Last Updated on November 26, 2025 by Bilal Hasdemir

At Liv Hospital, we know that trust and safety are key. That’s why understanding the risks of medical procedures is important. Nerve damage from an epidural is a rare but possible issue that patients should know about.
Epidural anesthesia is a common way to manage pain during childbirth and surgeries. It involves putting anesthetic into the space around the spinal cord. While it’s usually safe, there are risks, including nerve injury.
We aim to offer top-notch healthcare with full support for international patients. Knowing about the link between epidural anesthesia and nerve damage helps patients make better choices.
Key Takeaways
- Nerve damage from epidural anesthesia is a rare complication.
- Direct needle injury, local hematoma, infection, or reduced blood supply can lead to nerve damage.
- Most cases of nerve damage from epidural are temporary.
- Epidural anesthesia is commonly used for pain relief during childbirth and surgeries.
- Liv Hospital provides complete care and support for patients undergoing epidural anesthesia.
Understanding Epidural Anesthesia and Its Purpose
Epidural anesthesia is key for those having surgeries or giving birth. It’s a safe way to manage pain. It works by injecting medicine into the space around the spinal cord, blocking pain and movement.
What Is an Epidural and How Does It Work?
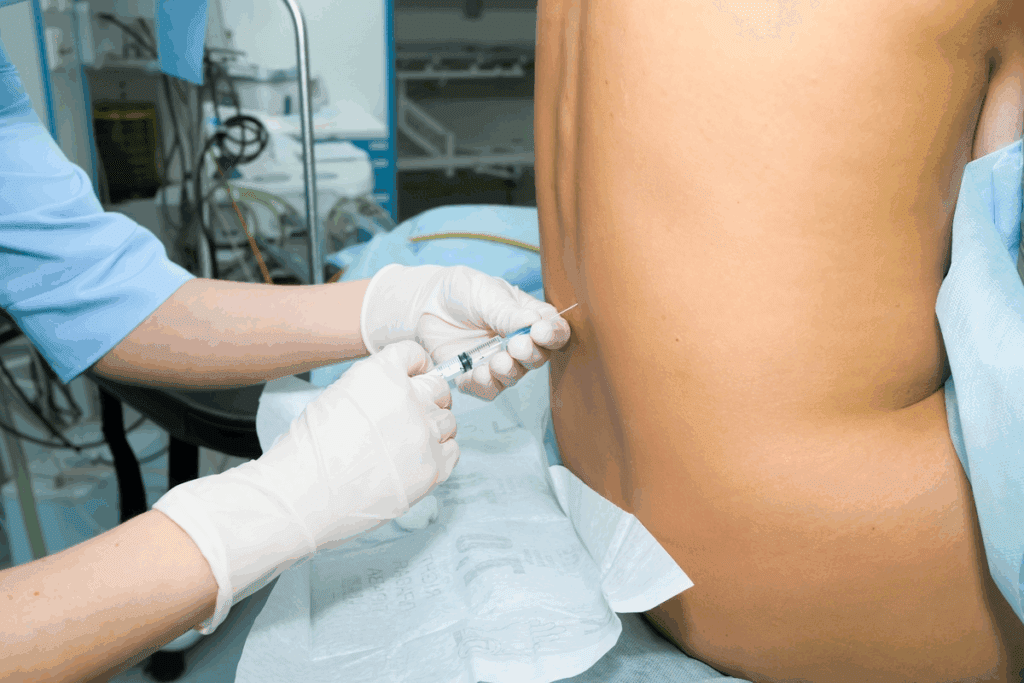
An epidural numbs the lower body. A needle is inserted into the epidural space. A catheter is then used to give medicine as needed.
The process works as follows:
- The patient is positioned to allow easy access to the epidural space.
- A local anesthetic is used to numb the skin where the epidural needle will be inserted.
- The epidural needle is carefully inserted, and once in place, a catheter is threaded through it.
- The needle is then removed, leaving the catheter in place for ongoing pain relief.
Common Medical Uses for Epidural Procedures
Epidural anesthesia is used for many things. This includes childbirth, surgeries on the lower body, and managing chronic pain. It’s a popular choice because it’s effective and safe.
| Medical Use | Description | Benefits |
| Childbirth | Pain relief during labor | Effective pain management, allows mothers to be more comfortable during delivery |
| Surgical Procedures | Anesthesia for lower abdominal and leg surgeries | Reduces pain, minimizes the need for general anesthesia |
| Chronic Pain Management | Ongoing pain relief for chronic conditions | Provides long-term pain management, improves quality of life |
Knowing how epidural anesthesia works and its uses helps patients understand its benefits and risks. This knowledge is important for making informed decisions.
Can an Epidural Cause Nerve Damage? The Reality of Risks
Epidural anesthesia is a common method for managing pain. But, it can also lead to nerve damage. We will look into how often this happens and what kind of nerve damage it can cause.
Frequency of Nerve Damage Complications
Nerve damage from an epidural is rare. Research shows that most nerve damage from epidurals is temporary. The chance of lasting nerve damage is less than 1 in 1,000. This low risk is good news for those thinking about epidural anesthesia for pain relief.
“The risk of nerve damage from epidural anesthesia, though small, is a big worry for patients and doctors,” experts say.
Temporary vs. Permanent Nerve Damage
It’s important to know the difference between temporary and permanent nerve damage. Most nerve damage from epidurals is temporary. It usually shows up as numbness, tingling, or weakness.
But, permanent nerve damage is rare and can have lasting effects. It can lead to chronic pain, numbness, or mobility problems. Knowing the risk of permanent damage helps understand the overall risks of epidural anesthesia.
It’s key to understand the difference between temporary and permanent nerve damage. This helps manage patient expectations and provide the right care. By knowing the risks and how to reduce them, doctors can help patients get the best results from epidural procedures.
Key Fact #1: Mechanisms of Nerve Injury During Epidural Procedures
Nerve injury from epidural procedures can happen in many ways. It’s important to know these causes to reduce risks and handle problems well.
Direct Needle Trauma to Nerves
Needle trauma is a big reason for nerve injury during epidurals. When the needle hits a nerve, it can hurt it. This can cause anything from a little numbness to a lot of pain or weakness.
Epidural Hematoma Formation
An epidural hematoma can also hurt nerves. This is when blood builds up and presses on nerves. It can lead to pain, weakness, or numbness.
Infection-Related Nerve Damage
Infections from epidural procedures can also damage nerves. Infections cause inflammation and harm to nerves. It’s key to treat infections quickly to avoid lasting nerve damage.
| Mechanism of Nerve Injury | Potential Consequences |
| Direct Needle Trauma | Numbness, pain, weakness |
| Epidural Hematoma | Compression, pain, weakness |
| Infection | Inflammation, nerve damage |
Understanding complications helps manage and lower risks.
Key Fact #2: Recognizing Symptoms of Nerve Damage from Epidural
It’s important to know the signs of nerve damage from epidural anesthesia early. This damage can cause many symptoms that affect a person’s health in different ways.
Sensory Symptoms: Numbness, Tingling, and Pain
Sensory symptoms are common signs of nerve damage from epidural anesthesia. People might feel numbness or tingling in certain areas. Sometimes, chronic pain can also occur, making life harder.
These feelings can be mild or very strong. Some symptoms last only a short time, while others can be long-lasting and very serious.
Motor Symptoms: Weakness and Mobility Issues
Nerve damage can also cause motor symptoms like weakness and mobility issues. This makes it hard to do everyday tasks because of muscle weakness or paralysis.
In severe cases, these symptoms can make it hard to walk or do physical activities. This might need physical therapy and rehabilitation.
Autonomic Symptoms: Bladder and Bowel Dysfunction
Some people may also have autonomic symptoms like bladder and bowel dysfunction. These can show up as trouble with urination, incontinence, or constipation.
These symptoms can be very upsetting and need special medical care to manage.
It’s key to spot these symptoms early for proper treatment. Knowing about these symptoms helps doctors give better care and improve patient results.
Key Fact #3: Timeline of Epidural Nerve Damage Symptoms
Knowing when nerve damage symptoms show up after an epidural is key. These symptoms can appear at different times. Knowing when they might happen helps both patients and doctors catch and treat problems early.
Immediate Post-Procedure Symptoms
Some people feel nerve damage right after the epidural. They might notice numbness, tingling, or pain in their legs or lower back. It’s very important to see a doctor right away if this happens, as it could be a serious issue.
Short-Term Complications (1-4 Weeks)
For others, nerve damage symptoms might not show up right away but can start a few weeks later. During this time, they might feel more pain, weakness, or numbness in certain areas. It’s important to keep an eye on these symptoms and talk to a doctor about them.
Long-Term or Persistent Symptoms
Some people might experience nerve damage symptoms that last a long time after the epidural. These symptoms can really affect a person’s life, needing ongoing care and possibly more serious treatments.
| Timeline | Possible Symptoms | Recommended Action |
| Immediate | Numbness, tingling, pain | Seek immediate medical attention |
| Short-Term (1-4 weeks) | Increasing pain, weakness, numbness | Monitor symptoms, consult healthcare provider |
| Long-Term | Persistent pain, weakness, numbness | Ongoing medical care, possible further treatment |
By knowing when nerve damage symptoms might happen after an epidural, patients can better manage their recovery. They can work closely with their doctors to handle any issues that come up.
Key Fact #4: Diagnosing Nerve Damage After Epidural Procedures
Getting a correct diagnosis is key to handling nerve damage from epidural anesthesia. Finding out if nerve damage has occurred after an epidural needs a detailed look. This helps us understand how bad the injury is.
Medical Evaluation Process
The first step is to look at the patient’s medical history and symptoms. We check the patient’s health, the epidural procedure details, and any symptoms or problems that followed. A careful physical exam is done to check for nerve damage signs like numbness, tingling, or weakness.
We also look at when the symptoms started. Did they happen right after the epidural, or later? Knowing this helps us figure out the cause and how bad the damage is.
Diagnostic Tests and Imaging
To confirm the diagnosis and see how bad the nerve damage is, we use diagnostic tests and imaging studies. These include:
- Electromyography (EMG) to check muscle electrical activity.
- Nerve conduction studies (NCS) to see how well nerves send signals.
- Magnetic Resonance Imaging (MRI) to see the nerves and tissues around them.
These tools help us find where and how bad the nerve damage is. This guides us in creating a treatment plan that fits the patient’s needs. Getting the diagnosis right is the first step to recovery.
Key Fact #5: Risk Factors That Increase Chances of Epidural Nerve Injury
It’s important to know the risks of nerve injury from epidural procedures. Both doctors and patients need to understand these risks. Knowing them helps us work together to avoid problems and get the best results.
Pre-existing Medical Conditions
Medical conditions before the epidural can raise the risk of nerve damage. Diabetes, multiple sclerosis, and peripheral neuropathy can harm nerves. Also, people with bleeding problems or on blood thinners might face more risks of nerve damage.
Anatomical Considerations
How your body is shaped can also affect nerve injury risks. Spinal issues like scoliosis or past surgeries can make epidural placement tricky. Spinal stenosis or other problems can bring nerves closer to the epidural space, raising injury risks.
Procedural Risk Factors
Many things during the epidural can impact nerve damage risks. The doctor’s experience and skill are key. The method used, like the needle type and placement, also matters. More attempts or hard placements can increase risks.
Knowing these risks helps doctors decide if an epidural is safe for you. This knowledge lets them take steps to lower risks. It makes epidural anesthesia safer for everyone involved.
Key Fact #6: Treatment Options for Nerve Damage from Epidural
Treating nerve damage from epidural procedures involves different methods. These range from simple treatments to surgery. The right treatment depends on how bad the nerve damage is and the patient’s health.
Conservative Management Approaches
For mild to moderate nerve damage, simple treatments work well. These include:
- Medications to manage pain and discomfort
- Physical therapy to maintain or improve mobility and strength
- Lifestyle modifications to reduce strain on the affected area
Conservative management is usually the first step. It can help manage symptoms and aid in recovery.
Physical Therapy and Rehabilitation
Physical therapy is key in treating nerve damage from epidural procedures. A custom rehabilitation plan can help patients regain strength and mobility. It also reduces pain. Rehabilitation works best when started early.
| Therapy Type | Benefits | Duration |
| Physical Therapy | Improves mobility and strength | Several weeks to months |
| Occupational Therapy | Enhances daily functioning | Variable, based on patient needs |
Surgical Interventions for Severe Cases
For severe or lasting nerve damage, surgical intervention might be needed. Surgery can relieve nerve pressure, repair nerves, or stabilize the spine.
Choosing surgery depends on the patient’s specific situation and health.
Key Fact #7: Recovery Expectations and Prognosis
Recovering from nerve damage after an epidural is complex. It depends on many factors. Knowing what to expect helps doctors give better care and treatment plans.
The road to recovery is influenced by how bad the nerve damage is, the treatment’s success, and the patient’s health. We’ll look at the usual recovery time and what can change it.
Typical Recovery Timeline
Recovery times for nerve damage from epidural anesthesia vary a lot. Some see improvement in weeks, while others take months or more.
Immediate Recovery: Sometimes, symptoms go away right after the epidural stops. But, nerve damage can cause lasting symptoms.
Short-term Recovery: The first few weeks are key for many. Some start feeling better during this time.
Factors Affecting Recovery Outcomes
Many things can change how well a patient recovers from nerve damage. These include:
- The severity of the nerve damage
- The success of the treatment plan
- The patient’s health and any existing conditions
- How quickly and well medical help is given
| Factor | Influence on Recovery |
| Severity of Nerve Damage | More severe damage often results in longer recovery times |
| Effectiveness of Treatment | Good and timely treatment can greatly improve outcomes |
| Patient’s Overall Health | Existing conditions can make recovery harder |
Understanding these factors and the usual recovery time helps doctors. They can manage patient hopes and create better treatment plans for nerve damage from epidural procedures.
Preventing Epidural Injury and Nerve Damage
Exploring epidural anesthesia shows us how important it is to prevent nerve damage. This task needs both medical skill and patient knowledge.
Stopping nerve damage from epidural procedures is complex. It requires careful steps from healthcare teams and patients. Best practices in medical care are key to lowering risks from epidural anesthesia.
Best Practices for Medical Professionals
Doctors can lower nerve damage risks by following guidelines and using careful techniques. This includes:
- Using advanced imaging to guide the epidural needle placement accurately.
- Knowing spinal anatomy well to avoid nerve damage.
- Watching patients closely during and after the procedure for any signs of trouble.
Continuous education and training for doctors are vital. They need to keep up with new techniques and best practices in epidural anesthesia.
Patient Preparation and Considerations
Patient preparation is also key in preventing nerve damage from epidural anesthesia. This involves:
- Teaching patients about the risks and benefits of epidural procedures.
- Doing thorough checks before the procedure to find any risks.
- Making sure patients know to report any symptoms or discomfort during or after the procedure.
By working together, doctors and patients can lower the risk of epidural nerve injury. This makes the experience safer for everyone.
When to Seek Immediate Medical Attention for Epidural Nerve Damage Symptoms
It’s important to know the signs of nerve damage after an epidural. Some symptoms need quick medical help to avoid lasting damage. This ensures the best results.
Red Flag Symptoms Requiring Emergency Care
Some symptoms mean you need to see a doctor right away. These include:
- Severe pain that can’t be controlled with medicine
- Progressive weakness or numbness in the legs
- Bladder or bowel dysfunction, like trouble urinating or losing bowel control
- Sudden severe headache or back pain
If you have any of these red flag symptoms, get medical help fast. Quick action can greatly improve your recovery and health.
Communicating Effectively With Healthcare Providers
Talking clearly with your healthcare team is key when you have nerve damage symptoms. Tell them about your symptoms, when they started, and what makes them better or worse.
Keeping a symptom journal is a good idea. It helps your healthcare team understand your situation better. They can then make better decisions for your care.
Don’t be shy about asking questions about your symptoms or treatment. Your healthcare providers are there to help you. They want to make sure you get the best care possible.
Conclusion: Balancing Benefits and Risks of Epidural Procedures
We’ve looked into epidural anesthesia and its effects on patients. It’s a key method for managing pain but comes with risks, like nerve damage.
It’s important to know about the risks, symptoms, and treatments for nerve damage from epidurals. This knowledge helps patients and doctors make better choices together.
It’s key to balance the good and bad of epidural procedures. We need to consider the pain relief it offers against the chance of nerve damage.
By understanding these aspects, we can give patients the best care. This means knowing what might happen and helping them choose wisely.
FAQ
What is the risk of nerve damage from an epidural?
Nerve damage from an epidural is rare. It can happen due to direct needle trauma, epidural hematoma, or infection.
Can epidural anesthesia cause permanent nerve damage?
Most nerve damage from an epidural is temporary. But, there’s a small chance of permanent damage in rare cases.
What are the symptoms of nerve damage from an epidural?
Symptoms include numbness, tingling, and pain. You might also feel weakness, have trouble moving, or face bladder and bowel issues.
How is nerve damage from an epidural diagnosed?
Doctors check your symptoms and medical history. They might use tests and imaging to diagnose nerve damage.
What are the treatment options for nerve damage from an epidural?
Treatment includes non-surgical methods, physical therapy, and rehabilitation. In severe cases, surgery might be needed.
Can pre-existing medical conditions increase the risk of nerve damage from an epidural?
Yes, certain health conditions and anatomical variations can raise the risk of nerve damage after an epidural.
How can nerve damage from an epidural be prevented?
Preventing nerve damage involves proper technique and patient selection by doctors. Patient education and preparation are also key.
What are the red flag symptoms that require immediate medical attention after an epidural?
Severe pain, progressive weakness, and bladder or bowel issues are red flags. Seek medical help right away if you experience these symptoms.
Can epidural cause nerve damage in the leg?
Yes, epidural anesthesia can cause nerve damage in the leg. Symptoms include numbness, tingling, and weakness.
What is the typical recovery timeline for nerve damage after an epidural?
Recovery time varies. Most people recover fully within a few weeks or months after an epidural.
How can I communicate effectively with my healthcare provider about epidural nerve damage symptoms?
To communicate well, report symptoms or concerns promptly and clearly. Seek immediate help if you notice red flag symptoms.
References
- Ruppen, W., Derry, S., McQuay, H., & Moore, R. A. (2006). Incidence of epidural hematoma, infection, and neurologic injury in obstetric patients with epidural analgesia/anesthesia. Anesthesiology, *105*(2), 394–399. https://pubmed.ncbi.nlm.nih.gov/16871076/






