Last Updated on October 31, 2025 by Bilal Hasdemir
Carcinoma in situ (CIS) of the bladder is a serious but treatable bladder cancer. It is in its early stages and is considered high-grade. CIS is a non-invasive but aggressive cancer that can become invasive if not treated. What is CA in situ bladder? Learn about this early-stage, high-risk type of non-muscle-invasive bladder cancer.
At Liv Hospital, we see CIS as a unique challenge. It is hard to spot because it doesn’t show symptoms early. But, if caught and treated quickly, it can be stopped from getting worse.
CIS of the bladder is an early-stage cancer but is very aggressive. It’s important to know what CIS is, its role in bladder cancer, and its high-grade nature.
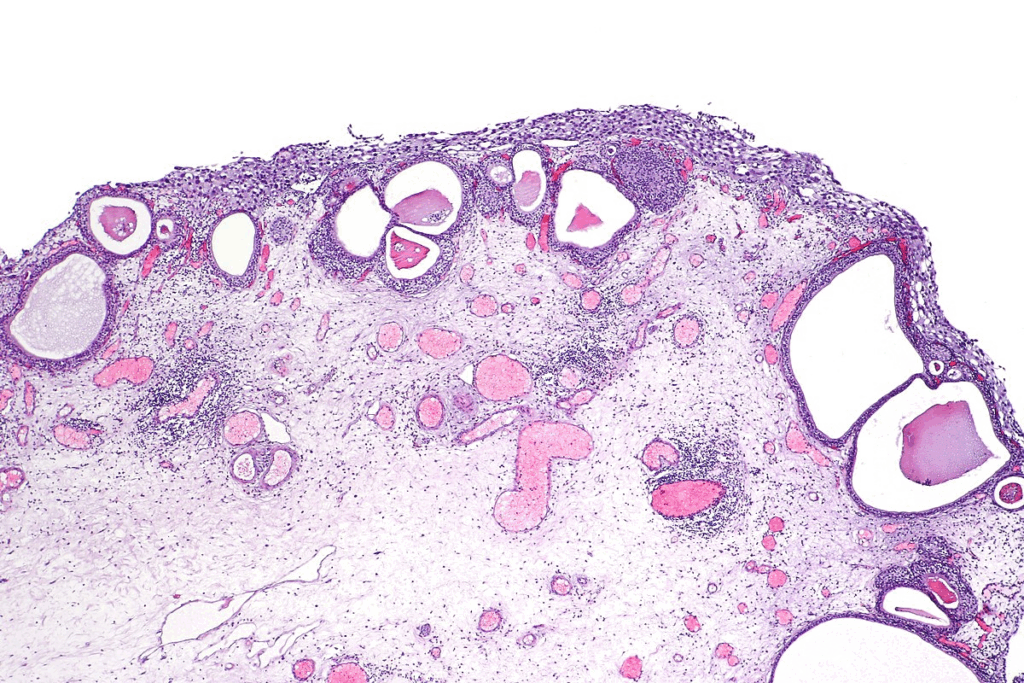
CIS is a type of bladder cancer that hasn’t spread deep into the bladder. It’s classified as stage 0 and is a non-muscle-invasive bladder cancer (NMIBC).
Bladder cancer is divided into stages and grades to guide treatment. CIS is stage 0 and high-grade, making it key in this system.
CIS is both early-stage and high-grade, which is tricky to handle.
In summary, CIS of the bladder is complex. It needs careful handling because of its aggressive nature and risk of getting worse.

Understanding CIS of the bladder is key because it can turn into invasive cancer. CIS is a serious, non-invasive bladder cancer. It can become muscle-invasive bladder cancer if not treated right.
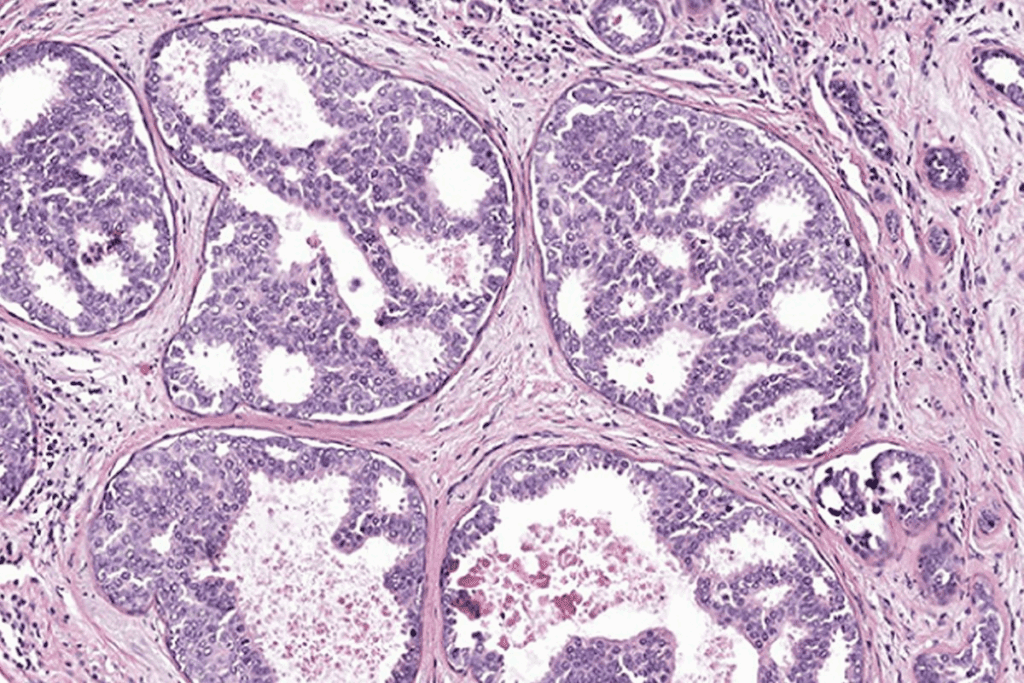
CIS has severely dysplastic urothelial cells that haven’t invaded the bladder wall. These cells show nuclear atypia, like big nuclei and irregular shapes. CIS cells are often disorganized and lose normal cell structure.
Nuclear atypia in CIS shows its cancer risk. Cells in CIS have dark nuclei due to more DNA. They also vary in size and shape, showing they are cancerous.
CIS cells also change in cytoplasm, like density and structure. These changes help doctors diagnose CIS and tell it apart from less serious urothelial lesions.
CIS is different from other bladder cancers, like low-grade papillary urothelial carcinoma. CIS is flat and non-papillary, making it hard to spot during cystoscopy. Unlike papillary tumors, CIS doesn’t grow in a papillary shape.
| Characteristics | CIS | Low-Grade Papillary Urothelial Carcinoma |
| Growth Pattern | Flat, non-invasive | Papillary, non-invasive |
| Nuclear Atypia | Significant, high-grade | Minimal, low-grade |
| Potential for Invasion | High | Low |
Knowing these differences is vital for the right treatment. CIS needs aggressive treatment because of its high risk of becoming invasive cancer.
The study of CIS of the bladder helps us understand its spread and causes. Knowing this is key to spotting who’s at risk and how to help them.
Carcinoma in situ (CIS) of the bladder is a serious, non-invasive cancer. It’s a big part of bladder cancer cases. De novo CIS is rare, making up less than 3% of all bladder cancers. But, it’s more common in people who’ve had bladder cancer before.
Prevalence studies show CIS often comes with other bladder cancers. It can be the first sign or come after a bladder cancer diagnosis.
Several things increase the risk of CIS of the bladder, including:
CIS of the bladder is more common in older adults, mostly over 60. Men are more likely to get it than women.
Understanding these patterns helps us focus on screening and prevention for those at highest risk.
Bladder CIS can be classified into primary, secondary, and concomitant subtypes. Each subtype has its own clinical significance. This classification helps doctors understand the disease better and choose the right treatment.
Primary CIS is when CIS appears without any history of papillary tumors. It often needs a different treatment plan than the other subtypes.
Secondary CIS occurs after a diagnosis of papillary tumors or other bladder cancers. It can be tough to manage because of its history and possible resistance to treatments.
Concomitant CIS is found with papillary tumors. It poses a unique challenge because both need to be treated at the same time.
Knowing the CIS subtype is very important. It helps doctors make better treatment plans and predict how well a patient will do.
To show the differences and importance of these subtypes, let’s look at a table:
| CIS Subtype | Characteristics | Clinical Implications |
| Primary CIS | No prior history of papillary tumors | Different management strategy; potentially more aggressive |
| Secondary CIS | Develops after prior diagnosis of papillary tumors | Challenging management due to history of previous treatments |
| Concomitant CIS | CIS occurs alongside papillary tumors | Need to address both CIS and papillary tumors simultaneously |
Understanding the CIS subtype helps doctors tailor treatments. This can lead to better outcomes for patients.
Understanding CIS bladder cancer symptoms is key to early detection and treatment. CIS of the bladder can show different symptoms, making it hard to diagnose on time.
Hematuria is a common symptom of CIS bladder cancer. It can be visible to the eye (gross) or only seen under a microscope (microscopic). Gross hematuria makes urine look pink, red, or cola-colored. Microhematuria is smaller and only visible under a microscope.
Both types of hematuria can point to CIS, but other issues can cause them too.
Patients with CIS bladder cancer may also have other urinary symptoms. These include:
These symptoms can really affect a person’s life and may lead them to see a doctor.
Some people with CIS bladder cancer won’t show any symptoms. They might find out about it during tests for other urinary problems or through screening.
If you keep getting urinary symptoms like hematuria, frequent urination, or pain while urinating, see a doctor. Early diagnosis is very important for managing CIS bladder cancer.
| Symptom | Description | Action |
| Gross Hematuria | Visible blood in urine | Seek medical attention |
| Microhematuria | Microscopic blood in urine | Discuss with healthcare provider |
| Urinary Symptoms | Frequency, urgency, dysuria | Consult a urologist |
Diagnosing CIS bladder cancer needs a mix of tools. It’s key for managing and treating the disease well.
Cystoscopy is a key step in diagnosing CIS bladder cancer. It uses a cystoscope to look at the bladder lining. A biopsy is taken during this to check the tissue samples.
Biopsy results are vital. They show the cell structure and any issues. Cystoscopy and biopsy together are the best way to diagnose CIS bladder cancer.
Urine cytology checks urine for abnormal cells. It’s useful but not always accurate for CIS. It’s best used with other tests.
Biomarkers in urine or tissue help diagnose bladder cancer. They spot genetic or molecular changes in CIS.
Imaging like CT scans or MRI helps see how far cancer has spread. But, they can miss CIS because it’s flat and non-invasive.
New tests in molecular and genetic fields help with CIS bladder cancer. They find specific genetic changes in CIS. This improves diagnosis and treatment planning.
We’re moving towards more tailored treatments for CIS bladder cancer. We’re using the latest in medical tech and research.
Understanding how to treat CIS of the bladder is key. Treatment often includes intravesical therapy, which is put directly into the bladder.
Intravesical Bacillus Calmette-Guérin (BCG) therapy is the top choice for CIS of the bladder. BCG therapy uses a weakened form of the Mycobacterium bovis bacterium in the bladder. It helps the body fight cancer cells. Many patients see their cancer clear up thanks to BCG therapy.
For those who can’t take BCG or have cancer come back, intravesical chemotherapy is an option. Mitomycin C is a common chemotherapeutic agent used in this way. It’s not as effective as BCG but is a valuable choice.
If BCG therapy doesn’t work, surgery might be needed. Radical cystectomy, which removes the bladder, is a big surgery for high-risk or resistant cases. It’s often paired with urinary diversion procedures.
New treatments for CIS are being researched. Checkpoint inhibitors and other immunotherapies are being looked at. They aim to boost the body’s fight against cancer. As we learn more about CIS, we’ll see better treatments come along.
Knowing how CIS affects bladder cancer is key. It helps set patient hopes and guides treatment. The outcome for CIS of the bladder changes a lot. This depends on how well treatment works and the patient’s health.
CIS can turn into invasive bladder cancer. This is a big worry. Studies show that without proper treatment, CIS can lead to invasive disease.
Survival rates for CIS are good if caught early and treated right. But, long-term results depend on treatment success and patient follow-up.
| Treatment Response | 5-Year Survival Rate |
| Complete Response | 90% |
| Partial Response | 70% |
| No Response | 40% |
Many things can change CIS prognosis. These include the cancer’s stage, other health issues, and the patient’s age and health.
Key Prognostic Factors:
Dealing with CIS means treating the disease and improving life quality. This includes handling side effects and supporting the patient’s mental health.
Understanding CIS prognosis helps doctors give better care. This improves patient outcomes and life quality.
Managing carcinoma in situ (CIS) of the bladder is key. It needs a mix of prevention, regular checks, and treatment. This helps stop the disease from getting worse and improves life quality.
To lower CIS risk, making lifestyle changes is important. Stopping smoking is a big step, as it’s a major risk factor. Eating more fruits and veggies and avoiding harmful chemicals also helps.
Staying away from harmful substances and chemicals is also good. Talking to a doctor can help make a plan to reduce risk.
Regular check-ups are vital for CIS management. This includes cystoscopy and urine cytology as often as needed. The schedule depends on the patient’s risk level.
| Surveillance Method | Frequency | Purpose |
| Cystoscopy | Every 3-6 months | Visual examination of the bladder |
| Urine Cytology | Every 3-6 months | Detection of cancer cells in urine |
| Imaging Studies | As needed | Assessment of tumor extent and metastasis |
It’s important to manage CIS treatment side effects. Intravesical BCG therapy can cause issues like frequent urination. Medications can help with these symptoms.
Patients should tell their doctors about any side effects. This way, treatment plans can be adjusted to be more comfortable.
Dealing with CIS affects not just the body but also the mind. Psychological support and resources are essential. This includes counseling, support groups, and educational materials.
By focusing on prevention and management, CIS patients can do better. We aim to offer the support and care they need on their journey.
Getting a diagnosis of carcinoma in situ (CIS) of the bladder can be tough. But, with the right treatment and support, patients can handle it well. Managing bladder cancer means getting medical help, making lifestyle changes, and getting psychological support.
A CIS diagnosis might seem scary, but it’s key to know CIS is a step before cancer spreads. Early action can really help. Understanding CIS helps patients choose the best treatment and care for themselves.
For those with bladder cancer, having a supportive group is vital. This includes doctors, family, and friends. It’s also important to stick to follow-up and watch plans to keep the condition in check and handle side effects.
By being active and well-informed in managing CIS, patients can live better and lower the chance of the disease getting worse. We aim to give top-notch healthcare and support to patients from around the world. We want to help them get the care and advice they need on their journey.
Carcinoma in situ (CIS) of the bladder is an early-stage bladder cancer. It is high-grade and can become invasive if not treated.
Symptoms include gross hematuria, microhematuria, and urinary discomfort. Some people may not show symptoms, making regular check-ups key.
Doctors use cystoscopy, biopsy, urine cytology, and imaging to diagnose CIS bladder cancer. Molecular and genetic tests also help.
Treatments include intravesical BCG therapy and chemotherapy. Surgery is used for BCG-resistant cases. New treatments are being researched.
The prognosis depends on several factors. These include the risk of invasive disease, survival rates, and long-term outcomes. Quality of life is also important.
While CIS bladder cancer can’t be fully prevented, avoiding smoking and reducing chemical exposure can lower the risk.
CIS bladder cancer is classified into primary, secondary, and concomitant types. Each type has its own treatment and prognosis implications.
CIS is unique due to its early-stage and high-grade nature. It has the ability to become invasive. Understanding these differences is key for diagnosis and treatment.
Risk factors include smoking, chemical exposure, and demographic patterns. Knowing these can help identify at-risk populations.
Surveillance frequency varies based on individual circumstances. Regular check-ups and screenings are essential for monitoring any changes or progression.
Patients can access psychological support, resources, and guidance. This helps manage treatment side effects and improve quality of life.
“Ca in situ” means cancer that stays in its original location. It hasn’t invaded surrounding tissues.
CIS bladder cancer is non-invasive but can become invasive if not treated or managed properly.
National Center for Biotechnology Information. (2025). What Is Carcinoma In Situ of the Bladder. Retrieved from https://pubmed.ncbi.nlm.nih.gov/19176205/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us