Last Updated on November 3, 2025 by mcelik

Getting a brain cancer diagnosis can feel overwhelming. Finding the right chemotherapy is key. At Liv Hospital, we offer top-notch care and support to patients from around the world.
We want to help you understand your treatment options. We aim to explain how chemotherapy helps with brain tumors. This includes how drugs are delivered and the main medicines used.
Brain tumors are a wide range of growths, each with its own set of challenges. Their complexity comes from different types, grades, and locations in the brain. Knowing these details is key to finding the right treatment.
Brain tumors are divided into primary and metastatic types. Primary tumors start in the brain, while metastatic ones spread from other parts of the body.
Primary brain tumors are split into types based on where they start. The most common include:
Each type of tumor has its own traits that affect how it’s treated.
Brain cancer treatment is tough for several reasons. The blood-brain barrier makes it hard to get drugs to the tumor. Also, the brain’s delicate areas make surgery risky.
Chemotherapy for brain tumors uses different ways to get drugs to the tumor. These include:
The right treatment depends on the tumor’s type, grade, and the patient’s situation.
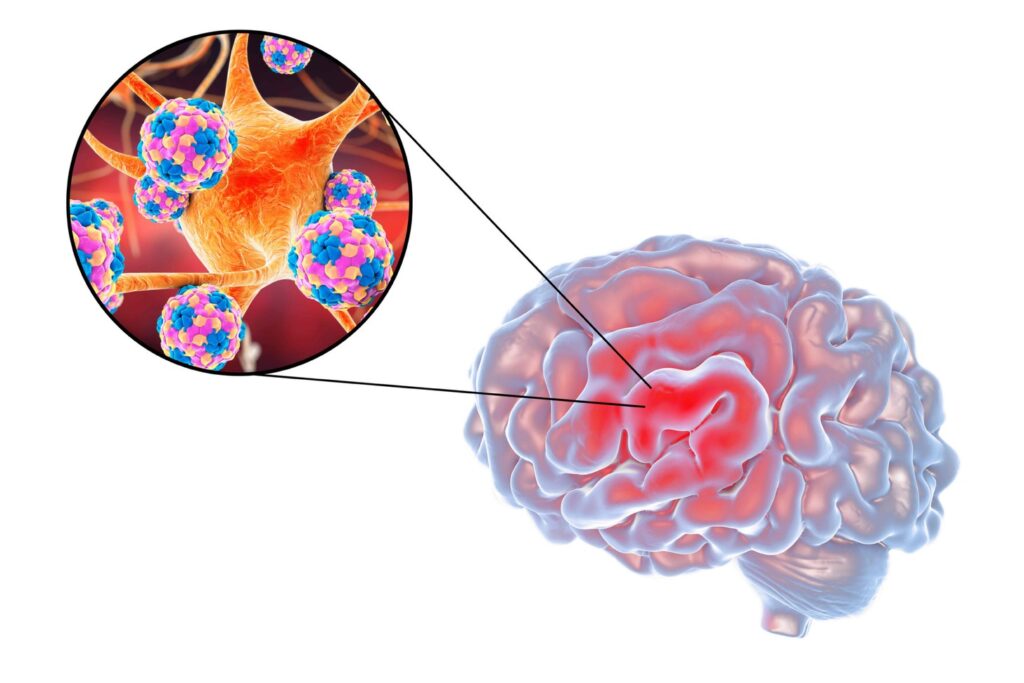
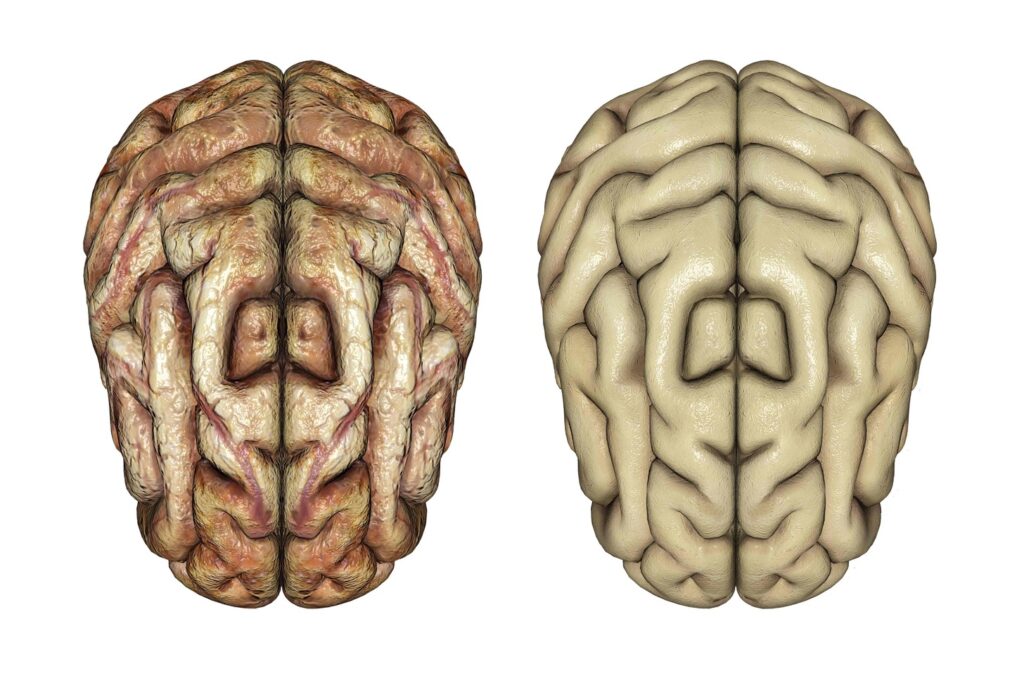
The blood-brain barrier is a big problem in treating brain tumors. It keeps the brain safe from harmful stuff. But, it also makes it hard to get chemotherapy drugs to the tumor.
The blood-brain barrier is a special layer that keeps the brain safe. It’s made of cells that block most substances from getting in. This barrier is tight and protects the brain.
This barrier keeps most molecules out, including many drugs. It helps keep the brain safe from toxins. But, it makes it hard to get drugs to brain tumors.
“The blood-brain barrier remains one of the most significant challenges in treating brain tumors, as it limits the effectiveness of many therapeutic agents.”
To get drugs past the blood-brain barrier, scientists and doctors have found ways:
| Strategy | Description | Advantages |
|---|---|---|
| Drug Modification | Changing drugs to help them get through the barrier. | Easy and can use drugs we already have. |
| Focused Ultrasound | Using sound waves to open the barrier. | Can target specific areas, not too invasive. |
| Nanoparticles | Creating tiny particles to carry drugs across the barrier. | Very specific, can be made for different drugs. |
| Direct Injection | Putting drugs directly into the brain or tumor. | Gets around the barrier, high drug concentration. |
By understanding the blood-brain barrier and using these strategies, we can make brain tumor treatment better. New technologies and methods help us get drugs to tumors more effectively. This gives us hope for better treatment results.
Brain tumor chemotherapy treatment uses different methods. Each has its own benefits and challenges. We’ll look at these approaches, including systemic, localized, and new technologies. This will help us understand the treatment options better.
Systemic administration means giving chemotherapy drugs all over the body. This is done through the bloodstream. It can be through IV infusion or oral pills.
Intravenous Administration: IV chemotherapy is a common way to treat brain tumors. Drugs are given directly into a vein. This method allows for quick and high drug levels.
Oral Administration: Some drugs come in pill form. This is convenient and can be as effective as IV for some drugs.
Localized delivery aims to target the tumor directly. This reduces side effects all over the body.
Wafers: Chemotherapy wafers are small, dissolvable disks. They are placed in the tumor during surgery. They slowly release drugs, treating the area.
Lumbar Puncture: This method involves injecting drugs into the spinal fluid. It allows the drugs to reach the brain and spinal cord.
| Delivery Method | Advantages | Disadvantages |
|---|---|---|
| Intravenous | High drug concentrations, quick administration | Systemic side effects, possible toxicity |
| Oral | Convenient, can be as effective as IV | Limited to drugs available in oral form |
| Wafers | Localized treatment, minimizes systemic effects | Limited to surgically accessible tumors |
| Lumbar Puncture | Targets central nervous system, reduces systemic toxicity | Requires specialized procedure, possible side effects |
New delivery technologies are being researched. They aim to improve brain tumor chemotherapy.
These new technologies aim to better deliver drugs and reduce side effects. As research grows, we’ll see more effective treatments for brain tumors.
Temozolomide is a key part of treating glioblastoma, a tough brain cancer. We’ll look at its role in fighting this disease.
Temozolomide damages cancer cells’ DNA. This stops them from growing. It’s a big help in slowing glioblastoma tumors.
Key benefits of temozolomide include:
The dose of temozolomide depends on the patient’s size. It’s adjusted based on how they do. It’s easy to take because it’s a pill.
Standard dosing protocols involve:
Many things can affect how well a patient does with temozolomide. These include their health, the type of glioblastoma, and how they handle the treatment.
Factors affecting patient response:
| Factor | Description | Impact on Treatment |
|---|---|---|
| MGMT gene methylation status | The methylation status of the MGMT gene promoter | Patients with methylated MGMT gene promoters tend to respond better to temozolomide |
| Patient’s age and health | Older patients or those with poor health may have a different response | May require dose adjustments or additional supportive care |
| Tumor characteristics | Size, location, and aggressiveness of the glioblastoma | Can influence the effectiveness of temozolomide in shrinking the tumor |
Knowing these factors helps us make treatment plans that work best for each patient. This way, we can get the most out of temozolomide in fighting glioblastoma.
Nitrosoureas, like carmustine and lomustine, are key in brain cancer treatment. They’ve been around for decades, helping many patients with brain tumors.
Carmustine is a nitrosourea used for brain tumors, like glioblastoma. It stops cancer cells from growing by messing with their DNA.
It’s great because it can get past the blood-brain barrier. This makes it effective against brain tumors. It can be given in different ways, such as:
The method used depends on the patient’s situation.
Lomustine is another nitrosourea used in brain cancer treatment. It’s often mixed with other drugs. It’s good for treating glioblastoma and anaplastic astrocytoma.
Lomustine is taken by mouth, which is easy for patients. It can get into the brain, which helps in fighting brain cancer.
Carmustine and lomustine both work well against brain tumors. But, their use depends on the type of tumor and the patient. Carmustine can be placed directly on the tumor with wafers. Lomustine is taken orally, affecting the whole body.
Choosing between carmustine and lomustine depends on the treatment plan and the patient’s health. Studies are ongoing to see which is better, helping doctors make the right choice.
Procarbazine and vincristine are key drugs in the PCV therapy for brain cancer. The PCV regimen, with lomustine, is a mainstay for treating certain brain tumors. It’s mainly used for patients with specific gliomas.
Procarbazine is an alkylating agent that damages cancer cells’ DNA. This stops them from reproducing. It’s given orally, making it easy for long-term treatment.
Procarbazine is effective in treating brain tumors, even more so with other drugs. It can cross the blood-brain barrier, targeting brain cancers well.
Vincristine is a vinca alkaloid that stops cell division. It binds to tubulin, a protein in cells. Vincristine is given intravenously, with doses based on the patient’s condition.
In brain tumor management, vincristine targets fast-growing cancer cells. It works better with other drugs, making treatment more effective.
The PCV regimen includes procarbazine, lomustine, and vincristine. It’s a standard treatment for certain brain tumors. This combination uses each drug’s unique action, attacking cancer cells from different angles.
Studies show the PCV regimen improves outcomes for these tumors. The synergy between the drugs makes it effective.
Understanding procarbazine and vincristine’s roles in PCV helps tailor treatments. This personalized approach is key to better outcomes for brain tumor patients.
Platinum-based therapies, like cisplatin and carboplatin, are key in fighting brain tumors. They are also used in treating other cancers. These drugs are important in the fight against brain tumors.
Cisplatin and carboplatin create platinum-DNA adducts. These adducts mess with DNA repair, causing cancer cells to die. This is why they work well against fast-growing cancer cells.
These drugs can get past the blood-brain barrier to some extent. But, how well they work depends on the tumor type and location.
Cisplatin is often used with other drugs for brain tumors like medulloblastoma and germ cell tumors. Carboplatin is used for those who can’t handle cisplatin because of its side effects.
These drugs can really help, with some patients seeing big reductions in tumors. But, results can vary a lot from person to person.
| Drug | Common Indications | Notable Side Effects |
|---|---|---|
| Cisplatin | Medulloblastoma, Germ Cell Tumors | Nephrotoxicity, Ototoxicity |
| Carboplatin | Medulloblastoma, Gliomas | Myelosuppression, Thrombocytopenia |
It’s important to manage the side effects of cisplatin and carboplatin to keep patients’ quality of life good. For cisplatin, we use hydration and diuresis to prevent kidney damage. For carboplatin, we watch blood counts to avoid low blood cells.
We also adjust doses and schedules to reduce side effects while keeping the treatment effective. For more on chemotherapy cycles, check out our page on chemotherapy rounds.
By carefully managing these therapies, we can make them more beneficial and safer for patients.
Brain tumor chemotherapy treatment cycles can vary a lot. It’s important for patients to know how long treatment will last. This helps them get ready for what’s coming.
Brain tumor chemotherapy is given in cycles. Each cycle has a recovery time after it. The usual plan includes:
The whole treatment duration can be from 6 months to a year or more. This depends on how well the patient responds and the treatment plan.
Many things can change how long treatment cycles and treatment duration are. These include:
Patients get checked often to see how they’re doing with brain tumor chemotherapy. These checks might include:
Based on these checks, the treatment plan might change. This could mean switching chemotherapy drugs, changing when treatment is given, or adding other treatments.
Knowing what affects treatment cycles and duration helps patients prepare. It lets them make smart choices about their care.
It’s key to manage brain tumor chemotherapy side effects to keep patients’ quality of life high. We know that while chemotherapy is vital, it can also have big effects on daily life.
Chemotherapy for brain tumors can cause many side effects. These can be mild or severe. Some common ones include:
These effects can differ based on the drugs, dosage, and how each patient reacts. It’s important for patients to talk about their side effects with their healthcare team. This way, they can get the right help and support.
Supportive care is key in managing chemotherapy side effects and improving quality of life. We suggest several strategies, including:
For more on managing chemotherapy side effects, visit our resource page.
To keep quality of life high during brain tumor chemotherapy, a mix of medical treatment, lifestyle changes, and emotional support is needed. We suggest:
By using these strategies, patients can handle chemotherapy’s challenges better. Our healthcare team is dedicated to supporting patients. We provide care that covers both physical and emotional health needs.
As we explore brain tumor chemotherapy, we see better treatment options for patients. We’ve talked about how chemotherapy helps fight brain cancer. This includes overcoming the blood-brain barrier and using different drugs.
Drugs like temozolomide and others are key in treatment plans. Each drug works in its own way and is used for specific cases. Looking ahead, we’ll focus on making these treatments better and finding new ways to deliver them.
With ongoing research, treatments for brain cancer will get even better. This will improve how well treatments work and the quality of life for patients. By keeping up with these advancements, we can offer the best care to those with brain tumors.
Chemotherapy is key in fighting brain tumors. It uses drugs to kill or slow cancer cells. It’s often paired with surgery and radiation therapy.
The blood-brain barrier is a big challenge in treating brain tumors. Some drugs can get past it. Others need special ways to reach the tumor site.
Temozolomide is a drug for glioblastoma. It damages cancer cells’ DNA, stopping them from growing. It’s taken by mouth, often with radiation therapy.
Nitrosoureas, like carmustine and lomustine, treat brain cancer. They mess with cancer cells’ DNA, causing them to die. They can be given by injection or taken orally.
The PCV regimen combines procarbazine, lomustine, and vincristine. It’s for slow-growing brain tumors or those that come back. It targets cancer cells in different ways.
Platinum-based therapies, like cisplatin and carboplatin, damage cancer cells’ DNA. This stops them from growing. They’re used for many brain tumors, often with other drugs.
Side effects include nausea, vomiting, and fatigue. Hair loss and infection risks are also common. The severity varies by drug and patient.
Response is checked with MRI or CT scans and doctor visits. These help see if the tumor is shrinking, staying the same, or growing.
Treatment length varies by tumor type, stage, and drug. It can last from months to over a year.
Support includes managing side effects, nutrition, counseling, and rehab. These help improve life quality during treatment.
Yes, new methods like nanoparticles and implantable devices are being developed. They aim to get drugs to tumors more effectively.
Options include temozolomide, nitrosoureas, PCV, and platinum-based therapies. Treatment choice depends on the glioma type, grade, and location, and the patient’s situation.
Chemotherapy tablets, like temozolomide, are used because they can cross the blood-brain barrier. They offer a convenient oral option instead of injections.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us