Branch retinal vein occlusion (BRVO) with macular edema is a big reason for vision loss. At Liv Hospital, we focus on giving top-notch care for this issue branch retinal vein occlusion oct.
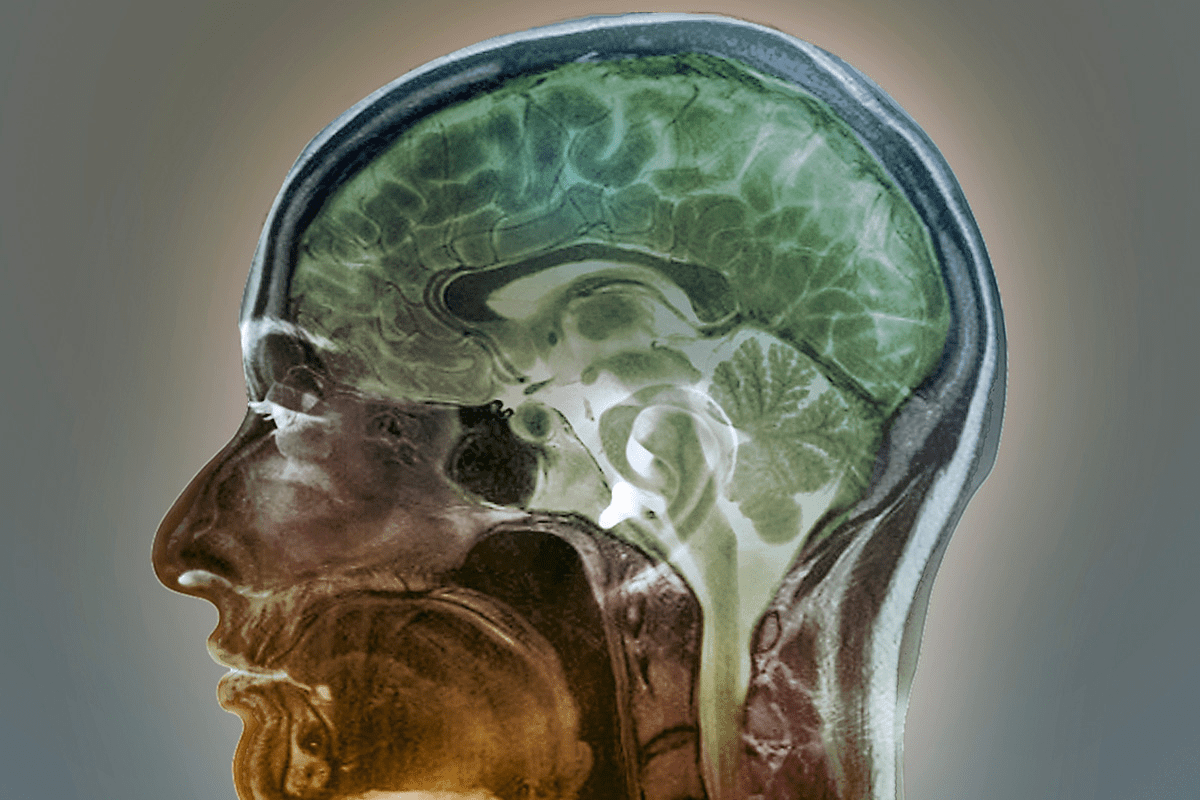
Advances in optical coherence tomography (OCT) imaging have changed how we diagnose and track BRVO with macular edema. OCT helps us give the right treatment, making patients better.
We aim to understand BRVO’s causes. We use OCT for diagnosis and modern treatments for macular edema.
Key Takeaways
- BRVO with macular edema is a leading cause of vision loss.
- OCT imaging plays a critical role in diagnosis and treatment monitoring.
- Effective treatment protocols improve patient outcomes.
- Understanding pathophysiology is key to managing BRVO.
- Modern treatment strategies effectively tackle macular edema.
Understanding Branch Retinal Vein Occlusion (BRVO)
It’s important to understand BRVO to treat it well. We’ll look into what BRVO is, why it happens, and how it shows up in people.
Pathophysiology of BRVO
BRVO happens when a vein in the retina gets blocked. This blockage causes bleeding, swelling, and a lack of blood flow. It’s a mix of blood vessel problems, inflammation, and how blood flows to the retina.
Common Risk Factors
Several things can increase your chance of getting BRVO. High blood pressure, high cholesterol, and glaucoma are some of them. Diabetes and heart disease can also play a part. Knowing these risk factors helps doctors spot who might get BRVO.
Clinical Presentation
BRVO can show up in different ways. People might suddenly see blurry or lose vision. When doctors look into the eye, they see bleeding, white spots, and swelling. How bad it looks depends on where and how much the vein is blocked.
Risk Factor | Association with BRVO |
Hypertension | Strongly associated |
Hyperlipidemia | Associated |
Glaucoma | Associated |
Diabetes Mellitus | May be associated |
The Role of Optical Coherence Tomography (OCT) in BRVO Diagnosis
Optical Coherence Tomography (OCT) has changed how we diagnose and treat Branch Retinal Vein Occlusion (BRVO). It gives us clear images of the retina. This helps us see the layers of the retina, which is key for spotting macular edema and other changes in BRVO.
How OCT Visualizes Macular Edema
OCT shows macular edema by taking detailed pictures of the retina. These pictures help us see how thick the retina is, where fluid is building up, and if there’s any damage. Seeing these details is vital for figuring out how bad the macular edema is and what treatment to use.
OCT Findings in BRVO
In BRVO, OCT shows things like thickened retina, cystoid macular edema, and sometimes a detached retina. OCT can also spot complications like retinal hemorrhage and vitreomacular traction. By looking at these signs, we can see how bad the disease is and track how it changes over time.
Advantages of OCT in Treatment Monitoring
OCT is great for keeping an eye on how treatment is working. By checking the retina’s thickness and shape often, we can tweak the treatment plan. OCT’s exact data helps us see if treatment is working, so we can decide if we need to change it.
In short, OCT is essential for diagnosing and managing BRVO. It lets us see the retina clearly, which helps us spot macular edema, track the disease, and adjust treatments. OCT is a key tool in our work with BRVO patients.
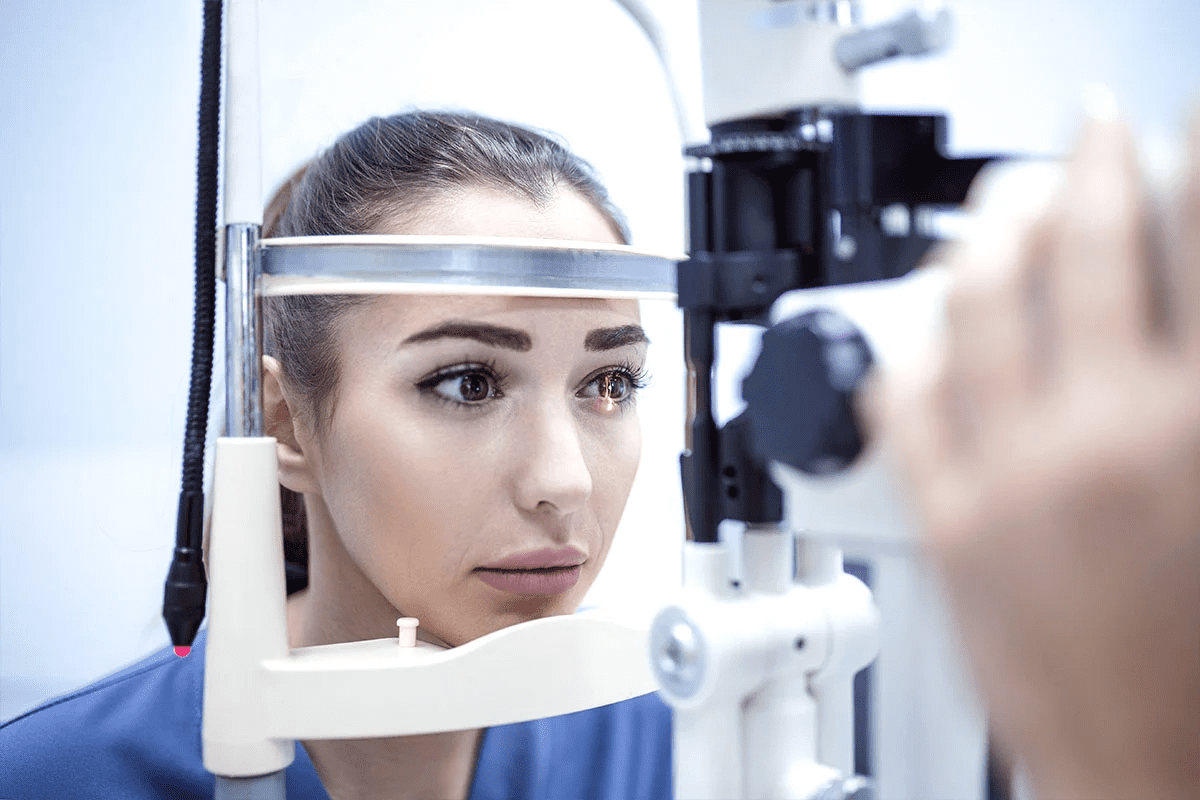
Initial Assessment and Diagnosis
Managing Branch Retinal Vein Occlusion (BRVO) starts with a precise diagnosis. This involves clinical exams and diagnostic tests. We’ll walk you through the steps to accurately diagnose BRVO.
Clinical Examination Techniques
A thorough clinical exam is key for diagnosing BRVO. We employ several methods, including:
- Funduscopy to see the retina and spot signs of BRVO like hemorrhages and edema.
- Optical Coherence Tomography (OCT) to check for macular edema and retinal thickening.
- Fluorescein angiography to look at retinal blood flow and find non-perfused areas.
Differential Diagnosis
When diagnosing BRVO, we must consider other conditions with similar symptoms. A leading ophthalmologist notes,
“Differential diagnosis is key in managing retinal vascular disorders.”
We rule out diabetic retinopathy, retinal artery occlusion, and other macular edema causes.
Classification of BRVO Severity
BRVO severity is classified based on retinal involvement and complications. This helps choose the right treatment. Here’s a summary of the classification criteria:
Severity | Characteristics |
Mild | Limited retinal involvement, minimal edema |
Moderate | Significant retinal hemorrhages, moderate edema |
Severe | Extensive retinal involvement, significant edema, and complications |
By accurately classifying BRVO severity, we can tailor treatments. This optimizes outcomes and improves quality of life.
Anti-VEGF Therapy: First-Line Treatment
In recent years, anti-VEGF therapy has become a key part of treating BRVO. It has greatly helped patients by cutting down on macular edema and boosting their vision.
Mechanism of Action
Anti-VEGF agents stop vascular endothelial growth factor (VEGF) from working. VEGF is a protein that helps blood vessels grow and can make them leak. By stopping VEGF, these agents reduce fluid in the retina, helping vision.
Key benefits of anti-VEGF therapy include:
- Reduction in macular edema
- Improvement in visual acuity
- Potential for regression of neovascularization
Available Anti-VEGF Agents
There are several anti-VEGF agents for treating BRVO, including:
- Ranibizumab (Lucentis): Made for eye use, ranibizumab is effective in reducing macular edema.
- Aflibercept (Eylea): This agent binds to VEGF strongly, making it a strong treatment for BRVO.
- Bevacizumab (Avastin): Though not FDA-approved for eyes, bevacizumab is sometimes used for BRVO off-label.
The choice of anti-VEGF agent can depend on many things, like how the patient responds, insurance, and the doctor’s preference.
Treatment Protocols and Dosing
Anti-VEGF therapy for BRVO usually involves regular eye injections. How often these injections are needed can change based on the agent and the patient’s response.
Common treatment protocols include:
- Monthly injections during the loading phase
- Pro re nata (PRN) dosing, where injections are given as needed based on clinical findings
- Treat-and-extend protocols, which involve gradually extending the interval between injections if the patient remains stable
Expected Outcomes
With anti-VEGF therapy, patients with BRVO can see big improvements in their vision and less macular edema. It’s important to keep an eye on treatment with OCT to make sure it’s working and adjust as needed.
“Anti-VEGF therapy has revolutionized the treatment of BRVO, giving patients a chance to regain vision and improve their quality of life.”
Understanding how anti-VEGF therapy works, the agents available, and the treatment plans helps doctors use it best for BRVO.
Intravitreal Steroid Therapy
Intravitreal steroid therapy is a valuable treatment for patients with Branch Retinal Vein Occlusion (BRVO). It’s used when anti-VEGF therapy doesn’t work well. This method can reduce macular edema and improve vision in BRVO patients.
When to Consider Steroid Treatment
Steroid treatment is for patients who don’t respond to anti-VEGF therapy or have ongoing macular edema. The choice to use intravitreal steroids depends on a detailed patient assessment. This includes the severity of macular edema and any health conditions. We also look at the patient’s medical history and how they’ve reacted to treatments before.
Types of Steroid Implants and Injections
There are different steroid implants and injections for BRVO treatment. These include:
- Dexamethasone implant: A biodegradable implant that slowly releases dexamethasone, a corticosteroid.
- Fluocinolone acetonide implant: A non-biodegradable implant that steadily releases fluocinolone acetonide.
- Triamcinolone acetonide injection: A corticosteroid injection sometimes used off-label for BRVO treatment.
Each option has its own benefits and possible side effects. The right treatment depends on the patient’s specific needs.
Managing Possible Side Effects
Intravitreal steroid therapy can be effective but has side effects like cataract formation and increased eye pressure. Regular monitoring is key to catch and manage these side effects early. We suggest a follow-up plan with regular OCT scans and eye pressure checks to act quickly if needed.
By carefully considering the benefits and risks, we can make intravitreal steroid therapy work best for BRVO patients.
Laser Photocoagulation Techniques
Laser photocoagulation is key in treating Branch Retinal Vein Occlusion (BRVO). It helps manage macular edema and prevent new blood vessels from growing. Over time, new methods have been developed to tackle BRVO’s challenges.
Grid Laser for Macular Edema
Grid laser photocoagulation is a proven method for treating macular edema in BRVO. It uses a grid pattern of laser burns to reduce swelling and improve vision. This technique helps cut down on fluid leakage from retinal capillaries, making the macula thinner.
Benefits of Grid Laser:
- Reduces macular edema
- Improves visual acuity
- Decreases the need for repeated intravitreal injections
Sector Photocoagulation
Sector photocoagulation focuses on areas of retinal ischemia and new blood vessel growth. Laser burns in these spots help reduce new blood vessel formation and prevent bleeding in the vitreous.
Key Considerations:
- Identifying areas of retinal non-perfusion
- Avoiding direct treatment of collateral vessels
- Monitoring for possible side effects
Combination Therapy Approaches
Using laser photocoagulation with other treatments like anti-VEGF therapy or intravitreal steroids can improve results. This approach helps tackle both macular edema and the underlying causes of BRVO more effectively.
Treatment Modality | Primary Benefit | Potential Complications |
Grid Laser | Reduces macular edema | Potential for scotomas, retinal damage |
Sector Photocoagulation | Reduces neovascularization | Risk of retinal ischemia, visual field defects |
Combination Therapy | Enhanced treatment outcomes | Potential for increased risk of side effects |
Understanding different laser photocoagulation techniques helps us create personalized treatment plans. This approach optimizes outcomes in managing BRVO.
Surgical Interventions for Complicated Cases
When Branch Retinal Vein Occlusion (BRVO) causes severe problems, like vitreous hemorrhage or tractional retinal detachment, surgery is needed. These treatments are key for handling tough cases and helping patients get better.
Vitrectomy Indications
Vitrectomy is an option for BRVO patients with big vitreous hemorrhage that doesn’t go away on its own. The choice to do vitrectomy depends on how bad the symptoms are and if there are complications. The main reasons for it include:
- Non-clearing vitreous hemorrhage
- Tractional retinal detachment
- Epiretinal membrane formation
Vitrectomy removes the vitreous gel and any blood or scar tissue that’s pulling on the retina. This surgery can help improve vision and stop more problems.
Arteriovenous Sheathotomy
Arteriovenous sheathotomy is a surgery that cuts the adventitial sheath at the arteriovenous crossing site. This surgery tries to improve blood flow and lessen swelling. It’s a new method, and its use and results are being looked into.
This surgery might help with better retinal circulation and less macular edema. But, it’s important to weigh the risks and benefits for each patient.
Management of Neovascular Complications
Neovascular complications, like new blood vessel growth on the disc or retina, can happen in BRVO patients. Managing it means using laser photocoagulation to treat non-perfusion areas and stop more new blood vessel growth. Sometimes, anti-VEGF therapy is used along with laser treatment.
It’s key to manage neovascular complications well to avoid serious vision loss. Regular checks with fluorescein angiography and OCT are needed to catch and treat these issues early.
In summary, surgery is very important for treating complicated BRVO cases. Knowing when and how to use treatments like vitrectomy, arteriovenous sheathotomy, and laser photocoagulation helps us give our patients the best care.
Long-term Management and Branch Retinal Vein Occlusion OCT Monitoring
Managing BRVO goes beyond the first treatment. It needs ongoing OCT monitoring for the best results. A good long-term care plan must tackle BRVO’s complexities and possible complications.
Follow-up Schedule
A good follow-up plan is key for BRVO care. Regular OCT monitoring helps us see how the retina is doing. We can spot early signs of problems.
Follow-up visits are set up like this:
- Every 4-6 weeks at first
- Every 8-12 weeks later
- More often if needed
Changing the schedule based on the patient’s health helps us act fast. This keeps their treatment on track.
Interpreting OCT Changes Over Time
Understanding OCT changes is important. It shows how BRVO is progressing and if treatment is working. We look for:
- Changes in retinal thickness
- Fluid presence or absence
- New or changing lesions
When to Adjust Treatment
Changing treatment based on OCT is key. We adjust when:
- OCT shows more or lasting edema
- Visual acuity drops
- New or worsening lesions appear
Quick treatment changes can lead to better results and fewer complications.
Managing Recurrent Macular Edema
Dealing with macular edema coming back is a big challenge. We use:
- More or different anti-VEGF therapy
- Other treatments like steroid implants
- Laser treatment in some cases
Being proactive in managing edema helps keep patients’ vision and quality of life good.
Conclusion: Optimizing Outcomes in BRVO with Macular Edema
Managing Branch Retinal Vein Occlusion (BRVO) with macular edema needs a detailed plan. This plan includes accurate diagnosis, choosing the right treatment, and ongoing monitoring. Understanding BRVO’s causes and using tools like Optical Coherence Tomography (OCT) helps a lot.
OCT is very important for diagnosing and tracking BRVO. It shows how bad the macular edema is and helps decide on treatments. There are many treatments, like anti-VEGF therapy, intravitreal steroids, and laser treatments. Each has its own use and benefits.
To get the best results in BRVO care, we must pick the right treatment and keep up with follow-ups. This way, we can handle any new problems and improve patient care. A detailed approach to BRVO management is essential for better patient outcomes and care.
FAQ
What is Branch Retinal Vein Occlusion (BRVO) with macular edema?
BRVO with macular edema happens when a vein in the retina gets blocked. This causes fluid to build up in the macula. This can lead to vision loss.
How is BRVO diagnosed?
Doctors use a detailed eye exam to find BRVO. They look closely at the macula with Optical Coherence Tomography (OCT). This helps see how bad the swelling is.
What are the common risk factors for developing BRVO?
High blood pressure, diabetes, glaucoma, and heart disease can increase your risk of BRVO.
What is the role of OCT in managing BRVO?
OCT is key in managing BRVO. It lets doctors see the swelling in the macula. They can also check how well treatments are working.
What are the treatment options for BRVO with macular edema?
Treatments for BRVO with macular edema include anti-VEGF therapy and laser treatment. Steroids and surgery are also options.
How does anti-VEGF therapy work in treating BRVO?
Anti-VEGF therapy stops the growth of new blood vessels. This reduces swelling in the macula.
What are the possible side effects of intravitreal steroid therapy?
Steroid therapy can cause cataracts, high eye pressure, and infection in the eye.
How is laser photocoagulation used to treat BRVO?
Laser treatment helps by applying laser to the macula. It also treats new blood vessels and ischemia.
What are the indications for vitrectomy in BRVO?
Surgery is needed for BRVO with bleeding, detachment, or swelling that doesn’t get better with other treatments.
How often should patients with BRVO be monitored with OCT?
Patients with BRVO need regular OCT scans. This is usually every 1-3 months. It helps check if treatments are working.
What is the prognosis for patients with BRVO?
The outlook for BRVO patients varies. It depends on how bad the condition is and how well it responds to treatment. Some see big improvements in their vision.
What is the difference between BRVO and CRVO?
BRVO blocks a branch vein, while CRVO blocks the main vein. CRVO usually has a worse outlook.
Can BRVO be treated with combination therapy?
Yes, treating BRVO can involve using more than one method. For example, anti-VEGF therapy with laser treatment can help tackle the condition from different angles.
References
National Health Service (NHS). Treating Branch Retinal Vein Occlusion with Macular Edema. Retrieved from https://www.hey.nhs.uk/patient-leaflet/treatment-options-branch-retinal-vein-occlusion-brvo-2/