodysplastic syndrome (MDS)?
The outlook for elderly MDS patients depends on several factors. These include the MDS type, the patient’s health, and other medical conditions. Older adults often face a tougher time due to less tolerance for strong treatments and higher disease progression risk.
How does age impact the treatment of bone marrow failure?
Age affects treatment options for bone marrow failure. Older adults may have other health issues, reduced organ function, and less ability to handle aggressive treatments. Treatment plans focus on balancing effectiveness with the patient’s quality of life and treatment tolerance.
What are the treatment limitations for elderly patients with bone marrow failure?
Treatment limitations include comorbidities, frailty, and reduced organ function. These make intensive treatments like bone marrow transplantation risky. Older adults also face a higher risk of complications, requiring careful, personalized planning.
Why is personalized, multidisciplinary care important for elderly patients with bone marrow failure?
Personalized, multidisciplinary care is key. It meets the complex needs of elderly patients. It includes geriatric assessment, disease management, and supportive care to enhance outcomes and quality of life.
What is the life expectancy for patients with myelodysplastic syndrome (MDS)?
Life expectancy for MDS patients varies. It depends on the MDS type, age, health, and treatment response. Some may live for years with supportive care, while others may see rapid disease progression.
How does bone marrow failure progress to acute myeloid leukemia (AML)?
Bone marrow failure, like MDS, can turn into AML, a more aggressive blood cancer. The risk of progression depends on the MDS type and other factors. Some patients need close monitoring and timely intervention.
What supportive care strategies are available for elderly patients with bone marrow failure?
Supportive care includes blood transfusions, growth factor support, infection management, and symptom control. These strategies aim to improve quality of life and manage bone marrow failure complications.
References
- Contejean, A., et al. (2018). Aplastic anemia in the elderly: A nationwide survey on clinical characteristics and treatment outcomes. Annals of Hematology, 97(10), 1787–1795. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6355477/
- Zhao, J., & DeVeaux, M. (2021). Marrow failure and aging: The role of “inflammaging”. Experimental Hematology, 96, 1-12. https://www.sciencedirect.com/science/article/abs/pii/S1521692621000487