Imagine being born without an immune system. Even a simple infection could be fatal. Bubble baby syndrome, or Severe Combined Immunodeficiency (SCID), shows the urgent need for life-saving care for the youngest patients.

SCID is a rare genetic disorder. It affects 1 in 50,000 to 100,000 babies born each year. It’s caused by genetic defects that prevent the immune system from working.
Newborns with SCID are very vulnerable to serious infections. Finding and treating them early is key to saving their lives.
Key Takeaways
- SCID is a rare and life-threatening genetic disorder.
- It affects 1 in 50,000 to 100,000 live births annually.
- Early detection and treatment are critical for survival.
- Newborns with SCID lack a functioning immune system.
- Genetic defects are the main cause of SCID.
The Nature of Bubble Baby Syndrome
Understanding SCID, or Severe Combined Immunodeficiency, means looking into its medical terms and history. We’ll dive into SCID’s details, its nickname origins, and what it means for those affected.
Definition and Medical Terminology
Severe Combined Immunodeficiency (SCID) is a rare group of disorders. They are caused by gene mutations that affect the immune system. SCID severely weakens both T cells and B cells, key parts of our immune system.
This makes it hard for those with SCID to fight off infections. They are at high risk of serious and deadly infections.
The term “combined immunodeficiency” shows that both T cells and B cells are impacted. This makes a more severe condition than disorders affecting only one type of immune cell. The complex medical terms around involve various genetic mutations and immune system problems.
Historical Context of the “Bubble Boy” Name
The nickname “bubble boy disease” comes from David Vetter, an American boy born in 1971 with SCID. He lived in a sterile plastic bubble to avoid infections.

David’s case is a symbol of SCID’s severity. It shows the extreme measures needed to protect those with severe immunodeficiencies. While “bubble boy disease” is well-known, it’s important to remember SCID includes many genetic disorders, not just David’s.
SCID: The Medical Science Explained
To understand , we must first know how the immune system works. Severe Combined Immunodeficiency (SCID) is a serious condition. It makes it hard for the body to fight off infections.
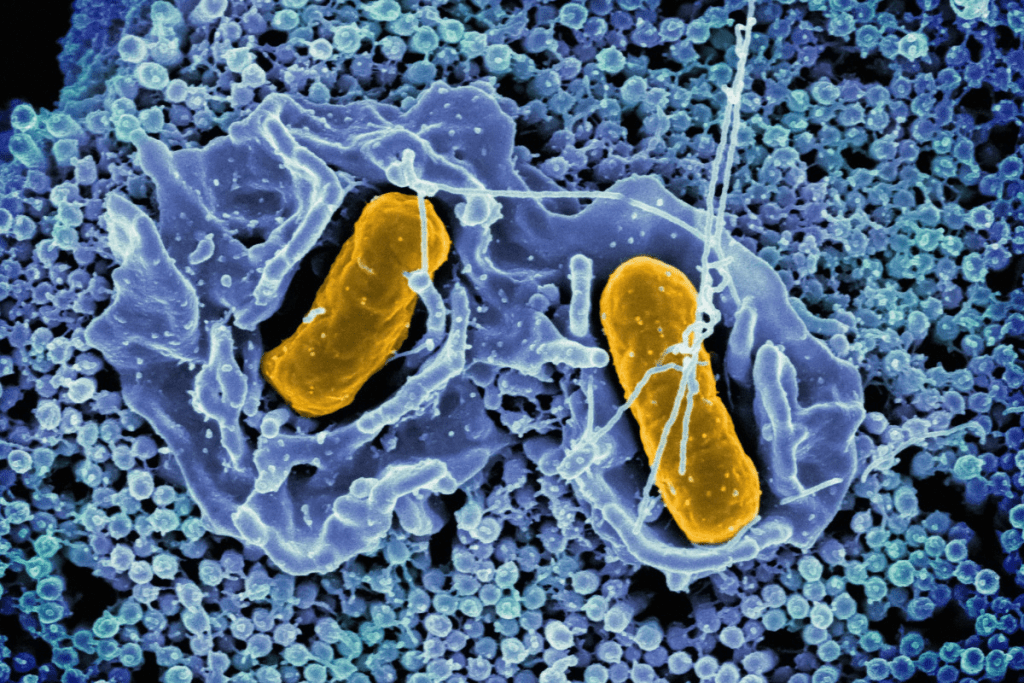
Normal Immune System Function
The immune system is made up of cells, tissues, and organs. They work together to protect the body from invaders like bacteria and viruses. T cells and B cells are key players in this defense.
T cells kill infected cells or help control the immune response. B cells make antibodies to fight off pathogens. A healthy immune system can tell self from non-self and remember past infections to fight better.
Immune System Defects in SCID
In SCID, the immune system can’t fight infections well. This is because T cells and B cells are either missing or don’t work properly. This makes patients very sick from infections.
SCID comes from genetic mutations that harm T cells and B cells. People with SCID can’t fight off infections, leading to serious and sometimes deadly illnesses.
Types of Immune Cells Affected
SCID mainly hits T cells and B cells. T cells kill infected cells or help the immune response. B cells make antibodies to mark pathogens for destruction.
The effects on these cells vary. Some SCID types only affect T cells, while others hit both T cells and B cells. The type of immune cell affected and the defect’s nature can change how shows up and how severe it is.
Genetic Foundations of Bubble Baby Syndrome
Understanding SCID’s genetic roots is key to better treatments and outcomes. SCID is a rare group of disorders. They are caused by mutations in genes vital for the immune system.
X-Linked SCID Mutations
X-linked SCID is a common form. It’s caused by mutations in the IL2RG gene on the X chromosome. This gene makes a protein needed for immune cells to work right. Males are more often affected because they only have one X chromosome.
Autosomal Recessive Forms
There are also autosomal recessive forms of SCID. These are caused by mutations in genes on autosomes. Autosomal recessive SCID can affect both males and females. It requires two mutated alleles to cause the condition.
Genes like ADA, JAK3, and IL7R can lead to autosomal recessive SCID when mutated.
Genetic Diversity in Recent Screening Data
Newborn screening data show a wider range of cases. While X-linked SCID is common, many cases come from autosomal recessive mutations. This diversity shows how complex is and why early genetic screening is vital.
The genetic landscape of is complex, with many genes and mutations involved. Knowing these genetic foundations is essential for developing effective treatments and improving patient outcomes.
Key Genetic Causes of SCID:
- X-linked mutations in the IL2RG gene
- Autosomal recessive mutations in genes such as ADA, JAK3, and IL7R
- A broader genetic diversity revealed by recent newborn screening data
Epidemiology and Demographics
Understanding SCID’s spread is key to better screening and treatment. SCID is rare, affecting a small part of the world’s population. Its occurrence varies widely among different groups.
Global Incidence Rates
SCID is found in about 1 in 50,000 to 1 in 100,000 newborns. This shows how different places and healthcare systems report it differently. Some groups have more cases because of genetic issues linked to SCID.
Regional Variations: In places where families often marry within their families, SCID is more common. For example, in some Middle Eastern and North African countries, the rate is much higher because of genetics and culture.
Demographic Patterns and Risk Factors
SCID mostly hits males, mainly because of X-linked SCID, which makes up about 70% of cases. Genetic counseling and prenatal diagnosis are vital for families with SCID history.
Being at risk includes having a family history of , marrying within the family, and certain genetic issues. Spotting these risks early is key to catching SCID early.
- Family history of SCID
- Consanguineous marriages
- Genetic mutations associated with SCID
Knowing these details helps doctors create better screening plans. This way, they can help more SCID patients.
Recognizing SCID: Symptoms and Warning Signs
It’s vital to spot the signs of SCID early to avoid serious issues. We must know the early signs that show this condition in babies.
Early Clinical Manifestations in Infants
SCID often shows up in the first few months of life. Recurrent infections are a key sign, like pneumonia or meningitis. Babies might also not grow well or have chronic diarrhea.
Some early signs include:
- Frequent or persistent infections
- Failure to gain weight or grow at a normal rate
- Chronic cough or difficulty breathing
- Diarrhea that persists or recurs frequently
Common Infections
Babies with SCID get infections easily because their immune system is weak. Bacterial, viral, and fungal infections are big threats. Common ones are:
- Pneumonia
- Meningitis
- Sepsis
- Chronic diarrhea caused by pathogens such as rotavirus or Candida
These infections can be severe and keep coming back, showing a weak immune system.
Disease Progression Without Intervention
If SCID isn’t treated, it can get worse fast. Without help, babies face serious infections that are hard to treat.
Early detection and treatment are key. Prompt diagnosis and proper treatment can greatly help babies with SCID.
Knowing the symptoms and warning signs of SCID helps us catch it early. This leads to better lives for affected babies.
Diagnostic Approaches for SCID
Understanding how to diagnose SCID is key for early treatment. Doctors use a mix of clinical checks, lab tests, and genetic studies to find SCID.
Newborn Screening Protocols
Newborn screening for SCID is common in many places. It uses a test called T-cell receptor excision circles (TRECs) to spot low T-cell counts. This is a sign of SCID.
The TREC test counts TRECs in a blood spot. Low counts mean might be present, so more tests are needed.
“Newborn screening for SCID has changed how we find this severe disease early,” say experts. This helps doctors act fast to stop serious infections.
Confirmatory Testing Methods
After newborn screening suggests SCID, more tests confirm it. These include:
- Flow cytometry to check T-cell health
- Genetic tests to find SCID-causing mutations
- Tests to see how well B-cells work
Prenatal Diagnosis Options for At-Risk Families
Families with SCID history can get prenatal testing. This genetic test checks if the fetus has SCID. It helps families plan for the baby’s arrival.
Prenatal tests like CVS or amniocentesis are used. They look for SCID-causing mutations. Knowing this early helps manage the condition from the start.
Treatment Modalities for Bubble Baby Syndrome
The treatment for Bubble Baby Syndrome is getting better fast. New therapies are coming up to fight this serious disease. We’ll look at the different treatments for SCID, their hows, whys, and what-ifs.
Bone Marrow Transplantation Procedures
Bone marrow transplants are key in treating SCID. They can cure many patients by replacing their bad immune system with good stem cells. Thanks to new methods, finding a match for patients is easier than before.
- HLA-matched sibling donors
- Haploidentical parental donors
- Unrelated cord blood donors
These new ways to find donors mean more chances for patients to get a transplant.
Gene Therapy Innovations
Gene therapy is a new hope for SCID, focusing on genetic causes. It tries to fix the genetic problem to bring back normal immune function. Early trials show it’s safe and works well for SCID.
The steps are:
- Find the genetic problem
- Get the patient’s stem cells
- Use viruses to fix the gene
- Put the fixed stem cells back in
Though it’s not without its hurdles, gene therapy could be a better, less harsh option than bone marrow transplants.
Immunoglobulin Replacement Therapy (IVIG)
Immunoglobulin Replacement Therapy (IVIG) is vital for many SCID patients. It gives them antibodies to fight off infections. It’s often used with other treatments like transplants or gene therapy.
IVIG helps by:
- Lowering infection risks
- Giving temporary immunity
- Helping during and after transplants
Protective Isolation Protocols
Protective isolation is key for SCID patients. It keeps them safe from harmful germs. This includes:
- Using clean tools and supplies
- Keeping away from sick people
- Washing hands a lot
- Using air filters to clean the air
By using all these treatments together, we can give SCID patients the best care. This improves their survival chances and quality of life.
Multidisciplinary Care for SCID Patients
Managing SCID well needs a team effort from many medical fields. We know that a group of experts is key for top-notch care for SCID patients.
Specialized Medical Team Composition
A specialized medical team is vital for SCID care. This team usually has pediatric immunologists, geneticists, transplant specialists, and more. They all work together to meet SCID patients’ complex needs.
We highlight the role of pediatric immunologists in this team. They are essential for diagnosing and managing SCID, and for making treatment plans.
Coordinated Care Approaches
Coordinated care approaches make sure all SCID aspects are covered, from start to finish. This means the healthcare team talks often, including specialists, primary doctors, and caregivers.
Together, we offer smooth care that fits SCID patients’ complex needs. This improves their health and life quality.
Role of Pediatric Immunologists and Specialists
Pediatric immunologists and specialists are critical in SCID management. They diagnose, plan treatments, and care for patients continuously.
We count on these experts to keep up with SCID treatment advances. This ensures our patients get the latest and best care.
With a multidisciplinary care approach, SCID patient outcomes can greatly improve. This model of care tackles the complex needs of these patients. It gives them the best chance at a healthy life.
Living with Bubble Baby Syndrome
Living with Bubble Baby Syndrome, or Severe Combined Immunodeficiency (SCID), is a tough journey for families. It needs a mix of medical care, lifestyle changes, and emotional support.
Daily Challenges for Families
Families with SCID face big daily challenges. Keeping a clean environment to avoid infections is key. This means using protective isolation protocols that can feel isolating.
Going to the store or social events is hard because of the risk of germs. Managing a child’s SCID medical needs is also complex. This includes regular doctor visits, giving meds, and watching for infections.
The emotional strain of caring for a child with SCID is huge. It affects the whole family’s life quality.
Infection Prevention Strategies
Stopping infections is critical for SCID kids. Families learn about infection prevention strategies like wearing masks and washing hands often. Keeping vaccinations current for everyone helps protect the child too.
Some families use HEPA filters to cut down on airborne germs. These steps, though needed, make life feel limited and require big changes.
Psychological Support Systems
The mental impact of SCID is huge. Kids and families get a lot from psychological support systems. This includes counseling, support groups, and meeting other families with SCID.
Keeping life as normal as possible is key. This means finding a balance between safety and a regular life. Healthcare teams, like pediatric immunologists and psychologists, are essential in this.
Prognosis and Long-term Outcomes
Medical technology and treatment have greatly improved for SCID patients. Early diagnosis and treatment have greatly boosted survival rates and quality of life.
Modern Survival Rates
Newborn screening and better treatments have raised SCID survival rates. Five-year survival rates now range from 87% to 92.5%. This shows how important early treatment is.
Early treatment is key to survival. Factors that help include:
- Early diagnosis through newborn screening
- Advancements in bone marrow transplantation techniques
- Innovations in gene therapy
- Effective infection prevention strategies
Factors Affecting Long-term Prognosis
Several factors affect SCID patients’ long-term outlook. These include when they were diagnosed, if they had infections, and their treatment. Early diagnosis and treatment lead to better outcomes.
Key factors affecting long-term prognosis include:
- The presence of active infections at diagnosis
- The type of SCID and genetic mutation involved
- The timing and type of treatment administered
Quality of Life After Treatment
Improving SCID patients’ quality of life is a major goal. With proper care, many children with SCID can live active lives. They can even thrive as adults.
Improvements in quality of life are attributed to:
- Comprehensive care approaches involving multidisciplinary teams
- Advanced infection prevention strategies
- Psychological support systems for patients and families
In conclusion, SCID patients’ prognosis and long-term outcomes have greatly improved. Ongoing advancements in treatment and care will continue to improve their quality of life.
Conclusion
Understanding SCID is key to helping children with this condition. We’ve learned that early detection and treatment greatly improve survival chances. Newborn screening and quick action have made a big difference.
Early detection is vital. It means we can start treatments like bone marrow transplants and gene therapy right away. These treatments have changed how we treat SCID.
As we learn more about SCID, we see the need for a full approach. This includes special medical care and support services. It’s all about improving the lives of these children.
By focusing on SCID and finding it early, we can help children with this serious condition. This focus is essential for better outcomes.
FAQ
What is Severe Combined Immunodeficiency (SCID)?
SCID, also known as Bubble Baby Syndrome, is a rare and serious genetic disorder. It severely weakens the immune system. This makes people very likely to get infections.
What causes SCID?
SCID is caused by genetic mutations. These mutations affect the development and function of T cells and B cells.
How is SCID diagnosed?
Newborn screening tests for SCID. It measures T-cell receptor excision circles (TRECs). Then, genetic analysis and immune function tests confirm the diagnosis.
What are the symptoms of SCID?
Babies with SCID often get severe infections early. These include pneumonia and meningitis, usually within the first few months.
What are the treatment options for SCID?
Treatments include bone marrow transplantation and gene therapy. Immunoglobulin replacement therapy (IVIG) and protective isolation are also used. These help manage the condition and prevent infections.
How effective is newborn screening for SCID?
Newborn screening is key in finding SCID early. This early detection leads to better treatment and survival rates.
What is the prognosis for children with SCID?
Early treatment has greatly improved survival rates. Children with SCID can now live active lives with proper care.
How does SCID affect families?
SCID brings daily challenges for families. They must manage infections and isolation. This shows the need for psychological support.
What is the role of a multidisciplinary team in managing SCID?
A team of pediatric immunologists, geneticists, and transplant specialists provides care. They work together from diagnosis to treatment and follow-up.
Can SCID be prevented?
SCID is a genetic disorder that can’t be prevented. But early detection through newborn screening and timely treatment can greatly improve outcomes.
References
- Kohn, D. B., Hershfield, M. S., & Puck, J. M. (2025). Severe Combined Immunodeficiency – StatPearls. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK539762/
- Orphanet. (2008, February 5). Severe combined immunodeficiency. Orphanet Journal of Rare Diseases. https://www.orpha.net/en/disease/detail/183660
- National Institute of Allergy and Infectious Diseases (NIAID). (2025, June 15). Severe Combined Immunodeficiency (SCID). Primary Immune Deficiency Disease. https://primaryimmune.org/understanding-primary-immunodeficiency/types-of-pi/severe-combined-immunodeficiency-scid
- Medscape. (2024). Severe Combined Immunodeficiency (SCID). Medscape Overview. https://emedicine.medscape.com/article/210249-overview
- Wikipedia contributors. (2025, May 23). Severe combined immunodeficiency. Wikipedia. https://en.wikipedia.org/wiki/Severe_combined_immunodeficiency








