Did you know that complications from bowel surgery can sometimes affect other parts of the body, including the bladder? This unexpected connection can lead to various urinary issues. It sparks concern among patients undergoing such procedures. Discussing how bowel surgery cause bladder problems can occur due to temporary or permanent nerve damage.
The relationship between bowel resection and bladder function is complex. Research shows that certain types of colon surgery may lead to bladder dysfunction. This is because the bladder is close to the surgical site.
Understanding the risks and complications of bowel surgery is key for both patients and healthcare providers.
Key Takeaways
- Bowel surgery can potentially lead to bladder problems.
- The risk of bladder complications varies depending on the type of colon surgery.
- Patients should discuss possible risks with their healthcare provider.
- Bladder dysfunction may occur due to the proximity of the bladder to the surgical site.
- Understanding the risks can help in managing expectations and outcomes.
The Anatomical Connection Between Bowel and Bladder
Exploring the connection between the bowel and bladder shows why surgery in the bowel can affect the bladder. The pelvic area is complex, with vital organs like the bowel and bladder close together.
Proximity of Structures in the Pelvic Cavity
The bowel and bladder are in the same pelvic area. This means surgery in one can impact the other. The proximity of these structures raises the risk of bladder problems during bowel surgery.
- The rectum and bladder are next to each other in the pelvic area.
- Surgery in the bowel can harm the bladder because they are so close.
Shared Nerve Pathways and Innervation
The bowel and bladder share nerve paths that can be damaged in bowel surgery. The autonomic nervous system is key for both organs. Damage to these nerves can cause urinary issues.
- The inferior hypogastric plexus is a main nerve network for both organs.
- It’s important to protect these nerves during surgery to avoid bladder problems.
Fascial and Ligament Relationships
The fascial and ligamentous structures in the pelvis support both the bowel and bladder. Knowing these relationships helps surgeons avoid bladder issues during bowel surgery.
- The pelvic fascia wraps around both organs, providing support.
- Ligaments like the pubovesical ligament help keep the pelvic organs in place.
Types of Bowel Surgery That Commonly Affect Bladder Function
Some bowel surgeries can harm the bladder, causing urinary problems. It is essential for both patients and doctors to be informed about these surgeries to better manage bladder issues.
Colorectal Resection Procedures
Colorectal resection removes parts of the colon or rectum. It’s often for cancer or severe diverticulitis. This surgery can mess with the bladder because of its close location and shared nerves.
- Anterior Resection: Taking out part of the rectum can harm nerves that control the bladder.
- Low Anterior Resection: This surgery removes the lower rectum. It can cause bladder problems due to nerve damage.
Small Intestine Surgical Interventions
Operations on the small intestine can also affect the bladder. These surgeries are complex and can cause inflammation or adhesions. This increases the risk of bladder issues.
- Small Bowel Resection: Removing a part of the small intestine can change the pelvic area. This might affect the bladder.
- Adhesion Removal: Surgery to remove adhesions in the small intestine can sometimes cause or worsen bladder problems.
Inflammatory Bowel Disease Operations
Surgeries for inflammatory bowel disease (IBD) can also harm the bladder. The surgery’s extent and complications like fistulas can raise the risk of bladder problems.
- J-Pouch Surgery: Making a pouch from the small intestine for stool can sometimes cause urinary issues.
- Colectomy: Removing the colon can affect the bladder, mainly if there’s a lot of pelvic dissection.
Cancer-Related Bowel Surgeries
Cancer surgeries for the bowel can significantly affect the bladder. The surgery’s extent, the involvement of nearby tissues, and adjuvant therapies like radiation can lead to bladder issues.
- Radical Resection: Removing a lot of cancerous tissue can damage nerves and affect bladder control.
- Cytoreductive Surgery: Removing as much cancer as possible can involve complex pelvic surgery. This can impact bladder function.
Common Bladder Problems Following Bowel Surgery
Bowel surgery can lead to bladder issues. Patients may face urinary problems that affect their daily life.
Urinary Retention and Voiding Difficulties
Urinary retention is a common problem after bowel surgery. It makes it hard to empty the bladder fully. This can cause discomfort and serious issues if not treated.
- Difficulty starting to urinate
- Struggling to urinate
- Feeling like the bladder isn’t fully empty
Urinary Incontinence Types
Urinary incontinence can also occur after bowel surgery. It includes stress incontinence, where movement causes leakage, and urge incontinence, needing to urinate suddenly.
- Stress urinary incontinence
- Urge urinary incontinence
- Mixed urinary incontinence
Recurrent Urinary Tract Infections
Patients may get recurrent urinary tract infections (UTIs) after bowel surgery. These infections can be painful and may need antibiotics.
- Frequent UTIs
- Dysuria (painful urination)
- Urinary urgency and frequency
Overactive Bladder Syndrome
Overactive bladder syndrome makes you feel a sudden, strong urge to urinate. It can be distressing and disrupt daily activities.
Symptoms include:
- Urinary urgency
- Frequent urination
- Nocturia (waking up to urinate at night)
How Can Bowel Surgery Cause Bladder Problems: Mechanisms Explained
Bowel surgery can affect the bladder in many ways. It’s because of the surgery’s close location to the bladder and shared nerve paths.
Direct Nerve Damage During Surgical Dissection
Direct nerve damage is a major cause. The nerves that control the bladder are near where bowel surgery happens. Damage to these nerves can cause urinary retention and incontinence.
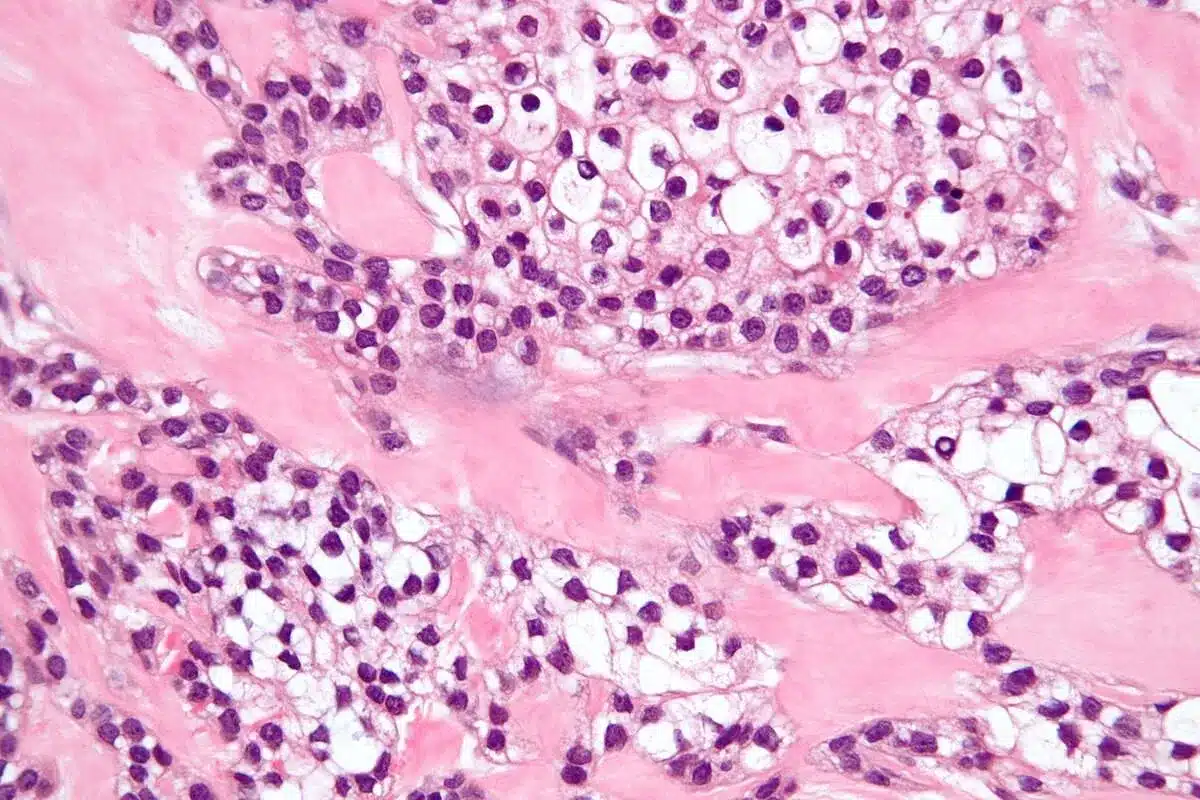
Inflammatory and Immune Responses
The body reacts to surgery with inflammation and immune responses. This can harm the bladder. Inflammation can cause scarring and adhesions that affect bladder function. The immune response can also damage nearby tissues.
Adhesions and Scar Tissue Formation
After bowel surgery, adhesions and scar tissue form. These can change the pelvic area’s shape. This can put pressure on the bladder or block its function. Symptoms like frequent urination, urgency, or trouble voiding can occur.
Changes in Pelvic Floor Support
Bowel surgery can also change the pelvic floor’s support. The pelvic floor muscles support both the bowel and bladder. Surgery can alter this support, leading to bladder problems like incontinence or voiding issues.
Mechanism | Effect on Bladder Function | Potential Symptoms |
Direct Nerve Damage | Impaired nerve control | Urinary retention, incontinence |
Inflammatory Responses | Scarring and adhesions | Frequency, urgency, voiding difficulty |
Adhesions and Scar Tissue | Distorted pelvic anatomy | Obstructed voiding, pain |
Changes in Pelvic Floor Support | Altered bladder support | Incontinence, voiding difficulties |
In conclusion, bowel surgery can cause bladder problems in many ways. Understanding these mechanisms is key to managing and reducing urinary complications after surgery.
Risk Factors for Developing Bladder Dysfunction After Intestinal Surgery
Several factors can increase the risk of bladder problems after bowel surgery. Knowing these factors helps manage patient expectations and outcomes.
Pre-existing Urinary Conditions
Those with urinary issues before surgery face a higher risk of bladder problems afterward. Issues like incontinence, overactive bladder, or past urinary surgeries can make recovery harder.
Age and Gender-Specific Considerations
Age and gender are key in bladder dysfunction risk. Older people and women, who have had many pelvic surgeries, are more likely to have urinary issues after surgery.
Surgical Approach Comparison
The type of surgery affects bladder risk. Minimally invasive surgeries, like laparoscopic or robotic-assisted, might lower risk compared to open surgeries.
Extent and Location of Surgical Resection
The size and location of the surgery area matter a lot. Big surgeries, like those near the rectum or sigmoid colon, raise bladder risk. This is because these areas are close to the bladder.
Risk Factor | Description | Impact on Bladder Dysfunction |
Pre-existing Urinary Conditions | Previous urinary incontinence, overactive bladder | Increased risk |
Age and Gender | Older patients, women with multiple pelvic surgeries | Higher susceptibility |
Surgical Approach | Minimally invasive vs. open surgery | Reduced risk with minimally invasive |
Extent and Location of Resection | Extensive resections, rectal or sigmoid colon involvement | Increased risk due to proximity to bladder |
Understanding these risk factors helps doctors advise patients better. It also helps in reducing bladder dysfunction risks after intestinal surgery.
Colorectal Surgery and Specific Bladder Complications
Colorectal surgery, like procedures on the rectum, can affect the bladder. This is because the rectum and bladder are close and share nerves. This closeness can lead to bladder problems after surgery.
Rectal Surgery and Pelvic Autonomic Nerve Damage
Rectal surgery can harm the nerves that control the bladder. This can cause urinary retention and incontinence. The risk is higher when the surgery is near the nerves.
Using nerve-sparing techniques can help. But, it depends on the surgeon’s skill and the patient’s body.
Colon Resection Effects on Urinary Function
Colon resection can also impact the bladder, though less than rectal surgery. The impact varies based on the colon part and surgery type. Minimally invasive techniques might lower the risk of bladder problems.
Patients might face temporary issues like urinary tract infections or voiding difficulties. These usually get better in a few months.
Post-Operative Complications Affecting the Bladder
Complications after colorectal surgery can also harm the bladder. Adhesions and scar tissue formation can cause urinary retention. Infections or inflammation in the pelvic area can also affect bladder function.
Dealing with these issues often needs a team effort. This includes urological care and pelvic floor rehabilitation. Early action can lessen long-term bladder problems.
Diagnostic Approaches for Post-Bowel Surgery Bladder Issues
When bladder problems show up after bowel surgery, doctors use many ways to figure out what’s going on. They aim to understand and fix urinary issues.
Comprehensive Urodynamic Testing
Urodynamic tests are key to seeing how the bladder and urethra work. They check if urine is being stored and released right. These tests can spot problems like urinary retention and incontinence.
- Uroflowmetry measures the flow rate of urine.
- Cystometry checks how the bladder acts when it’s filling up with urine.
- Pressure flow studies look at the bladder’s pressure during urination.
Imaging Studies and Their Role
Imaging studies are very important for finding bladder problems after bowel surgery. Ultrasound and MRI help doctors see the bladder and nearby areas. They look for any damage or oddities.
Symptom Assessment and Questionnaires
Understanding symptoms is a big part of diagnosing bladder issues. Doctors use questionnaires and symptom scores to get a clear picture of what the patient is going through.
- Other tools might include bladder diaries and quality of life questionnaires.
By using all these methods, doctors can really get to know the bladder problems after bowel surgery. This helps them plan better treatments.
Treatment Options for Bladder Dysfunction After Bowel Resection
Urinary problems after bowel surgery are common. It’s important to know the treatment options. A leading urologist says, “The management of bladder dysfunction after bowel surgery requires a thorough approach. It considers the underlying causes and the patient’s health.”
Pharmacological Management Approaches
Medicines are often the first treatment for bladder issues after bowel surgery. Anticholinergics and beta-3 adrenergic agonists help with overactive bladder. Alpha-blockers are used for urinary retention.
The right medicine depends on the symptoms and medical history. For example, anticholinergics can help with urgency and frequency but might cause dry mouth.
Pelvic Floor Physical Therapy and Rehabilitation
Pelvic floor physical therapy is key in managing bladder issues. It strengthens the pelvic floor muscles. This improves bladder control and reduces incontinence symptoms.
A pelvic health physical therapist creates a custom exercise plan. This may include Kegel exercises, biofeedback, and electrical stimulation.
Surgical Interventions for Persistent Problems
If other treatments don’t work, surgery might be needed. Options include sacral neuromodulation, bladder augmentation, or urinary diversion. These are for severe bladder dysfunction.
These surgeries are for those whose bladder symptoms greatly affect their quality of life.
Intermittent and Indwelling Catheterization Techniques
Some patients need catheterization for urinary retention or incontinence. Intermittent catheterization drains the bladder at set times. Indwelling catheters stay in continuously.
Choosing between them depends on the patient’s needs and ability to safely use the catheter.
A medical expert notes, “The key to managing bladder dysfunction after bowel surgery is a personalized approach. It must address the individual’s unique needs and circumstances.”
Prevention Strategies to Minimize Bladder Complications
It’s key to prevent bladder problems in patients having bowel surgery. Knowing the risks helps doctors lower the chance of bladder issues after surgery.
Pre-Operative Assessment and Planning
Checking patients before surgery is very important. Doctors look at urinary conditions and health to plan better. This helps surgeons lower risks.
Nerve-Sparing Surgical Techniques
Using nerve-sparing surgery helps keep the bladder working. Surgeons use advanced imaging and nerve monitoring to protect nerves. This method cuts down nerve damage risks.
Minimally Invasive Approaches
Minimally invasive surgery, like laparoscopic or robotic, is better. It causes less damage and helps patients recover faster. This way, there’s less pain and fewer complications, like bladder problems.
Post-Operative Care Protocols
Good care after surgery is key to avoiding bladder issues. This includes early movement, right pain control, and watching for urinary problems. Following these steps helps doctors catch and fix any issues fast.
With these prevention steps, bladder problems after bowel surgery can be greatly reduced. This leads to better health and a better life for patients.
Recovery Timeline: What to Expect for Bladder Function
Patients who have bowel surgery often notice changes in how their bladder works. How fast and fully the bladder recovers depends on several things. These include the type of surgery, the patient’s health, and any bladder problems they had before surgery.
Immediate Post-Operative Period (1-2 Weeks)
Right after surgery, bladder function can change a lot. Urinary retention is common because of swelling, pain, or anesthesia effects. Many need a catheter to help with urine during this time.
Short-Term Recovery (1-3 Months)
As healing starts, bladder function usually gets better. But, some might keep having urinary incontinence or trouble peeing. Doing pelvic floor exercises and other rehab can help during this time.
Long-Term Outcomes and Adaptation (Beyond 3 Months)
After three months, recovery might slow down, but it keeps going. The surgery type, nerve damage, and health can affect how well you recover. Some people might have to live with permanent changes in their bladder function.
Permanent Changes and Coping Strategies
For some, bowel surgery can mean lasting bladder issues. Finding good ways to cope, like timed voiding or pelvic floor exercises, can really help. Working closely with doctors is key to managing these changes.
Knowing what to expect and the factors that affect bladder function after surgery can help patients. Being informed and proactive can lead to better recovery and overall health.
When to Seek Medical Attention for Post-Surgical Bladder Problems
People who have had bowel surgery need to know when to get medical help for bladder issues. Bladder problems after surgery can show up in different ways. Knowing the signs is important for getting help quickly.
Critical Warning Signs and Symptoms
It’s important for patients to watch out for signs of bladder problems after bowel surgery. Some key warning signs include:
- Persistent Urinary Retention: Trouble emptying the bladder fully.
- Severe Pain: Pain in the lower belly or pelvis that doesn’t go away.
- Infection Signs: Fever, chills, or blood or pus in the urine.
- Incontinence: Losing bladder control and leaking.
Emergency Situations Requiring Immediate Care
Some situations need immediate medical help. These include:
Situation | Symptoms |
Acute Urinary Retention | Can’t urinate, severe pain |
Severe Infection | High fever, chills, feeling confused |
Bladder Injury | Severe pain, bleeding |
Knowing these emergency situations can save lives.
“Prompt medical intervention is key to managing post-surgical bladder complications well.”
Follow-up Care Guidelines and Scheduling
Follow-up care is vital after bowel surgery. Patients should:
- Keep up with follow-up appointments as their doctor suggests.
- Tell their doctor about any new or getting worse symptoms right away.
- Stick to the treatment plan for bladder problems.
By following these steps, patients can lower the risk of long-term bladder problems.
Patient Experiences: Living with Bladder Issues After Bowel Operations
Patients dealing with bladder issues after bowel operations face many challenges. These challenges can greatly affect their daily lives. They need a lot of support to manage these issues.
Daily Management Strategies
It’s important to manage bladder issues well to feel normal. Patients use different methods like pelvic floor exercises and dietary changes. They also use absorbent products to deal with incontinence.
Pelvic floor rehabilitation is key in managing bladder problems. Kegel exercises help strengthen the muscles that control the bladder. This can help reduce incontinence symptoms.
Quality of Life Considerations
Bladder issues can greatly affect a patient’s quality of life. Simple tasks become hard, and social activities are often avoided. This is due to fear of incontinence or the need to go to the bathroom often.
To improve their situation, patients should be proactive. They can keep a bladder diary, adjust their fluid intake, and stay active.
Support Groups and Resources
Living with bladder issues after bowel surgery can feel isolating. But, there are support groups and resources available. They offer emotional support, practical advice, and a sense of community.
Connecting with others who face similar challenges is beneficial. Online forums, local support groups, and healthcare providers can provide valuable guidance and reassurance.
“Finding a community that understands your experiences can be incredibly empowering,” notesa patient advocate. “It’s a reminder that you’re not alone in this journey.”
Latest Research on Preventing Urinary Complications in Bowel Surgery
Recent studies show how vital it is to prevent urinary problems after bowel surgery. New methods are being found to lessen these issues.
Advances in Nerve-Preserving Surgical Techniques
Nerve-preserving surgery is showing great promise. It helps avoid damaging nerves that control the bladder. This reduces the risk of urinary problems.
Nerve-sparing surgery uses advanced tools to protect important nerves during surgery.
Novel Medication Protocols
Researchers are looking into new medicines to manage urinary issues after surgery. These might help the bladder work better or prevent infections.
Innovative Rehabilitation Approaches
New rehab methods, like pelvic floor physical therapy, are being used. They help patients recover from surgery and lower the risk of urinary problems.
Predictive Models for Risk Assessment
There’s also research on predictive models for risk. These models aim to spot patients at higher risk of urinary issues. This way, doctors can take specific steps to help them.
Research Area | Description | Potential Benefits |
Nerve-Preserving Surgery | Advanced techniques to preserve nerves during surgery | Reduced risk of urinary complications |
Novel Medication Protocols | New medications to manage and prevent urinary issues | Improved bladder function, reduced UTIs |
Innovative Rehabilitation | Pelvic floor physical therapy and other rehabilitation methods | Faster recovery, reduced urinary complications |
Predictive Models | Models to identify patients at higher risk of urinary complications | Targeted interventions, improved outcomes |
By focusing on these research areas, doctors hope to greatly reduce urinary problems after bowel surgery. This will improve patient outcomes and quality of life.
Conclusion
The connection between bowel surgery and bladder function is complex. It’s important to understand this to avoid complications. Many factors, like the surgery itself and the patient’s health, play a role in bladder problems after surgery.
Knowing how bowel surgery can affect the bladder helps both patients and doctors. They can work together to reduce risks and solve problems quickly. This knowledge helps patients understand their recovery better.
Being aware of bowel surgery’s effects on the bladder can improve recovery. It can also enhance the quality of life for those who have had bowel surgery.
FAQ
Can bowel surgery cause long-term bladder problems?
Yes, bowel surgery can cause long-term bladder issues. These include urinary retention, incontinence, and overactive bladder syndrome. This is due to nerve damage, inflammation, or changes in the pelvic floor.
What types of bowel surgery are most likely to affect bladder function?
Certain surgeries can impact bladder function. These include colorectal resection, small intestine surgery, and operations for inflammatory bowel disease. Also, surgeries for cancer in the bowel area can affect the bladder.
How can I minimize the risk of bladder complications after bowel surgery?
To reduce bladder risks, start with a thorough pre-op plan. Use nerve-sparing techniques and minimally invasive methods. Also, follow strict post-op care to minimize complications.
What are the common signs and symptoms of bladder problems after bowel surgery?
Signs include urinary retention, incontinence, and frequent urination. You might also experience urgency and recurrent infections. Seek medical help if these symptoms persist or get worse.
How is bladder dysfunction after bowel surgery diagnosed?
Doctors use urodynamic testing and imaging to diagnose. They also assess symptoms and use questionnaires to understand bladder function and find causes.
What treatment options are available for managing bladder dysfunction after bowel surgery?
Treatments include medications and physical therapy. For persistent issues, surgery might be needed. Intermittent or indwelling catheterization can also be used.
Can bladder function recover after bowel surgery?
Yes, bladder function can recover. Recovery times vary. Some see improvement quickly, while others may take longer or face ongoing issues.
Are there any risk factors that increase the likelihood of bladder dysfunction after bowel surgery?
Yes, several factors increase bladder risks. These include pre-existing urinary conditions, age, gender, and the type of surgery. The extent and location of the surgery also play a role.
How can I manage bladder issues after bowel surgery?
Manage bladder issues with lifestyle changes and exercises. Stick to your medication plan. Support groups and resources can offer additional help and guidance.
What is the impact of bowel surgery on bladder function in the long term?
Bowel surgery can have a significant impact on bladder function. Some may face permanent changes, while others see improvement or complete resolution over time.
Are there any advances in preventing urinary complications in bowel surgery?
Yes, new techniques and medications are being developed. These aim to reduce urinary complications in bowel surgery. Research also focuses on improving rehabilitation and predictive models for risk assessment.
What are the specific complications of colorectal surgery on the bladder?
Colorectal surgery can lead to specific bladder issues. These include damage to pelvic nerves during rectal surgery. It can also affect urinary function due to colon resection. Post-operative complications can also impact the bladder.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC6494605/