Last Updated on October 31, 2025 by Bilal Hasdemir

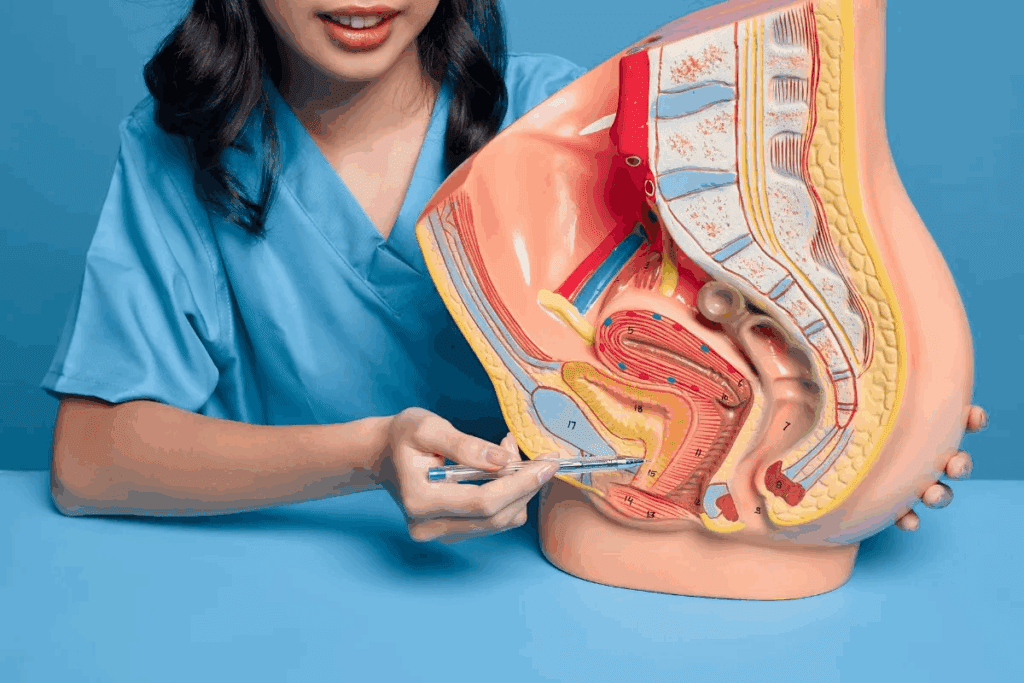
Benign prostatic hyperplasia (BPH) is a common issue for aging men. It’s about the nonmalignant growth of prostate tissue. Understanding BPH is key for good diagnosis and treatment. We look at how medical images help in diagnosing and managing BPH. This guide is for healthcare professionals and patients bph images.
Places like Liv Hospital focus on educating patients and using evidence-based care. High-quality medical photos are important for diagnosis and learning. They give great insights into urological health.
It’s important for aging men to know about Benign Prostatic Hyperplasia (BPH). BPH is when the prostate grows too much because of more cells.
As men get older, BPH becomes more common. By the 60s, up to 60% of men have BPH. By the 70s, it’s up to 90%.
BPH is a big problem for older men. It’s not the same as prostate cancer, even though both can make the prostate bigger.
More and more men get BPH as they age. It’s a big health issue for men in their later years.
| Age Group | Prevalence of BPH |
| 40-49 years | 20-30% |
| 50-59 years | 40-50% |
| 60-69 years | 50-60% |
| 70+ years | 80-90% |
The prostate gets bigger in BPH because of more cells. This makes it hard to pee because the urethra gets squished.
“The enlargement of the prostate gland is a hallmark of BPH, and understanding its pathophysiology is critical for developing effective treatment strategies.”
The reasons for BPH are complex. Hormones, cell growth, and maybe inflammation play a part.
Doctors need to understand BPH to treat it well. Knowing how BPH works helps them find better treatments.
BPH images are key in guiding diagnosis and treatment. They show the signs of enlarged prostate through different imaging methods.
Ultrasound and MRI are vital in diagnosing BPH. They help doctors see the prostate’s size and shape. This information is key in choosing the right treatment.
Transrectal ultrasound is used to measure prostate size and guide biopsies. This is important in deciding if surgery or other treatments are needed.
Understanding the link between BPH images and symptoms is key. Doctors use these images to see how prostate size affects urinary flow and symptoms.
This helps in creating treatment plans that meet each patient’s needs. For example, someone with a big prostate and bad symptoms might need stronger treatment than someone with mild symptoms.
Also, imaging can show the risk of problems like urinary retention or kidney damage. This allows for early action to prevent these issues.
Diagnosing BPH has changed a lot thanks to new imaging technologies. We now have many tools to help diagnose BPH, each with its own benefits and drawbacks.
Prostate imaging has evolved a lot. At first, doctors used digital rectal exams and asked about symptoms. But now, we have many imaging tools to help diagnose and treat BPH.
Early imaging techniques were based on X-rays, which didn’t give much info about the prostate. Then, ultrasound technology came along, letting doctors see the prostate better.
“The introduction of ultrasound in the diagnosis of BPH was a game-changer, allowing for non-invasive assessment of prostate size and morphology.”
Later, MRI and other advanced imaging techniques improved our ability to diagnose and treat BPH. These tools have made diagnosis more accurate and helped guide treatment.
BPH imaging can be divided into invasive and non-invasive methods. Non-invasive techniques like ultrasound and MRI are key for diagnosing BPH.
Invasive imaging methods, like biopsies, are used when cancer is suspected or detailed tissue analysis is needed.
Choosing the right imaging method for BPH is important. Invasive methods give detailed info but can be risky. Non-invasive methods are safer but might not work for everyone.
Knowing the good and bad of each imaging method helps us better diagnose and manage BPH. This leads to better care for patients.
Transrectal ultrasound (TRUS) is key in diagnosing benign prostatic hyperplasia (BPH). It gives us detailed images of the prostate gland. This makes it our go-to tool for BPH assessment.
When we use TRUS on patients with BPH, we see certain signs. These include:
These signs are vital for diagnosing BPH and figuring out how severe it is.
TRUS is great for measuring prostate volume and the transition zone. Here’s how we do it:
Getting the prostate volume right is key for diagnosing BPH and tracking its growth.
With TRUS, we can better diagnose and manage BPH. This improves patient care.
Magnetic Resonance Imaging (MRI) has changed how we diagnose Benign Prostatic Hyperplasia (BPH). It gives us detailed pictures of the prostate gland. This is key for managing and treating BPH effectively.
In MRI scans for BPH, T1 and T2 weighted images are both important. T1 weighted images help us see the prostate’s shape and find problems like lymphadenopathy or bone metastases. T2 weighted images show the prostate’s inside, helping us see how big it is and how it affects nearby areas.
Using both T1 and T2 images makes diagnosing BPH more accurate. It gives us a full view of the prostate. This helps us understand how severe BPH is and plan the best treatment.
Multiparametric MRI is a big step forward in diagnosing and treating BPH. It combines different MRI sequences like T1 and T2 images, diffusion-weighted imaging, and dynamic contrast-enhanced imaging. This gives us a detailed look at the prostate.
This detailed look lets us see the prostate’s size, shape, and how it works. We can then create treatment plans that fit each patient’s needs.
In summary, MRI has greatly improved diagnosing and treating BPH. It gives us detailed images of the prostate. This helps us provide better care to our patients.
Understanding how Benign Prostatic Hyperplasia (BPH) affects urine flow is key. We use advanced tests to see how BPH impacts urinary function. Uroflowmetry and pressure-flow studies are two main tools for this.
Uroflowmetry is a test that measures urine flow rate without surgery. It shows how urine flows, helping doctors spot BPH symptoms. The results are a flow curve, showing urine volume per second over time.
The flow curve’s shape tells doctors about urinary blockage. For example, a long voiding time and low flow rate suggest severe BPH.
| Parameter | Normal Value | BPH Indication |
| Maximum Flow Rate (Qmax) | >15 ml/s | |
| Voiding Time | >60 seconds |
Pressure-flow studies measure bladder pressure during voiding. This test gives detailed info on bladder contractility and prostate resistance.
By looking at pressure-flow graphs, doctors can tell if a patient has bladder outlet obstruction or detrusor underactivity. This is important for choosing the right treatment.
For instance, a patient with high bladder pressure and low flow rate likely has bladder outlet obstruction. But a patient with low bladder pressure and low flow rate might have detrusor underactivity.
We use these images to make treatment plans that fit each patient’s needs. This ensures the best care for their BPH.
X-ray imaging is key in diagnosing and managing Benign Prostatic Hyperplasia (BPH). We use X-ray imaging to check the urinary tract and prostate gland, mainly in tough cases.
Intravenous pyelogram (IVP) is an X-ray imaging method that shows the upper urinary tract well. For BPH, IVP spots urinary tract changes from enlarged prostate.
Key findings on IVP for BPH include:
CT urography is an X-ray imaging method that gives detailed views of the urinary tract. It’s great for complex BPH cases with upper tract damage or other issues.
The advantages of CT urography include:
| Imaging Modality | Key Features | Clinical Utility |
| Intravenous Pyelogram (IVP) | X-ray based, contrast-enhanced imaging of the urinary tract | Assesses upper urinary tract changes due to BPH |
| CT Urography | High-resolution, cross-sectional imaging of the urinary tract | Provides a detailed look at complex BPH cases |
Using these X-ray imaging methods, we better understand BPH and its impact on the urinary tract. This helps us find better treatment plans.
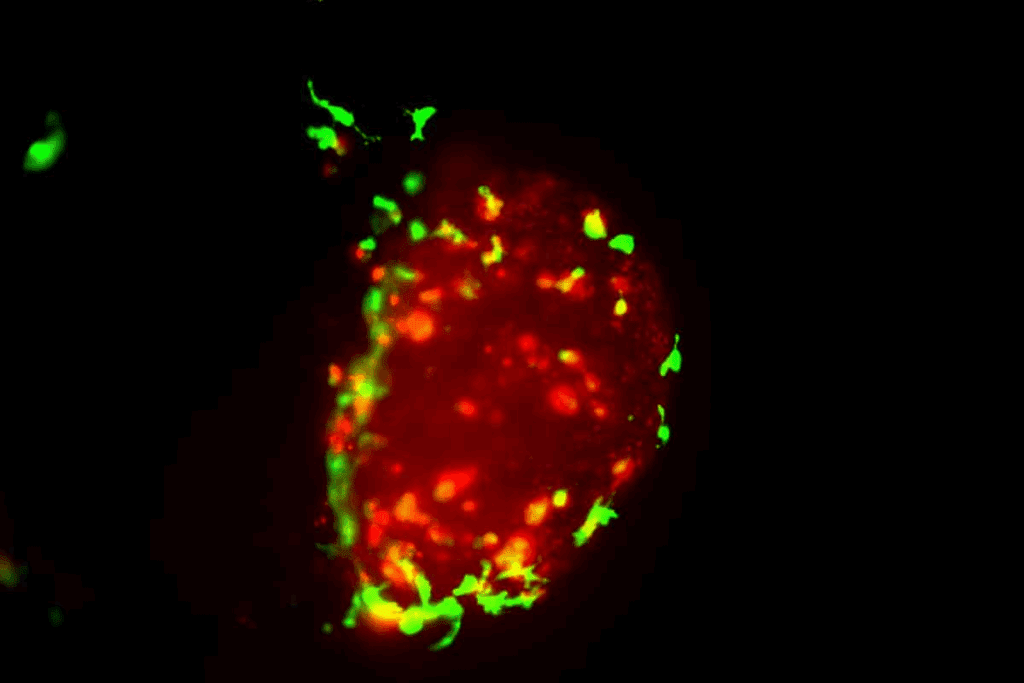
Histopathology gives us a close look at the prostate’s cells. It helps us understand Benign Prostatic Hyperplasia (BPH) better. By looking at cells under a microscope, we can spot changes in BPH. This is key for making the right diagnosis and treatment plan.
In BPH studies, we see two main types of growth: stromal and glandular. Stromal hyperplasia means more growth in the tissue around the cells. Glandular hyperplasia is when the gland parts get bigger. Knowing these differences helps us understand BPH better in each patient.
Knowing the type of growth matters for treatment. For example, how much stromal tissue there is can affect treatment choices. This makes treatment plans more personal.
Immunohistochemical staining is a big help in BPH studies. It lets us see specific proteins in the tissue. This gives us clues about what’s happening in BPH.
Using immunohistochemical staining has really helped us understand BPH. It shows us how the disease works at a cellular level. This helps us create better treatments.
By combining what we see in the lab with what we know from patients, we can do better for BPH patients. We can make treatments that really fit each person’s needs.
Cystoscopy is a key procedure that lets doctors see the prostate and bladder outlet directly. This is important for diagnosing and treating Benign Prostatic Hyperplasia (BPH).
Through cystoscopy, doctors get detailed images of the prostate and bladder. These images show how big the prostate is and how it affects the urethra. This information is key for figuring out how severe BPH is and what treatment is best.
During cystoscopy, doctors can see how big the prostate is and how it blocks the urethra. This helps them understand how much the prostate is blocking the flow.
The doctor uses a cystoscope to look inside the bladder. This lets them see the bladder outlet and prostate up close. The images taken during this are very helpful for making a diagnosis.
Cystoscopy is also great for finding out if there’s a blockage at the bladder outlet. Doctors can see the bladder neck and prostate urethra. This helps them know if there’s a blockage and how bad it is.
The info from cystoscopy helps doctors decide the best treatment for BPH. Whether it’s medicine, surgery, or something else, the findings from endoscopy are very important.
In short, cystoscopy and prostate visualization are very important for treating BPH. They let doctors see the prostate and bladder outlet clearly. This helps them make accurate diagnoses and effective treatment plans.
Using different BPH images is key for better patient care. We’ve learned how various imaging methods give us important insights into BPH. By mixing data from ultrasound, MRI, and other tools, doctors can make accurate diagnoses and plans.
When we combine findings from different images, we get a clearer picture of BPH. This helps us understand how big the prostate is and how it affects urination. It also helps us choose the best treatment for each patient. This leads to better health and care for our patients.
We think using BPH images in care will keep getting better. New imaging tech and more knowledge about BPH will help. By keeping up with these changes, we can give our patients the best care. This means better health for everyone.
BPH is when the prostate gland gets bigger. It happens to more than half of men over 60. This condition can make it hard to pee and lower your quality of life.
Doctors use many ways to see BPH, like ultrasound and MRI. They also use TRUS and X-rays like CT urography. Each method gives different info to help figure out what to do next.
TRUS is the top choice for looking at BPH. It measures the prostate and checks for signs of enlargement. This helps doctors decide on treatment.
MRI gives a full view of the prostate. It uses special images to help doctors understand how big it is. This makes planning treatment easier.
Histopathology looks at tiny details of BPH. It tells doctors about the types of growths in the prostate. This info helps in making treatment plans.
Tools like uroflowmetry show how urine flows. They help doctors understand the problem better. This is key for choosing the right treatment.
Using all kinds of images helps doctors give better care. It leads to accurate diagnoses and effective treatments. This improves how well patients do and their overall quality of life.
Endoscopy lets doctors see the prostate directly. They can see how big it is and if it’s blocking the bladder. This is important for knowing how bad BPH is and what to do about it.
National Center for Biotechnology Information.7 BPH Images Essential Medical Photo Guide Benign. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK558920/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us