
Choosing to have a bone marrow transplant is a big step. It’s important to know the possible risks and side effects. As a top healthcare provider, we aim to offer the best care. We also provide support and guidance to patients from around the world.
At Liv Hospital, we know that a bone marrow transplant is a lifesaving but complex treatment. It comes with risks and side effects that can last a long time. Spotting the signs of transplant problems early is key to better survival chances.
We want to help you understand this complex process better. In this article, we’ll talk about the main risks and side effects of transplant failure. These include ongoing low blood counts, infections, and bleeding.

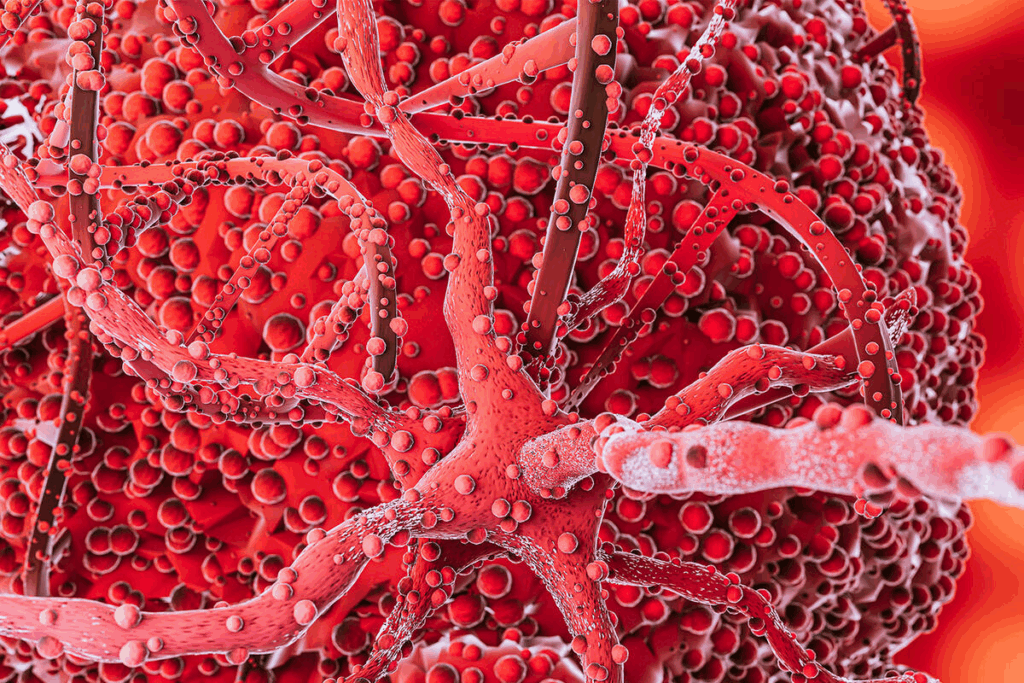
A bone marrow transplant, also known as a stem cell transplant, is a complex process. It replaces a patient’s bone marrow with healthy cells. This is key for those with certain cancers, blood disorders, or immune system diseases.
This transplant involves putting healthy stem cells into a patient’s body. The goal is to replace damaged or diseased bone marrow. It helps the patient make healthy blood cells again.
Transplants can be based on the source of the stem cells and the donor’s genetic match with the patient.
There are several types of bone marrow transplants. Here are a few:
Each type has its own considerations and possible complications.
| Type of Transplant | Donor Source | Key Considerations |
| Autologous | Patient’s own cells | Lower risk of GVHD, but could reinfuse malignant cells |
| Allogenic | Related or unrelated donor | Higher risk of GVHD, but can fight cancer |
| Syngeneic | Identical twin | Lowest risk of GVHD, but rare due to the need for an identical twin |
The transplant process has several steps. First, patients prepare with chemotherapy and/or radiation to destroy the diseased bone marrow.
Then, they receive the infused stem cells. These cells go to the bone marrow and start making new blood cells. The time after the transplant is critical, with risks of infection and GVHD.
Transplant failure is rare but serious. It’s when the new cells don’t make blood cells. Knowing these risks and the transplant process helps manage expectations and improve outcomes.
It’s important for patients and caregivers to know the early signs of bone marrow transplant failure. This knowledge helps ensure quick medical help. Early detection can greatly improve patient outcomes.
Failure of a bone marrow transplant can show in many ways. Knowing these signs is key to managing the condition well. Look out for problems with blood counts, infections, bleeding, and how the bone marrow works.
Low blood counts are a big warning sign of transplant failure. This can cause severe anemia, thrombocytopenia, and neutropenia. These conditions make patients more likely to get infections and bleed easily.
Low blood counts happen when the bone marrow can’t make enough blood cells. This might need transfusions to manage. It’s vital to check blood counts often to spot any problems early.
| Blood Component | Normal Range | Low Count Implications |
| White Blood Cells (WBC) | 4,500 – 11,000 cells/μL | Increased infection risk |
| Red Blood Cells (RBC) | 4.32 – 5.72 million cells/μL (male) | Anemia, fatigue |
| Platelets | 150,000 – 450,000 cells/μL | Bleeding, bruising |
Getting infections again and again, even with treatment, is a big warning sign. Patients with weak immune systems are at high risk for serious infections.
It’s important to watch for signs of infection like fever, chills, and cough. If these happen, get medical help right away.
Seeing unusual bleeding or bruising can mean bone marrow transplant failure. This often comes from low platelet counts or platelet problems. Patients might notice easy bruising, prolonged bleeding from cuts, or spontaneous bleeding.
Managing these symptoms usually means getting platelet transfusions. It’s also about finding and fixing the cause of the bleeding or bruising.
When the transplanted bone marrow doesn’t start making new blood cells, it’s a big problem. This can lead to long-lasting low blood counts and higher risks of infections and bleeding.
We work closely with patients to track engraftment. We use bone marrow biopsies and blood count checks to adjust treatment plans as needed. This helps support recovery.
Knowing these early warning signs helps patients and caregivers get help quickly. This can make a big difference in how well a bone marrow transplant goes.
Bone marrow transplantation comes with a big risk: infections. This is because the treatment weakens the immune system. This makes patients more open to many kinds of germs.
Bacterial infections are a big worry for those getting bone marrow transplants. These can cause sepsis, a serious condition where the body attacks itself. It’s very important to catch and treat these infections early to avoid sepsis.
These infections often start in the skin, lungs, or gut. Doctors often use strong antibiotics to prevent them. But this can sometimes make germs resistant to treatment.
Viruses like CMV, EBV, and HSV can wake up in patients after a transplant. Keeping an eye on these viruses and using antiviral drugs is key to managing this risk.
These viruses can cause serious problems, like damage to organs. For example, CMV can lead to lung or gut diseases. EBV can cause a type of cancer called PTLD.
Fungal infections are a big danger for those with weakened immune systems. Fungi like Aspergillus and Candida can cause serious infections. Using antifungal drugs and starting treatment early is vital to stop these infections.
People at risk include those with long-lasting low white blood cell counts, those on strong antibiotics, and those with GVHD. To protect them, doctors often give them antifungal drugs.
Stopping infections is a big part of taking care of someone after a transplant. Ways to do this include using medicines to prevent infections, keeping everything clean, and watching for signs of infection.
| Prevention Strategy | Description | Benefit |
| Prophylactic Antimicrobials | Use of antibiotics, antivirals, and antifungals to prevent infections | Reduces the risk of life-threatening infections |
| Infection Control Practices | Strict hygiene practices, isolation when necessary | Minimizes exposure to pathogens |
| Monitoring for Infection | Regular checks for signs of infection | Enables early detection and treatment |
Managing blood-related complications after a bone marrow transplant is a big challenge. These issues can really affect a patient’s life and recovery. We watch patients closely for these problems to act quickly.
Severe anemia is a big problem after a bone marrow transplant. It causes fatigue, weakness, and shortness of breath. Anemia happens when the body has too few red blood cells, often because of a transplant or a disease that requires a transplant. We treat anemia with transfusions and medicines that help make more red blood cells.
Thrombocytopenia, or low platelet count, raises the risk of bleeding and hemorrhage. Patients with thrombocytopenia might get bruises, nosebleeds, or bleeding gums. To lower this risk, we give platelet transfusions and keep a close eye on patients for bleeding signs.
Neutropenia, with a low neutrophil count, makes infections more likely. Neutropenia can come from the conditioning before the transplant or the transplant itself. We fight neutropenia with isolation, antibiotics, and medicines that boost neutrophil production.
Transfusions are key to handling blood issues after a bone marrow transplant. Red blood cell transfusions help with anemia, and platelet transfusions lower bleeding risk. We manage transfusions carefully to keep our patients safe and healthy.
GVHD is a big problem in bone marrow transplants. It happens when the donor’s immune cells see the recipient as foreign. Then, they attack the host’s tissues.
Acute GVHD starts within the first 100 days after the transplant. It can be mild or very severe. It affects the skin, liver, and stomach.
Chronic GVHD starts after 100 days. It can affect many parts of the body. Symptoms can vary a lot.
Preventing and managing GVHD is complex. It involves several steps:
| Strategy | Description |
| Immunosuppressive Therapy | Drugs to suppress the immune system and prevent GVHD |
| T-Cell Depletion | Removing T-cells from the graft to lower GVHD risk |
| Supportive Care | Managing GVHD symptoms and complications |
GVHD can really affect a person’s life after a bone marrow transplant. Chronic GVHD can cause long-term problems. We help patients find ways to deal with GVHD and improve their quality.
The conditioning regimen for bone marrow transplants can lead to mucositis and various gastrointestinal complications. These issues significantly impact patients’ quality of life and nutritional status.
Oral mucositis is a common and painful side effect of the conditioning regimen. It causes inflammation and ulceration of the mucous membranes in the mouth. This condition makes eating, drinking, and speaking difficult.
We manage oral mucositis through a combination of pain relief medications, oral care protocols, and nutritional support.
Management Strategies for Oral Mucositis:
Gastrointestinal complications can result in significant nutritional challenges. Patients may experience nausea, vomiting, diarrhea, and malabsorption. These issues can lead to weight loss and malnutrition.
We address these challenges through personalized nutritional plans. These plans often involve dietary adjustments and supplements.
| Nutritional Challenge | Management Approach |
| Nausea and Vomiting | Antiemetic medications, dietary adjustments |
| Diarrhea | Fluid replacement, electrolyte supplements |
| Malabsorption | Nutritional supplements, parenteral nutrition |
Diarrhea and malabsorption are frequent gastrointestinal complications following bone marrow transplantation. These issues can lead to dehydration, electrolyte imbalances, and malnutrition if not properly managed.
We monitor patients closely and implement appropriate interventions. These include fluid replacement and nutritional support.
Effective management of mucositis and gastrointestinal complications requires a multidisciplinary approach. This includes pain management, nutritional support, and infection prevention.
We work closely with patients to develop personalized care plans. These plans address their specific needs and minimize the risk of complications.
Key Components of Management:
After a bone marrow transplant, organs can face toxicity and dysfunction. The treatment needed for the transplant can harm different parts of the body. This can lead to serious problems.
Hepatic issues, like Veno-Occlusive Disease (VOD) and Sinusoidal Obstruction Syndrome (SOS), are big worries. These happen when liver veins get blocked, causing liver problems.
Symptoms to watch for: Weight gain, ascites, hepatomegaly, and jaundice.
The treatment can also harm the heart, leading to heart failure. This is a big worry for those with heart issues before the transplant.
Monitoring cardiac function through regular echocardiograms and MUGA scans is essential for early detection.
| Cardiac Complication | Symptoms | Management |
| Heart Failure | Shortness of breath, fatigue, swelling | Diuretics, ACE inhibitors |
| Cardiac Arrhythmias | Palpitations, dizziness | Anti-arrhythmic medications |
Renal insufficiency is another risk, caused by the treatment’s toxicity or infections, and GVHD.
“Renal function monitoring is critical in the post-transplant period to prevent long-term damage.”
-As advised by doctors.
Managing this involves adjusting medication and keeping the patient hydrated.
In severe cases, the damage to organs can cause multi-organ failure. This is a serious condition that needs intensive care.
Prevention is key, with careful patient selection, monitoring, and managing complications.
Bone marrow transplant patients often face lung problems. These issues can make recovery harder and affect their quality of life. We focus on watching and managing these risks to give the best care.
Interstitial pneumonitis occurs when lung tissue becomes inflamed. It can happen due to infections, meds, or GVHD. Symptoms include cough, shortness of breath, and fever. We use detailed tests to find the cause and treat it correctly.
Bronchiolitis obliterans makes the small airways in the lungs inflamed and scarred. It’s linked to chronic GVHD. We help patients manage symptoms and slow the disease with meds and lifestyle changes.
Pulmonary edema is when fluid builds up in the lungs. It can be caused by heart problems, too much fluid, or toxic effects from treatments. Symptoms include trouble breathing and chest pain. Our team quickly works to ease symptoms and find the cause.
Respiratory failure is a serious condition that can happen from severe lung problems. It needs quick medical help and often involves using a breathing machine. We aim to give timely and effective treatment to help patients through this tough time.
Pulmonary issues can greatly affect bone marrow transplant outcomes. Knowing these risks and working with our healthcare team can help lessen them. This can improve patient results.
| Pulmonary Complication | Common Causes | Symptoms | Management Approach |
| Interstitial Pneumonitis | Infections, medications, GVHD | Cough, shortness of breath, fever | Comprehensive diagnostics, tailored treatment |
| Bronchiolitis Obliterans | Chronic GVHD | Shortness of breath, wheezing | Medications, lifestyle adjustments |
| Pulmonary Edema | Cardiac dysfunction, fluid overload, toxicity | Difficulty breathing, chest discomfort | Prompt intervention, addressing the underlying cause |
| Respiratory Failure | Severe pulmonary complications | Severe difficulty breathing | Mechanical ventilation, intensive care |
“The management of pulmonary complications after bone marrow transplantation requires a multidisciplinary approach, combining the expertise of pulmonologists, transplant specialists, and other healthcare professionals to provide complete care.”
Expert in Transplant Care
Patients going through bone marrow transplants face serious neurological issues. These problems can affect their health in the short and long term. The treatment process, known as conditioning, can harm the nervous system and brain function.
The treatment’s high-dose chemotherapy and radiation can lead to neurotoxicity. This can cause symptoms like confusion, seizures, and even encephalopathy. We watch for these signs closely to act quickly.
Seizures might happen due to the treatment’s toxicity or imbalances in electrolytes. Encephalopathy, which affects mental status, also requires careful handling. This is to avoid lasting brain damage.
Many patients struggle with cognitive impairment, known as “chemo brain.” This makes it hard to remember, focus, and process information. While some issues may go away, others can last, needing ongoing support.
Peripheral neuropathy is nerve damage that causes pain, numbness, and weakness in limbs. It can come from some chemotherapy drugs. We help patients manage symptoms to improve their life quality.
The side effects on the brain and nerves from bone marrow transplants highlight the need for detailed care. By knowing these risks, we can help patients more during their treatment. This helps keep their health and well-being in check.
The journey after a bone marrow transplant comes with its own set of challenges. While it can save lives, it’s important for patients and their caregivers to know the risks. These can show up months or years later.
One big risk is getting secondary malignancies, or new cancers. These can include:
Seeing a healthcare provider regularly is key to catching these issues early.
Endocrine dysfunction is another common problem. It affects glands that make hormones, which are vital for our bodies. This can cause issues like:
We team up with endocrinologists to manage these issues and help patients live better lives.
Fertility is a big worry for those getting bone marrow transplants. The treatment can harm reproductive organs, leading to infertility or early menopause. We talk about ways to preserve fertility before the transplant, if possible.
Patients need to understand that:
Osteoporosis and avascular necrosis are also long-term problems. They can affect bone health due to the transplant and certain medications like corticosteroids.
“The risk of osteoporosis and avascular necrosis highlights the need for long-term care after a bone marrow transplant.”
-Specialists’ note.
We focus on prevention and early treatment to manage these bone issues well.
The psychological effects of a bone marrow transplant can be deep. It affects many parts of a patient’s life. The treatment, though lifesaving, is tough. It includes long stays in isolation and the risk of serious problems.
Patients often face mental health issues like post-traumatic stress and anxiety. The treatment’s intensity and the unknown outcomes cause a lot of emotional pain.
Signs of post-traumatic stress include flashbacks, high anxiety, and avoiding transplant reminders. To manage these, patients might need therapy and sometimes medicine.
Many patients feel tired all the time after a transplant. This tiredness makes it hard to do things they used to enjoy. It affects their quality of life a lot.
To fight chronic fatigue, doctors use graded exercise therapy and cognitive behavioral therapy. These help increase energy and improve daily functioning.
The transplant can change how patients see themselves and their relationships. Treatment side effects like hair loss or weight changes can hurt self-esteem.
It also puts a strain on relationships with loved ones. Support groups and counseling help patients deal with these changes and keep their relationships strong.
Finding ways to cope is key to dealing with the transplant’s mental effects. This includes getting help from professionals, doing things that relax you, and getting support from family, friends, and groups.
| Coping Strategy | Description | Benefits |
| Professional Support | Access to psychologists and counselors for individual or group therapy | Provides tools to manage anxiety, depression, and PTSD |
| Stress Reduction Techniques | Meditation, yoga, and other practices to reduce stress | Improves mental well-being and resilience |
| Support Groups | Connecting with others who have experienced similar challenges | Reduces feelings of isolation, fosters community |
Using these strategies, patients can handle the mental challenges of bone marrow transplants better. This improves their overall quality of life.
Managing bone marrow transplant complications is key to good results. We’ve talked about the risks and side effects, like infections and GVHD. These can affect organs and the brain, too.
Keeping an eye on these issues helps doctors catch problems early. This way, they can act fast. Patients can also understand what to expect better.
We aim to give top-notch care and support to reduce these complications. It’s a team effort, and we work with patients to create care plans that fit them.
By focusing on monitoring and managing these issues, we can make patients’ lives better. This improves their health and happiness.
Common risks and side effects include infections and low blood counts. Severe anemia and thrombocytopenia are also common. Graft-versus-host disease (GVHD) and organ toxicity are other risks.
Symptoms include low blood counts and infections. Unusual bleeding and delayed engraftment are also signs. These symptoms show the transplant may not be working.
To prevent infections, antibiotics, antivirals, and antifungals are used. Strict infection control is also key. This includes isolation and good hygiene.
GVHD happens when the donor’s immune cells attack the recipient’s body. To manage it, immunosuppressive drugs are used. Monitoring and supportive care help reduce symptoms and prevent damage.
Blood complications include severe anemia and low platelet counts. These can cause fatigue, bleeding, and infections. There are serious risks after a transplant.
Managing these complications involves pain relief and nutrition support. Medications help reduce symptoms. This approach aims to lessen discomfort and improve recovery.
Organ toxicity can harm the liver, heart, kidneys, and more. It’s caused by the conditioning regimen. These risks can lead to serious organ damage or failure.
Organ toxicity can harm the liver, heart, kidneys, and more. It’s caused by the conditioning regimen. These risks can lead to serious organ damage or failure.
Organ toxicity can harm the liver, heart, kidneys, and more. It’s caused by the conditioning regimen. These risks can lead to serious organ damage or failure.
Side effects include neurotoxicity and seizures. Encephalopathy, cognitive impairment, and neuropathy are also possible. These can affect the brain and nervous system.
Long-term complications include secondary cancers and endocrine issues. Fertility problems, osteoporosis, and avascular necrosis are also risks. These can affect health years after the transplant.
Managing the psychological impact involves counseling and stress management. Support groups help too. These strategies aim to improve mental health and quality of life.
Complications include graft failure and GVHD. Infections and organ toxicity are also risks. These can affect the success and safety of the transplant.
Side effects include pain, infection, and bleeding at the injection site. These can be uncomfortable and may require medical attention.
Risks can be minimized by careful patient selection and donor matching. Meticulous post-transplant care is also key. This includes preventing infections and managing GVHD.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us