Last Updated on November 27, 2025 by Bilal Hasdemir
Chemotherapy plays a vital role in fighting brain tumors, aiming to destroy cancer cells while protecting surrounding healthy tissue. At Liv Hospital, we provide advanced brain tumor chemotherapy treatment designed to improve patient outcomes and quality of life.
Our expert medical team focuses on precise diagnosis and personalized therapy, tailoring each treatment plan based on the patient’s type and stage of cancer. We use leading chemotherapy drugs and innovative delivery methods to ensure optimal effectiveness with minimal side effects. Liv Hospital is dedicated to delivering world-class healthcare, offering continuous care, guidance, and support to both local and international patients throughout their treatment journey.
Key Takeaways
- Chemotherapy plays a critical role in brain tumor management.
- Liv Hospital offers comprehensive care with international standards.
- Personalized treatment plans are tailored to each patient’s needs.
- Effective drugs and innovative delivery methods are used.
- Optimal outcomes are achieved through expert care and guidance.
The Critical Role of Chemotherapy in Brain Tumor Management
Chemotherapy is key in fighting brain tumors. It targets cancer cells and stops them from growing. We use it to kill cancer cells while keeping the healthy brain safe.
How Chemotherapy Targets Cancer Cells in the Brain
Chemotherapy for brain cancer uses drugs that attack fast-growing cancer cells. These drugs can be taken by mouth or given through an IV. Our team picks the best treatment based on the tumor and the patient’s health.
The goal is to shrink tumors and make life better for patients. By attacking cancer cells, chemotherapy slows or stops tumor growth. This gives patients a better chance of recovery.
Balancing Efficacy and Brain Tissue Preservation
One big challenge in brain cancer treatment is finding the right balance. We aim to kill cancer cells without harming the brain. We choose the right drugs and doses carefully to achieve this.
To show how different drugs work, let’s look at some examples:
| Chemotherapy Agent | Tumor Type | Efficacy | Common Side Effects |
| Temozolomide | Glioblastoma | High | Nausea, Fatigue |
| Carmustine (BCNU) | Various Brain Tumors | Moderate | Pulmonary Toxicity, Myelosuppression |
| Lomustine (CCNU) | Brain Tumors, Lymphoma | Moderate | Myelosuppression, Nausea |
As the table shows, different drugs work differently and have different side effects. This helps us create treatment plans that fit each patient’s needs.
Navigating the Blood-Brain Barrier Challenge

The blood-brain barrier is a big challenge in treating brain tumors with chemotherapy. It protects the brain but also stops chemotherapy drugs from reaching tumors.
Understanding the Protective Barrier Mechanism
The blood-brain barrier is made of cells that line blood vessels in the brain. It acts as a filter, letting some molecules in but keeping others out. This barrier is vital for the brain’s health but makes it hard to get drugs to tumors.
We look at how well chemotherapy drugs can get past the blood-brain barrier. We check their size, how well they dissolve in fats, and how they move through the barrier.
Drug Selection Criteria for Effective Penetration
We pick chemotherapy drugs based on how well they can get through the blood-brain barrier. We look at:
- Molecular size and structure
- Lipid solubility
- Ability to utilize specific transport mechanisms
- Drug interactions with other medications
By checking these things, we choose drugs that can best get to brain tumor cells.
| Chemotherapy Drug | Ability to Cross Blood-Brain Barrier | Common Use in Brain Tumor Treatment |
| Temozolomide | High | Glioblastoma |
| Carmustine (BCNU) | Moderate | Various brain tumors |
| Lomustine (CCNU) | Moderate | Brain tumors, including glioblastoma |
Knowing how the blood-brain barrier affects chemotherapy helps us find better treatments. By picking drugs that can get past this barrier, we can help more patients with brain tumors.
Temozolomide: The Gold Standard for Glioblastoma Treatment
Temozolomide is seen as the top choice for glioblastoma treatment. It can get past the blood-brain barrier. This makes it great at hitting glioblastoma cells.
Mechanism of Action and Effectiveness
Temozolomide works by messing with DNA in cancer cells. This stops them from growing. It’s easy to take because it’s an oral drug. Research shows it helps patients live longer, even with radiation therapy.
It’s good at getting into the brain because it can cross the blood-brain barrier. This is a big deal in brain tumor treatment. It helps it hit cancer cells better.
Administration Protocols and Patient Response Patterns
Patients take temozolomide by mouth, once a day, on an empty stomach. The dose and how long you take it depend on your health and how you react. Treatment usually lasts 6-12 cycles, each 28 days long.
How well patients do with temozolomide varies. Some see big improvements, like living longer and feeling better. Others may not see as much change. It’s important to watch how patients do and adjust treatment as needed.
Temozolomide is a big step forward in treating glioblastoma. It gives hope to patients and doctors. Its use in treatment plans is a key area for ongoing research and practice.
Nitrosoureas in Brain Tumor Therapy
Chemotherapy for brain tumors often uses nitrosoureas. They can get past the blood-brain barrier. This makes them key in treating brain tumors. They are effective because they can reach the brain, targeting the tumor more precisely.
Carmustine (BCNU): Applications and Delivery Methods
Carmustine, or BCNU, is used for many brain tumors, like glioblastoma. It can be given through an IV or as a wafer in the tumor during surgery. This gives doctors options to fit each patient’s treatment plan.
Lomustine (CCNU): Treatment Regimens and Outcomes
Lomustine, or CCNU, is another nitrosourea for brain tumors. It’s taken by mouth and crosses the blood-brain barrier well. Its oral form makes it easy for long-term treatment.
Carmustine and lomustine both work well against brain tumors. The choice depends on the tumor type, patient health, and past treatments.
| Drug | Administration Method | Common Use |
| Carmustine (BCNU) | Intravenous/Wafer Implant | Glioblastoma, other brain tumors |
| Lomustine (CCNU) | Oral | Brain tumors, including glioblastoma |
The PCV Combination Regimen Explained
The PCV combination regimen is a key treatment for brain tumors. It combines procarbazine, lomustine, and vincristine. This mix is a standard treatment that works well against brain tumors.
Procarbazine: Mechanism and Role in the Combination
Procarbazine is a vital part of the PCV regimen. It damages the DNA of cancer cells, stopping them from growing. As an alkylating agent, it breaks DNA strands, causing cell death.
Adding procarbazine to the PCV regimen boosts its effectiveness. It can get past the blood-brain barrier, making it great for treating brain tumors.
Vincristine: Contribution to the PCV Protocol
Vincristine is another key drug in the PCV mix. It stops cancer cells from dividing by blocking microtubule formation. This action halts cancer cell growth.
Vincristine works alongside procarbazine and lomustine to fight tumors. Its addition enhances the treatment’s effectiveness by targeting cancer cells in different ways.
Clinical Applications and Success Rates of PCV Therapy
The PCV regimen is used for many brain tumors, like oligodendrogliomas and anaplastic astrocytomas. Studies show it improves survival rates for these patients.
| Tumor Type | Progression-Free Survival | Overall Survival |
| Oligodendroglioma | 60-80% | 70-90% |
| Anaplastic Astrocytoma | 40-60% | 50-70% |
PCV therapy success rates depend on the tumor type and patient factors. Yet, it’s a mainstay in treating brain tumors, giving patients a valuable treatment option.
Platinum-Based Agents for Brain Cancer
Platinum-based agents like cisplatin and carboplatin are key in fighting brain cancer. They are effective in targeting cancer cells. This makes them a big part of many treatment plans.
Cisplatin: Applications in Brain Tumor Treatment
Cisplatin is a chemotherapy drug used for many cancers, including brain tumors. It works by damaging DNA, which kills cancer cells. This is why it’s good at fighting fast-growing cancer cells.
Key Applications:
- Used with other drugs to work better.
- Helps treat certain brain tumors, like glioblastoma.
- Given through an IV to reach all parts of the body.
Carboplatin: Advantages and Treatment Protocols
Carboplatin is another important drug for brain cancer. It’s similar to cisplatin but has fewer side effects. This makes it a good choice for some patients.
Advantages:
- Has fewer side effects than cisplatin.
- Good for patients who can’t take cisplatin.
- Often used with other drugs for brain tumors.
Here’s how cisplatin and carboplatin compare in treating brain cancer:
| Characteristics | Cisplatin | Carboplatin |
| Mechanism of Action | Cross-links DNA, interfering with DNA repair | Similar to cisplatin, cross-links DNA |
| Administration Route | Intravenous | Intravenous |
| Common Side Effects | Nausea, nephrotoxicity, neurotoxicity | Myelosuppression, nausea |
| Use in Brain Cancer | Effective in certain brain tumors, including glioblastoma | Used in combination regimens for brain tumors |
In conclusion, drugs like cisplatin and carboplatin are key in treating brain cancer. They target fast-growing cells well. Knowing how to use these drugs helps doctors give better care to patients.
Brain Tumor Chemotherapy Treatment: Delivery Methods and Approaches
Choosing the right way to give chemotherapy for brain tumors is key. The method used can greatly affect how well the treatment works and the patient’s life quality.
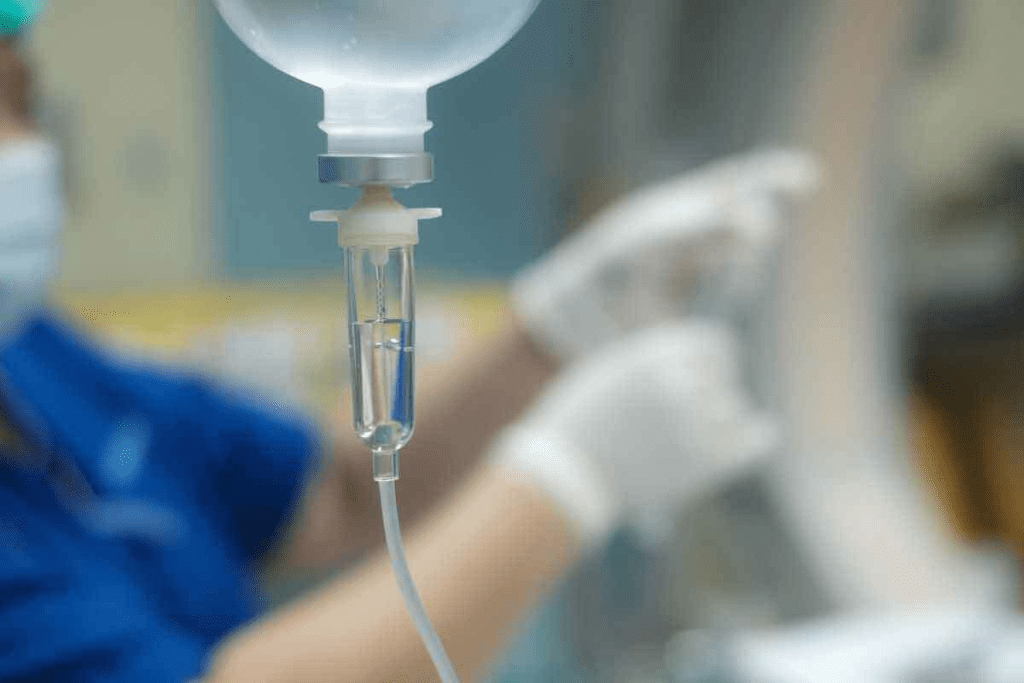
Oral Administration: Convenience and Compliance Factors
Oral chemotherapy is given at home, making it easier for patients. Temozolomide is a drug used for brain tumors. It can get past the blood-brain barrier.
It’s easier on patients because they don’t have to go to the hospital as much. But, they must take it exactly as told to work well.
Intravenous Delivery: Protocols and Monitoring
Intravenous chemotherapy is another way to give drugs. It lets doctors use drugs like cisplatin and carboplatin for brain tumors.
But, it needs close watch because of side effects and exact dosing. Patients often go to the hospital for it and check-ups.
Intrathecal Chemotherapy: Direct CNS Delivery
Intrathecal chemotherapy puts drugs right into the spinal fluid. It’s good for tumors in the CNS or spreading there.
It’s very effective but needs special care. Risks include infection or nerve problems.
Gliadel Wafers: Surgical Implantation Techniques
Gliadel wafers are put in the tumor during surgery. They’re filled with carmustine. This method gets chemotherapy right to the tumor.
Studies show it can help some patients with malignant glioma live longer. The surgery must be precise for it to work best.
Treatment Duration and Cycles: What Patients Can Expect
Patients with brain cancer often ask about their treatment length and what to expect. The time for chemotherapy varies based on the tumor type, stage, and individual factors. We will explore standard treatment plans and what affects their length and intensity.
Standard Treatment Protocols
Chemotherapy for brain tumors usually involves several cycles. The number of cycles can range from 6 to 12, depending on the tumor and patient response. For example, research shows that certain protocols work better for specific tumors.
| Tumor Type | Typical Number of Cycles | Treatment Goals |
| Glioblastoma | 6-8 cycles | Control tumor growth, manage symptoms |
| Meningioma | 6-12 cycles | Achieve tumor shrinkage, improve quality of life |
Factors Affecting Treatment Duration
Several factors can change how long and intense chemotherapy is. These include the patient’s health, how the tumor responds, and any side effects. Adjustments to treatment protocols are made to improve outcomes.
“The ability to adjust treatment based on patient response is key in managing brain tumors effectively.” – a Neuro-Oncologist
Knowing what affects treatment duration and understanding standard protocols helps patients prepare. It’s vital for patients to talk about their treatment plan and any worries with their healthcare provider.
Managing Side Effects and Quality of Life During Treatment
Chemotherapy for brain tumors needs a full plan to handle side effects and keep quality of life good. As we deal with brain tumor treatment, we must face the challenges patients have during chemotherapy.
Common Adverse Effects and Mitigation Strategies
Chemotherapy for brain tumors can cause many side effects, from mild to severe. Common ones include:
- Fatigue: A constant feeling of tiredness that can affect daily life.
- Nausea and Vomiting: Managed with antiemetic meds and diet changes.
- Hair Loss: A temporary issue that goes away after treatment ends.
- Cognitive Changes: Some patients might have memory problems or trouble focusing.
To lessen these side effects, we use both medical help and lifestyle changes. For example, fatigue management can include pacing activities, eating well, and getting enough sleep.
Supportive Care and Lifestyle Adjustments
Supportive care is key to improving life quality for patients on chemotherapy. This includes:
- Nutritional Support: A diet that meets the patient’s nutritional needs.
- Psychological Support: Counseling and support groups for emotional challenges.
- Physical Activity: Gentle exercises that fit the patient’s abilities.
By adding these supportive care steps and making lifestyle changes, patients can handle chemotherapy side effects better. This helps them keep a good quality of life during treatment.
Innovative Approaches and Future Directions
The field of brain tumor treatment is changing fast. New methods are being developed to help patients. Researchers are working hard to find better ways to treat brain tumors.
Targeted Therapies and Personalized Medicine
Targeted therapies are a big step forward. They focus on the unique traits of tumors. This helps protect healthy brain cells.
Personalized medicine goes even further. It tailors treatments to each patient’s tumor genetics. This makes treatments more effective and safe.
Now, treatments are getting better and causing fewer side effects. For example, drugs targeting glioblastoma’s genetic mutations are being made. This precision medicine aims for better results with fewer side effects.
Advanced Local Delivery Systems in Development
Local delivery systems are another big innovation. Scientists are creating ways to send chemotherapy straight to tumors. This avoids the blood-brain barrier.
Methods like convection-enhanced delivery are being tested. They aim to increase drug effectiveness at the tumor site. This could reduce side effects for the rest of the brain.
These new systems are showing great promise in trials. They could make chemotherapy more effective and safer. We’re excited about these advancements for better patient care.
Conclusion: Optimizing Brain Tumor Chemotherapy Outcomes
Improving brain tumor chemotherapy results needs a detailed and personal plan. At Liv Hospital, we focus on top-notch care and support for international patients. We aim to meet each patient’s unique needs.
Our team creates special treatment plans for each patient. We use the latest in chemotherapy, like temozolomide and platinum-based agents. Our goal is to boost patient results and life quality.
We keep innovating in medical care. Our aim is to give our patients the best care and support. We want to help patients live their best lives, free from brain tumors.
FAQ
What is the role of chemotherapy in brain tumor management?
Chemotherapy is key in fighting brain tumors. It targets cancer cells and stops them from growing. Our team makes sure it works well without harming healthy brain cells.
How do chemotherapy drugs cross the blood-brain barrier?
Our team picks drugs that can get past the blood-brain barrier. This ensures patients get the best treatment. For example, temozolomide can cross this barrier.
What is temozolomide used for in glioblastoma treatment?
Temozolomide is the top choice for glioblastoma treatment. It can get into the brain and kill cancer cells effectively.
What are nitrosoureas used for in brain tumor therapy?
Nitrosoureas, like carmustine and lomustine, are vital in treating brain tumors. They are used in many treatment plans and ways.
What is the PCV combination regimen used for in brain tumor treatment?
The PCV regimen is a common treatment for brain tumors. It combines procarbazine, lomustine, and vincristine for better results.
How are platinum-based agents used in brain cancer treatment?
Platinum-based agents, such as cisplatin and carboplatin, are important in brain cancer treatment. They are used in many treatment plans and have benefits.
What are the different methods of delivering chemotherapy for brain tumors?
Chemotherapy for brain tumors can be given in several ways. These include taking pills, getting shots, using intrathecal chemotherapy, or Gliadel wafers. Each method has its own benefits and ease of use.
How long does chemotherapy treatment for brain tumors typically last?
The length and number of chemotherapy cycles vary. It depends on the tumor type, stage, and the patient’s health. Treatments usually last from 6 to 12 cycles.
How are side effects managed during brain tumor chemotherapy treatment?
Managing side effects and keeping quality of life high is key. Common side effects are reduced with supportive care and lifestyle changes.
What are the future directions in brain tumor chemotherapy treatment?
Brain tumor treatment is getting better fast. New approaches and directions offer hope. These include targeted therapies, personalized medicine, and advanced delivery systems.
What is glioma chemotherapy?
Glioma chemotherapy uses drugs to treat gliomas, a type of brain tumor. The goal is to stop tumor growth and improve patient outcomes.
What are the common chemotherapy drugs used for brain tumors?
Common drugs for brain tumors include temozolomide, nitrosoureas, PCV regimen, and platinum-based agents. Each drug works differently and has its own treatment plan.
References:
- Jezierzaş„ski, M. (2024). Temozolomide (TMZ) in the Treatment of Glioblastoma: Efficacy and Clinical Trials. PMC, https://pmc.ncbi.nlm.nih.gov/articles/PMC11275351/