At Liv Hospital, we know how important bone marrow is. It makes blood cells that help fight off infections, carry oxygen, and stop bleeding. If it doesn’t work right, serious health problems can happen. A bone marrow failure disorder occurs when the marrow can’t make enough blood cells, making life harder. Discover 4 key causes of bone marrow suppression causes and failure disorders explained in detail.
We focus on caring for our patients and are experts in treating bone marrow problems. Knowing what causes these issues is key to fixing them. In this article, we’ll look at the main reasons for bone marrow suppression and failure. This will help both patients and doctors tackle these problems.
Key Takeaways
- Understanding bone marrow’s role is key to health.
- Bone marrow failure disorders really affect life quality.
- Finding out why bone marrow suppression happens is vital for treatment.
- Liv Hospital offers top care for complex bone marrow issues.
- Good treatment depends on knowing the cause.
Understanding Bone Marrow Function and Its Importance
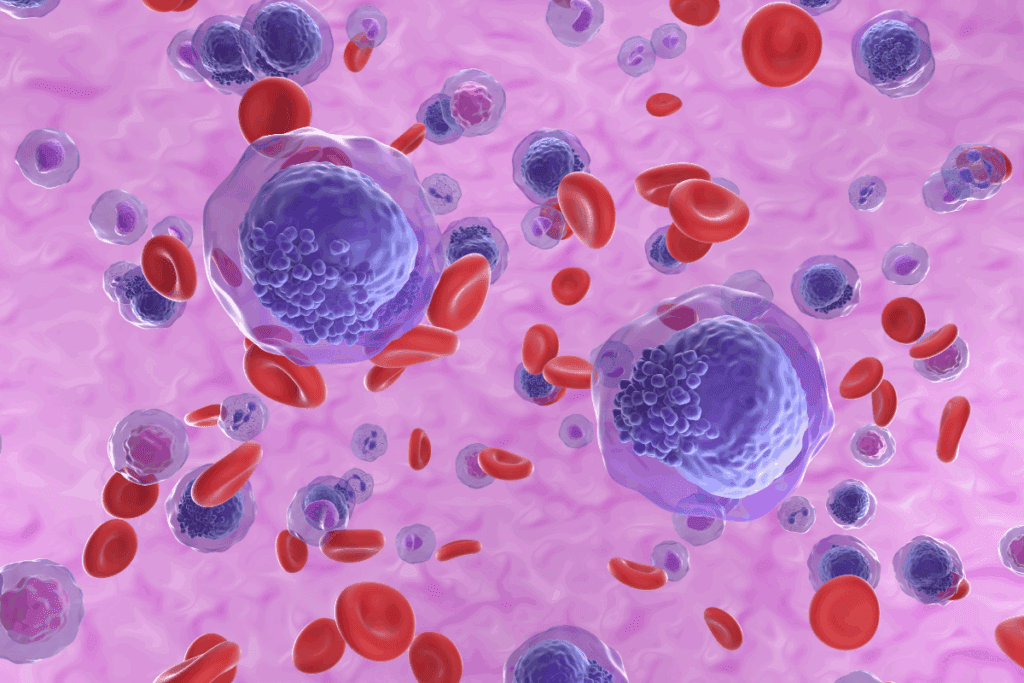
It’s key to know how bone marrow works to keep our blood cells healthy. Bone marrow is a soft tissue inside bones like the hips and thighbones. It makes blood cells through a process called hematopoiesis.
The Role of Bone Marrow in Blood Cell Production
Bone marrow is vital for making three main blood cell types: red, white, and platelets. Red cells carry oxygen, white cells fight infections, and platelets help blood clot.
Our body needs bone marrow to keep making these cells. It replaces old or damaged cells with new ones. This keeps us healthy and prevents issues like anemia and bleeding problems.
Types of Blood Cells Produced in Bone Marrow
The bone marrow makes three main blood cell types:
- Red blood cells: These carry oxygen from our lungs to the rest of our body.
- White blood cells: They help fight infections and diseases.
- Platelets: These small cells help our blood clot when we’re injured.
| Blood Cell Type | Function | Diseases Associated with Dysfunction |
| Red Blood Cells | Carry oxygen throughout the body | Anemia, Sickle Cell Disease |
| White Blood Cells | Fight infections and diseases | Leukemia, Lymphoma |
| Platelets | Help blood to clot | Thrombocytopenia, Bleeding Disorders |
Normal Bone Marrow Function vs. Dysfunction
When bone marrow works right, it makes healthy blood cells efficiently. But, if it doesn’t, it can cause problems like bone marrow suppression and failure.
Many things can cause bone marrow to not work properly, like genetic issues, infections, toxins, and some medicines. Knowing the difference between normal and dysfunctional bone marrow helps doctors diagnose and treat problems.
Bone Marrow Suppression vs. Bone Marrow Failure: Key Differences

It’s important to know the difference between bone marrow suppression and failure. Both affect how the bone marrow makes blood cells. But they have different signs and what they mean for treatment.
Defining Bone Marrow Suppression
Bone marrow suppression means the bone marrow makes fewer blood cells for a while. This can happen from things like chemotherapy, radiation, or some medicines. Bone marrow suppression is often reversible when the cause is fixed.
Defining Bone Marrow Failure Disorders
Bone marrow failure is a more serious issue where the bone marrow can’t make enough blood cells. It can cause big problems like infections, anemia, and bleeding issues. It can be caused by genes, acquired conditions, or toxins.
Temporary vs. Permanent Bone Marrow Damage
The main difference is how long the damage lasts. Suppression is usually short-term, but failure can be permanent. Knowing if it’s temporary or permanent helps decide how to treat it.
We’ll look at what causes, symptoms, and treatments for both in later parts. For now, it’s key to see that they both affect blood cell making but are treated differently.
Common Symptoms and Clinical Manifestations
People with bone marrow issues often face many symptoms. This is because their body makes fewer blood cells. These symptoms can really affect a person’s life and might make them want to see a doctor.
Signs of Decreased Red Blood Cell Production
Not having enough red blood cells leads to anemia. Symptoms include feeling very tired, weak, and short of breath. You might also feel dizzy or lightheaded because your body isn’t getting enough oxygen.
Signs of Decreased White Blood Cell Production
When there are fewer white blood cells, it’s called neutropenia. This makes it harder for your body to fight off infections. Look out for signs like fever, chills, or sore throat. If you notice these, get medical help right away.
Signs of Decreased Platelet Production
Thrombocytopenia means you have fewer platelets. This can cause bleeding problems. You might notice easy bruising, small spots on your skin, or cuts that won’t stop bleeding. In serious cases, it can cause dangerous internal bleeding.
When to Seek Medical Attention
If you’re experiencing symptoms that won’t go away or are getting worse, you should see a doctor. For example, if you have myelosuppression, knowing when to get help is very important. Always watch your health and talk to your doctor if something seems off.
| Symptom | Possible Cause | Action |
| Fatigue, weakness | Anemia (low red blood cells) | Consult a healthcare provider |
| Recurrent infections | Neutropenia (low white blood cells) | Seek immediate medical care |
| Easy bruising, bleeding | Thrombocytopenia (low platelets) | Contact a healthcare provider |
Bone Marrow Suppression Causes: The Four Primary Factors
We find four main reasons for bone marrow suppression and failure. Knowing these is key to diagnosing and treating these complex issues well.
Overview of Major Causative Factors
Bone marrow suppression comes from many sources. These include inherited genetic disorders, acquired conditions, exposure to chemotherapy or radiation, and certain infections or toxins. These can harm the bone marrow’s ability to make blood cells.
“The bone marrow’s failure to produce enough blood cells can severely harm a patient’s health and quality,” say medical experts in hematology.
How These Factors Affect Bone Marrow Function
The four main causes affect bone marrow differently. For example, genetic disorders can cause stem cell problems. Chemotherapy and radiation can stop the bone marrow from regrowing. Acquired conditions, like aplastic anemia, can come from autoimmune reactions or toxins.
It’s vital to understand how these factors harm bone marrow function. This knowledge helps in creating specific treatment plans.
Risk Factors for Developing Bone Marrow Disorders
Some factors raise the risk of bone marrow disorders. These include a family history of genetic issues, exposure to harmful chemicals or toxins, past chemotherapy or radiation, and certain infections. Spotting these risk factors early can lead to better detection and prevention.
By knowing the risk factors and causes of bone marrow suppression, doctors can provide better care and treatment options.
Cause #1: Inherited Genetic Disorders
Understanding the genetic basis of bone marrow failure is key to diagnosing and treating it. Inherited genetic disorders are a major cause of bone marrow failure syndromes. We will look at these disorders, their mechanisms, and how they affect bone marrow.
Fanconi Anemia and Its Mechanisms
Fanconi anemia is a rare genetic disorder. It causes bone marrow failure, birth defects, and a higher risk of cancer. It’s caused by mutations in genes that fix DNA damage.
The diagnosis of Fanconi anemia is critical because it severely impacts bone marrow function and overall health.
Research on Fanconi anemia has shed light on its genetic causes. Studies show that FA gene mutations lead to unstable chromosomes. This makes it hard for bone marrow to produce blood cells.
Dyskeratosis Congenita
Dyskeratosis congenita is another inherited disorder that affects bone marrow. It’s known for its oral leukoplakia, nail dystrophy, and skin hyperpigmentation. The condition is linked to telomere maintenance gene mutations, causing premature telomere shortening and bone marrow failure.
Shwachman-Diamond Syndrome
Shwachman-Diamond syndrome is a rare disorder. It causes pancreatic insufficiency, bone marrow dysfunction, and skeletal issues. It’s caused by mutations in the SBDS gene, affecting ribosome biogenesis and hematopoietic stem cell function.
Other Hereditary Bone Marrow Failure Syndromes
Other inherited genetic disorders can also cause bone marrow failure. These include Diamond-Blackfan anemia and severe congenital neutropenia. Each has unique genetic and clinical features needing specific treatments.
| Disorder | Primary Characteristics | Genetic Basis |
| Fanconi Anemia | Bone marrow failure, congenital abnormalities, increased cancer risk | Mutations in FA genes |
| Dyskeratosis Congenita | Mucocutaneous features, bone marrow failure | Mutations in telomere maintenance genes |
| Shwachman-Diamond Syndrome | Pancreatic insufficiency, bone marrow dysfunction, skeletal abnormalities | Mutations in the SBDS gene |
Cause #2: Acquired Bone Marrow Conditions
We will look at different acquired conditions that affect bone marrow. These include their causes and how they impact health. These disorders can lead to a decrease in blood cell production. They can be caused by autoimmune diseases, toxins, and infections.
Aplastic Anemia: Mechanisms and Risk Factors
Aplastic anemia is when the bone marrow can’t make blood cells. This happens because the stem cells in the marrow get damaged. As a result, the body doesn’t get enough red blood cells, white blood cells, and platelets.
The causes of aplastic anemia include autoimmune diseases, toxins, and viral infections.
Risk factors for developing aplastic anemia include:
- Exposure to chemicals such as pesticides and benzene
- Certain viral infections, including hepatitis and HIV
- Autoimmune disorders
- Previous chemotherapy or radiation therapy
A medical expert notes, “Aplastic anemia is a serious condition. It needs quick medical care to manage symptoms and prevent problems.”
Myelodysplastic Syndromes (MDS)
Myelodysplastic syndromes (MDS) are disorders where blood cells don’t form right. This leads to bone marrow failure. MDS can turn into more serious diseases like acute myeloid leukemia (AML).
MDS is caused by genetic changes in bone marrow stem cells. This makes blood cell production ineffective. Risk factors include radiation, chemicals, and previous chemotherapy.
Paroxysmal Nocturnal Hemoglobinuria (PNH)
Paroxysmal nocturnal hemoglobinuria (PNH) is a rare disease. It causes red blood cell destruction, bone marrow failure, and blood clots. It’s caused by mutations in the PIGA gene, important for blood cell proteins.
PNH symptoms include red blood cell destruction. This can be triggered by infections and some medicines. Treating PNH involves stopping red blood cell destruction, preventing blood clots, and treating bone marrow failure.
Autoimmune-Mediated Bone Marrow Suppression
Autoimmune bone marrow suppression happens when the immune system attacks the bone marrow. This leads to fewer blood cells. It can cause anemia, neutropenia, and thrombocytopenia.
The exact reasons for this are complex. They involve genetics and environmental factors. Treatment usually involves immunosuppressive therapy to stop the immune system’s attack.
“Understanding the causes of bone marrow suppression is key to finding effective treatments,” say healthcare professionals.
Cause #3: Chemotherapy and Radiation Exposure
Chemotherapy and radiation can harm bone marrow in cancer patients. These treatments are key in fighting cancer, but can also have side effects on bone marrow.
How Cancer Treatments Affect Bone Marrow
Chemotherapy targets fast-growing cells, including cancer and bone marrow cells. This can lower the production of blood cells. This leads to anemia, neutropenia, and thrombocytopenia.
Radiation therapy can also damage bone marrow, which is more likely in areas like the pelvis or spine. The damage’s extent depends on the radiation dose and area.
Myelosuppressive Effects of Different Chemotherapy Agents
Chemotherapy agents vary in how much they suppress bone marrow. For example, alkylating agents and anthracyclines are very myelosuppressive. This can affect treatment plans, sometimes needing adjustments or extra support.
| Chemotherapy Agent | Myelosuppressive Effect |
| Alkylating Agents | High |
| Anthracyclines | High |
| Antimetabolites | Moderate |
Radiation-Induced Bone Marrow Damage
Radiation can cause immediate or long-term damage to bone marrow. High doses can permanently harm it, while lower doses might allow recovery. The bone marrow’s ability to regenerate is key to recovery.
Recovery Timeline After Treatment
Recovery time after chemotherapy and radiation varies. Bone marrow function starts to recover a few weeks after treatment ends. But full recovery can take months. Recovery depends on treatment type, dose, and individual factors.
Supportive care, like hematopoietic growth factors, can help manage myelosuppression. It supports bone marrow recovery.
Cause #4: Infections and Toxic Exposures
Infections and toxic exposures can harm bone marrow, leading to suppression or failure. The bone marrow’s role in making blood cells is at risk from pathogens and toxins. It’s important to understand these threats well.
Viral Infections That Target Bone Marrow
Some viruses directly harm bone marrow function. For example, parvovirus B19 can stop red blood cell production, causing severe anemia. Viruses like hepatitis viruses and HIV can also affect bone marrow, either directly or through the immune system.
Viruses can harm bone marrow in different ways. Some directly infect blood-making cells. Others trigger an immune response that damages the bone marrow. Knowing how viruses work is key to finding new treatments.
Bacterial Infections and Bone Marrow Suppression
Bacterial infections can also harm bone marrow, often by releasing inflammatory substances that slow blood cell production. For example, tuberculosis and brucellosis can lead to low blood cell counts. How much bone marrow is affected depends on the infection’s severity and length.
Environmental Toxins and Chemical Exposures
Exposure to certain toxins and chemicals can harm bone marrow. Benzene, for instance, can cause bone marrow failure. Pesticides and some industrial solvents can also suppress bone marrow.
| Toxin/Chemical | Effect on Bone Marrow |
| Benzene | Bone marrow failure, aplastic anemia |
| Pesticides | Variable effects, including cytopenias |
| Industrial solvents | Bone marrow suppression, aplastic anemia |
Medication-Induced Bone Marrow Depression
Some medications can depress bone marrow as a side effect. Chemotherapy agents target fast-growing cancer cells but also affect bone marrow cells. Other drugs, like certain antibiotics and anti-inflammatory drugs, can also suppress bone marrow, but less predictably.
It’s important to watch for signs of bone marrow suppression in patients on these medications. Early detection can help manage the condition and prevent serious problems.
Diagnosis and Evaluation of Bone Marrow Disorders
Bone marrow disorders can be hard to diagnose. But there are several methods to help identify them. Accurate diagnosis is key to finding the right treatment.
Blood Tests and Complete Blood Count Analysis
Blood tests, including a complete blood count (CBC), are often the first step. A CBC checks the levels of different blood cells. This gives clues about how well the bone marrow is working.
Abnormal cell counts can mean the bone marrow is not working properly. For example, low red blood cells can lead to anemia. Low white blood cells can make you more prone to infections.
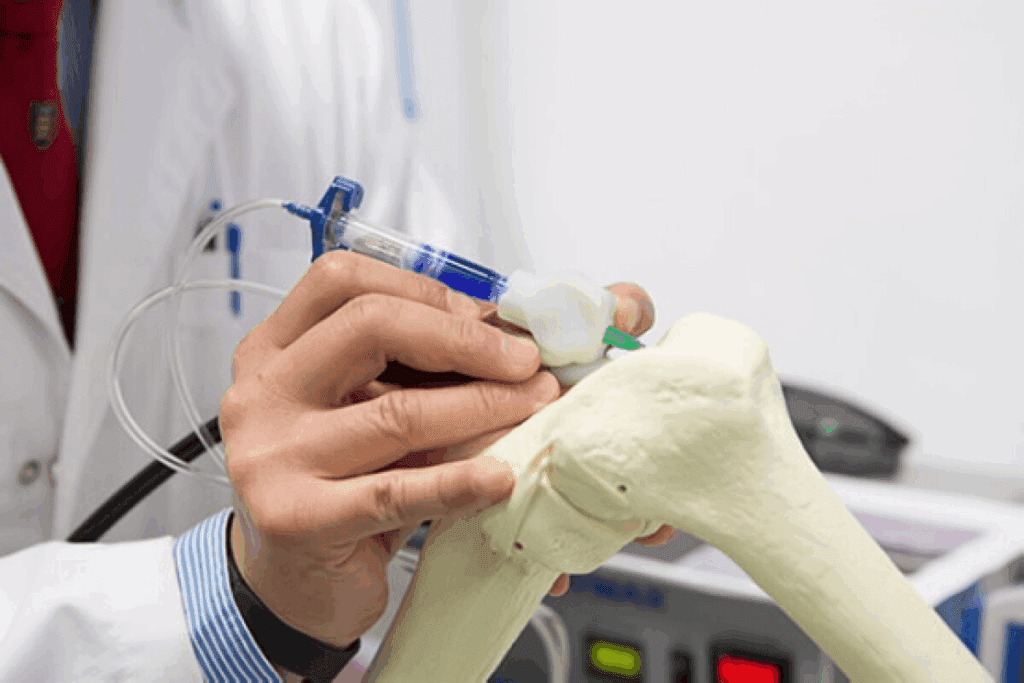
Bone Marrow Aspiration and Biopsy
If blood tests show a problem, a bone marrow aspiration and biopsy are done. These procedures take a sample of bone marrow for examination.
The aspiration looks at the cells in the marrow. The biopsy checks the marrow’s structure and any scarring.
Genetic Testing for Inherited Disorders
Genetic testing is key for inherited bone marrow failure syndromes. It looks at the patient’s DNA for specific mutations.
This testing confirms the diagnosis, helps decide treatment, and guides genetic counseling for families.
Differential Diagnosis Considerations
When diagnosing bone marrow disorders, it’s important to consider many possibilities. Doctors look at both inherited and acquired conditions, infections, and toxin exposure.
| Diagnostic Method | Purpose | Key Findings |
| Complete Blood Count (CBC) | Measures levels of different blood cells | Abnormal cell counts indicate marrow dysfunction |
| Bone Marrow Aspiration | Assesses cellularity and morphology of marrow cells | Presence of abnormal cells or inadequate cellularity |
| Bone Marrow Biopsy | Examines the structure of the bone marrow | Fibrosis, scarring, or abnormal architecture |
| Genetic Testing | Identifies genetic mutations associated with inherited syndromes | Specific genetic mutations confirming inherited conditions |
Treatment Approaches and Management Strategies
Managing bone marrow disorders well needs a detailed treatment plan. We will look at the different ways to treat bone marrow suppression and failure.
Supportive Care Measures
Supportive care is key in handling bone marrow disorders. It helps ease symptoms and improve life quality for patients. We give blood transfusions for anemia and thrombocytopenia. We also use antibiotics to fight infections.
Key Supportive Care Measures:
- Blood transfusions
- Antibiotic therapy
- Growth factor support
- Nutritional support
Hematopoietic Growth Factors
Hematopoietic growth factors boost blood cell production in the bone marrow. We use them to treat anemia, neutropenia, and thrombocytopenia caused by bone marrow suppression.
| Growth Factor | Function | Clinical Use |
| Erythropoietin | Stimulates red blood cell production | Treatment of anemia |
| Granulocyte-Colony Stimulating Factor (G-CSF) | Stimulates white blood cell production | Prevention and treatment of neutropenia |
| Thrombopoietin | Stimulates platelet production | Treatment of thrombocytopenia |
Immunosuppressive Therapy
In some cases of bone marrow failure, we use immunosuppressive therapy. This therapy calms the immune system’s attack on the bone marrow. We use drugs like cyclosporine and anti-thymocyte globulin for this.
Stem Cell Transplantation
Stem cell transplantation can be a cure for some bone marrow failure disorders. We use it to replace damaged bone marrow with healthy stem cells from a donor.
Types of Stem Cell Transplantation:
- Allogeneic transplantation (from a donor)
- Autologous transplantation (using the patient’s own stem cells)
Understanding the different treatments helps us give the best care to patients with bone marrow disorders.
Conclusion: Prognosis and Living with Bone Marrow Disorders
Knowing the prognosis of bone marrow disorders is key for both patients and doctors. The outlook changes a lot based on the cause and how severe it is. For example, people with genetic disorders face different issues than those with acquired ones.
Dealing with bone marrow failure needs a lot of care and support. We stress the need for a team effort to handle symptoms, avoid problems, and boost life quality. Treatments like supportive care, growth factors, and stem cell transplants are very important.
Thanks to new medical treatments, the outlook for bone marrow disorder patients has gotten better. Every patient’s path is different. The outcome depends on the cause, how severe it is, and how well they respond to treatment. By tailoring care to each person, we can improve their life ty and prognosis.
FAQ
What is bone marrow failure?
Bone marrow failure happens when the bone marrow can’t make enough blood cells. This includes red blood cells, white blood cells, and platelets. It leads to health problems.
What are the main causes of bone marrow suppression and failure?
Main causes include genetic disorders, acquired conditions, and exposure to chemotherapy or radiation. Certain infections or toxins also play a role.
How do genetic disorders affect bone marrow function?
Genetic disorders like Fanconi anemia and dyskeratosis congenita can cause bone marrow failure. They affect blood cell production due to inherited genetic mutations.
What are the symptoms of bone marrow suppression and failure?
Symptoms depend on the blood cells affected. They can include fatigue, infections, and bleeding disorders. This is because of low production of red blood cells, white blood cells, and platelets.
How is bone marrow failure diagnosed?
Diagnosis involves blood tests and bone marrow aspiration, a biopsy. Genetic testing is also used to check the bone marrow’s function and find the cause.
What are the treatment options for bone marrow suppression and failure?
Treatments include supportive care, hematopoietic growth factors, and immunosuppressive therapy. Stem cell transplantation may also be considered, based on the cause and severity.
Can bone marrow function recover after chemotherapy or radiation treatment?
Yes, bone marrow function can recover after treatment. The recovery time depends on the treatment type and intensity.
How do infections and toxins affect bone marrow function?
Infections and toxins can harm bone marrow cells or disrupt their production. This leads to a decrease in blood cell production.
What is the prognosis for patients with bone marrow disorders?
The prognosis varies based on the cause, severity, and treatment response. It highlights the need for thorough care and support for patients.
Are there any preventive measures for bone marrow suppression and failure?
Preventive measures include avoiding toxins, managing infections quickly, and careful use of chemotherapy and radiation. Some causes are unavoidable, but these steps can help.
References:
- Young, N. S. (1995). Bone marrow failure: Pathophysiology and management. Blood, 85(10), 2758-2776. Retrieved from https://pubmed.ncbi.nlm.nih.gov/7698059/
- Fassel, H., & Sheth, S. (2020). Bone marrow failure in children: Approach to diagnosis and treatment. Indian Journal of Pediatrics, 87(2), 141-149. Retrieved from https://thalassemia.weill.cornell.edu/research/publications/bone-marrow-failure-children-approach-diagnosis-and-treatment