Last Updated on December 3, 2025 by mcelik
Did you know that nearly 3% of adults in the United States suffer from carpal tunnel syndrome? This condition affects the median nerve in the wrist. It can cause numbness, tingling, and pain in the hand and arm.
Diagnosing carpal tunnel syndrome requires a few steps. These include physical exams, looking at your medical history, and using tests. Electromyography (EMG) and nerve conduction studies (NCS) are often used. But, Magnetic Resonance Imaging (MRI) is also used to check the median nerve and the area around it.
Key Takeaways
- Carpal tunnel syndrome affects nearly 3% of adults in the US.
- Diagnosis involves physical exams, medical history, and diagnostic tests.
- MRI is being used to assess the median nerve and surrounding structures.
- Understanding the diagnostic process can help in seeking appropriate treatment.
- Early diagnosis is crucial for effective management of the condition.
Understanding Carpal Tunnel Syndrome

Let’s explore what carpal tunnel syndrome is all about. It happens when the median nerve gets squeezed in the wrist. This nerve controls the feeling in the palm side of the thumb, index, middle fingers, and part of the ring finger. It also helps move the thumb.
Obtaining an accurate diagnosis is essential for effectively treating Carpal Tunnel Syndrome.
Carpal tunnel syndrome is a condition where the median nerve gets compressed. This can cause numbness, tingling, and weakness in the hand. Swelling, inflammation, or wrist issues can cause this compression.
Common Symptoms and Risk Factors
Symptoms of carpal tunnel syndrome vary but often include numbness or tingling in certain fingers. These feelings can happen at any time, even when you’re sleeping. You might also feel weakness or clumsiness in your hand, or pain in your fingers or wrist.
Things that can increase your risk of getting CTS include doing the same motion over and over, being exposed to vibrations, having certain health conditions like diabetes, and having certain wrist shapes.
Impact on Daily Life
Carpal tunnel syndrome can really affect your daily activities. Even simple tasks like typing or holding things can be hard because of the pain or numbness. If it’s not treated, it can even cause permanent nerve damage.
The Importance of Accurate Diagnosis

Obtaining an accurate diagnosis is essential for effectively treating Carpal Tunnel Syndrome. When we diagnose CTS right, we can tailor the treatment to fit the person’s needs. This improves results and lowers the chance of problems.
Why Proper Diagnosis Matters
A correct diagnosis is important because it lets doctors tell CTS apart from other conditions with similar symptoms. This is crucial for picking the right treatment. Accurate diagnosis means patients get the best care for their specific problem, whether it’s non-surgical or surgery.
Also, a correct diagnosis helps find any underlying conditions that might be causing CTS, like diabetes or rheumatoid arthritis. By treating these conditions, we can better manage CTS symptoms.
Consequences of Misdiagnosis
Misdiagnosis can lead to the wrong treatment, more suffering, and higher healthcare costs. If CTS is mistaken for another condition, or vice versa, the patient might get treatments that don’t fix the problem. This can cause ongoing pain and discomfort, hurting the patient’s quality of life.
| Condition | Similar Symptoms to CTS | Consequences of Misdiagnosis |
| Cervical Radiculopathy | Neck pain, arm numbness | Unnecessary neck surgery, continued CTS symptoms |
| Ulnar Nerve Entrapment | Hand numbness, weakness | Inappropriate treatment, persistent symptoms |
| Thoracic Outlet Syndrome | Arm numbness, pain | Delayed CTS treatment, potential surgical complications |
The Diagnostic Journey
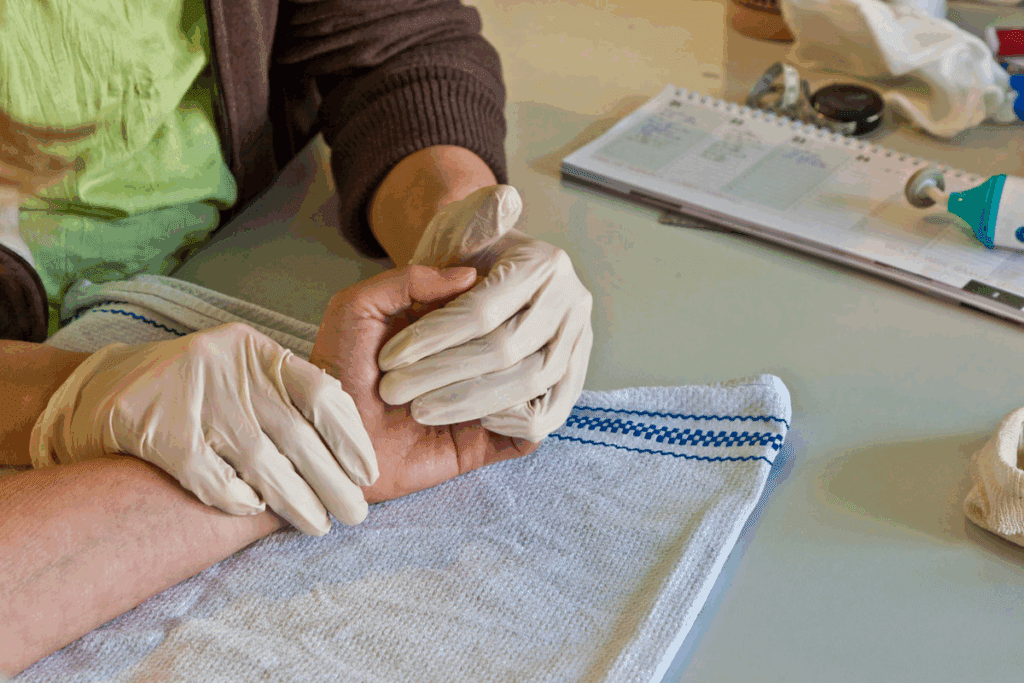
The journey to diagnose CTS starts with a detailed medical history and physical check-up. Doctors might use tests like Tinel’s Sign and Phalen’s Maneuver to check the median nerve. In some cases, tests like nerve conduction studies (NCS) and electromyography (EMG) are needed to confirm the diagnosis.
Advanced imaging like MRI or ultrasound can also be used. These help see the median nerve and the area around it. They can spot any abnormalities or signs of nerve compression.
Understanding the need for accurate diagnosis and the risks of misdiagnosis helps us better navigate the diagnostic journey for CTS. This knowledge helps patients and doctors work together for effective treatment, improving outcomes.
Clinical Examination for Carpal Tunnel Syndrome
Obtaining an accurate diagnosis is essential for effectively treating Carpal Tunnel Syndrome.
Physical Assessment Techniques
CTS diagnosis involves several physical tests. These tests check the median nerve’s function and sensitivity. They help spot signs of nerve compression.
The first step is a detailed medical history and symptom review. Then, the hand, wrist, and arm are examined. The goal is to find muscle weakness, atrophy, or sensory changes.
Tinel’s Sign Test
Tinel’s sign is a common test. It involves tapping lightly on the median nerve at the wrist. If this action makes symptoms worse, it’s a positive sign of nerve irritation.
Phalen’s Maneuver
Phalen’s maneuver is another key test. It involves bending the wrist as far as possible and holding it for 30-60 seconds. If symptoms worsen, it’s a sign of CTS.
Durkan’s Compression Test
Durkan’s test is used to diagnose CTS too. It involves pressing directly on the carpal tunnel. Symptoms like numbness or tingling within 30 seconds are a positive sign.
These tests together give healthcare providers the info they need to diagnose CTS. They help figure out how severe it is and what treatment to use.
Carpal Tunnel Syndrome Test Options in Medical Settings
Medical professionals use different tests to diagnose Carpal Tunnel Syndrome (CTS). The choice depends on symptoms, patient history, and clinical findings.
Overview of Diagnostic Approaches
There are many ways to diagnose CTS. First, doctors do a physical exam. They check wrist and hand function and perform specific tests. These help find out if CTS is present and how severe it is.
Common diagnostic approaches include:
- Clinical evaluation
- Nerve conduction studies (NCS)
- Electromyography (EMG)
- Imaging tests such as X-ray, ultrasound, and MRI
When to Pursue Advanced Testing
Advanced tests are used when initial tests are not clear. This is especially true for unusual symptoms or when other conditions are suspected.
Advanced testing is particularly useful in the following scenarios:
- When clinical findings and symptoms do not correlate
- In cases of severe or progressive symptoms
- When planning surgical intervention
The Diagnostic Algorithm
The diagnostic process for CTS starts with a clinical exam. If more proof is needed, more tests are done. The choice of tests depends on the situation and suspected causes.
A typical diagnostic pathway may involve:
- Initial clinical assessment
- Nerve conduction studies (NCS) and electromyography (EMG) for functional assessment
- Imaging tests like ultrasound or MRI for structural evaluation
Knowing the diagnostic algorithm helps doctors choose the right tests. This ensures accurate diagnosis and effective treatment of CTS.
Electrodiagnostic Testing for Carpal Tunnel
Electrodiagnostic testing is key in diagnosing and managing Carpal Tunnel Syndrome. These tests check the median nerve and the muscles it supplies. They give important info for diagnosis and treatment.
Nerve Conduction Studies (NCS)
Nerve Conduction Studies are vital for Carpal Tunnel Syndrome. NCS stimulates the median nerve and measures the electrical response. This test shows how fast and strong the nerve signals are, helping to see how severe the nerve compression is.
The NCS process is simple. Electrodes are placed on the skin over the median nerve. A small electrical impulse is applied, and the nerve’s response is recorded. This gives data on nerve function.
Electromyography (EMG)
Electromyography is another important test for Carpal Tunnel Syndrome. EMG checks the electrical activity of muscles. It helps find muscle damage from nerve compression. A small needle electrode is inserted into the muscle, and the electrical activity is recorded at rest and during muscle contraction.
This test is great for spotting muscle denervation in advanced Carpal Tunnel Syndrome. It helps healthcare providers see how much nerve damage there is and plan treatment.
Interpreting Electrodiagnostic Results
Understanding electrodiagnostic test results needs expertise. The results of NCS and EMG together show how severe Carpal Tunnel Syndrome is. Tests classify it as mild, moderate, or severe based on nerve conduction and muscle denervation.
Getting these tests right is crucial for treatment. Healthcare providers use the results to decide if simple treatments or more serious interventions are needed.
Patient Experience During Testing
Electrodiagnostic testing is usually okay, but some discomfort is possible. NCS might feel a bit uncomfortable because of the electrical impulse. EMG can cause pain when the needle goes into the muscle.
But, these tests are quick, and the discomfort is short-lived. Healthcare providers work to make the experience as comfortable as possible for patients.
X-ray Imaging for Carpal Tunnel Assessment
X-rays are not the first choice for diagnosing carpal tunnel syndrome. Yet, they can help find other reasons for wrist pain. X-rays are great for checking many wrist problems. Let’s look at how they fit into diagnosing carpal tunnel syndrome.
Can X-rays Detect Carpal Tunnel Syndrome?
X-rays can’t see soft tissues like nerves and tendons. So, they’re not the best for directly finding carpal tunnel syndrome. But, they can spot other issues like fractures, arthritis, or bone spurs that might cause similar symptoms.
We use X-rays to check the bones in the wrist. They can show problems like fractures or dislocations that might press on the median nerve.
Special X-ray Views for Wrist Evaluation
To fully see the wrist, we take special X-ray views. These include:
- Posteroanterior (PA) view: Gives a general look at the wrist.
- Lateral view: Shows how the bones line up and if there are fractures or dislocations.
- Oblique views: Give extra views to spot small problems not seen on standard views.
These views help us understand the wrist’s structure and any problems.
Limitations of X-ray in Carpal Tunnel Diagnosis
X-rays can’t see soft tissues, which is a big problem for diagnosing carpal tunnel syndrome. Since the condition affects the median nerve, a soft tissue, X-rays can’t directly find it.
Key limitations of X-ray for CTS diagnosis include:
- Can’t see the median nerve or the soft tissues around it.
- Not good at finding nerve compression or damage.
- Can’t tell how severe carpal tunnel syndrome is.
Even with these limits, X-rays are still useful. They help rule out other wrist pain causes and find factors that might help.
Ultrasound Evaluation of the Carpal Tunnel
Ultrasound imaging is a non-invasive way to see the median nerve in carpal tunnel syndrome. It’s popular because it shows the nerve and its surroundings in real-time.
How Ultrasound Visualizes the Median Nerve
Ultrasound uses sound waves to create detailed images of the median nerve in the carpal tunnel. It helps doctors check the nerve’s size, shape, and how it moves. The median nerve looks like a dark area next to the bright carpal bones and flexor retinaculum.
Advantages of Ultrasound Assessment
- Non-invasive and safe
- Real-time imaging capability
- No radiation exposure
- Can assess nerve mobility
Diagnostic Criteria on Ultrasound
Doctors look for certain signs when using ultrasound to check for carpal tunnel syndrome. These include:
- Cross-sectional area of the median nerve
- Nerve swelling or edema
- Flattening ratio of the median nerve
- Presence of bowing of the flexor retinaculum
Research shows that a median nerve area over 10 mm² at the pisiform bone level means carpal tunnel syndrome.
Dynamic Ultrasound Imaging
Dynamic ultrasound imaging checks the median nerve while you move your wrist. It shows how the nerve moves and if it’s caught or compressed. It helps find out if symptoms get worse in certain wrist positions.
By using both static and dynamic ultrasound, doctors can fully understand the median nerve and its surroundings. This helps them accurately diagnose and treat carpal tunnel syndrome.
MRI Imaging for Carpal Tunnel Syndrome
Magnetic Resonance Imaging (MRI) is key for diagnosing Carpal Tunnel Syndrome (CTS). It helps us see the median nerve and the area around it. This lets us understand why the nerve might be compressed.
How MRI Works for Nerve Visualization
MRI uses strong magnetic fields and radio waves to show soft tissues like nerves. For CTS, it shows the median nerve’s shape and how it’s pressed. This method is great for seeing how much the nerve is compressed and finding other signs of CTS.
MRI Protocols for Carpal Tunnel Assessment
Special MRI plans are made to see the median nerve and nearby tissues well. These plans use T1 and T2 images to show nerve details and problems. Our radiologists pick the best images to check the carpal tunnel fully.
| MRI Sequence | Primary Use in CTS Assessment |
| T1-weighted | Anatomical detail, nerve visualization |
| T2-weighted | Detection of edema, nerve compression |
What Radiologists Look For
Radiologists look for signs of nerve compression in MRI scans for CTS. They check for swelling or nerve flattening. They also look for increased signal intensity on T2 images.
“MRI has become an indispensable tool in our diagnostic arsenal, allowing us to non-invasively assess the median nerve and guide treatment decisions,” says a leading radiologist.
Advanced MRI Techniques
Advanced MRI methods like diffusion tensor imaging (DTI) and MR neurography are used more. They give detailed info on nerve structure and help measure CTS severity. We’re always looking to use these advanced methods to improve diagnosis and treatment.
Can You Actually See Carpal Tunnel Syndrome on MRI?
We look into how MRI helps see Carpal Tunnel Syndrome, a common issue affecting millions. MRI is key in spotting many muscle and bone problems, including Carpal Tunnel Syndrome.
What MRI Can and Cannot Show
MRI is great at showing soft tissues like nerves, tendons, and ligaments. For Carpal Tunnel Syndrome, MRI can spot changes in the median nerve and nearby tissues. But, it’s important to know MRI isn’t always needed to diagnose Carpal Tunnel Syndrome. It’s mainly used to check for other causes of wrist pain or to see how severe the nerve compression is.
Median Nerve Appearance on MRI
On MRI, the median nerve looks like a clear structure in the carpal tunnel. If someone has Carpal Tunnel Syndrome, the nerve might look flattened or swollen. It might also look brighter on T2-weighted images because of swelling or inflammation. These signs can show how bad the condition is.
Key features of median nerve appearance on MRI include:
- Flattening of the median nerve at the level of the hamate
- Swelling of the median nerve proximal to the carpal tunnel
- Hyperintensity on T2-weighted images
Detecting Secondary Signs of Compression
MRI can also spot other signs of compression besides the median nerve. For example, it can show if the thenar muscles are affected on T2-weighted images. This can tell us more about how long the condition has been there and how severe it is.
MRI Findings in Different Stages of Carpal Tunnel Syndrome
MRI findings change as Carpal Tunnel Syndrome progresses. In the early stages, the median nerve might not show much. But in later stages, there can be clear nerve damage and muscle problems. Knowing these differences helps doctors diagnose and plan treatment correctly.
MRI’s ability to show detailed images of the median nerve and surrounding areas makes it a valuable tool for diagnosing and assessing Carpal Tunnel Syndrome.
When is an MRI Necessary for Carpal Tunnel Syndrome?
Obtaining an accurate diagnosis is essential for effectively treating Carpal Tunnel Syndrome.
Clinical Scenarios Requiring MRI
There are times when MRI is crucial for diagnosing and treating carpal tunnel syndrome. These include:
- Atypical presentations: When symptoms are unusual or don’t respond to usual treatments, MRI can find the cause.
- Severe symptoms: For those with serious or worsening nerve damage, MRI shows how bad it is.
- Suspected concomitant conditions: MRI can spot other issues that might be causing or looking like carpal tunnel syndrome, like tumors or cysts.
When Clinical Exams Are Sufficient
Often, a detailed clinical exam can diagnose carpal tunnel syndrome. This includes a medical history, physical check-up, and tests like Tinel’s sign and Phalen’s maneuver. MRI is used when the diagnosis is not clear or more info is needed for treatment.
MRI for Atypical Presentations
When carpal tunnel syndrome shows up differently, it’s hard to diagnose. MRI is great here because it shows the median nerve and nearby areas in detail. It helps find any issues that might be causing symptoms.
Pre-surgical Planning
Before surgery for carpal tunnel syndrome, MRI is very important. It helps surgeons see the nerve and any possible problems. This lets them plan a more accurate and effective surgery.
| Clinical Scenario | Role of MRI |
| Atypical presentations | Identify underlying causes of unusual symptoms |
| Severe or progressive symptoms | Assess extent of nerve damage |
| Pre-surgical planning | Provide detailed anatomy for surgical planning |
Comparing Diagnostic Imaging Techniques
Several imaging techniques are used to diagnose Carpal Tunnel Syndrome. Each has its own strengths and weaknesses. The choice depends on the patient’s condition, technology availability, and cost.
MRI vs. Ultrasound
MRI and ultrasound are both useful for diagnosing Carpal Tunnel Syndrome. MRI shows detailed images of the median nerve and surrounding structures. This helps detect nerve compression and other issues. Ultrasound, on the other hand, allows clinicians to see the median nerve moving.
Choosing between MRI and ultrasound depends on the situation. MRI is best for finding masses or severe nerve damage. Ultrasound is often chosen for its real-time images and lower cost.
MRI vs. X-ray
X-rays are mainly used for bone structures, not nerve compression. However, X-rays can help rule out fractures or arthritis. MRI is better for diagnosing CTS because it shows soft tissues.
MRI gives a detailed look at the carpal tunnel and its contents. While X-rays are good for bones, MRI is better for soft tissues like nerves.
Cost-Benefit Analysis of Different Imaging Methods
The cost of imaging varies a lot. X-rays are the cheapest, while MRI is more expensive. Ultrasound is in the middle, needing more skill but costing less than MRI.
When looking at costs, it’s important to consider how accurate the diagnosis is. MRI’s detailed images might be worth the extra cost for complex cases.
Emerging Imaging Technologies
New imaging technologies are coming out, like DTI and MRN. These techniques show nerves better, helping diagnose Carpal Tunnel Syndrome more accurately.
As these technologies spread, they could lead to better treatments for CTS. This could mean more tailored care for patients.
At-Home Carpal Tunnel Tests
Obtaining an accurate diagnosis is essential for effectively treating Carpal Tunnel Syndrome.
Limitations of Home Testing
Tests like Tinel’s sign self-assessment or Phalen’s maneuver can give you a hint. But, they’re not perfect. They can give wrong results.
Home tests have big limits. They can’t tell you for sure if you have CTS. A study showed that just feeling symptoms isn’t enough to know for sure.
The main problems with home tests are:
- They need a pro to understand them
- They can’t show how bad the nerve damage is
- It’s easy to do them wrong
When to Seek Professional Evaluation
If you keep feeling weird symptoms or if home tests suggest CTS, see a doctor. They can do detailed tests to really know what’s going on.
You should see a doctor if you notice:
- Constant numbness or tingling in your hand or fingers
- Weakness in your hand or wrist
- Pain that keeps you awake or stops you from doing things
Digital Health Tools for Monitoring
Mobile apps and wearables are great for keeping an eye on CTS symptoms. They can track how bad your symptoms are and even suggest exercises to help.
These tools have some good points:
- They watch your symptoms all the time
- They offer exercises just for you
- They help your doctor understand your situation better
Even though they can’t diagnose, they’re useful. They give your doctor more information to make better decisions.
How Doctors Determine the Right Carpal Tunnel Syndrome Test
Figuring out if someone has CTS needs careful thought. We look at many things to pick the best test for each patient.
Factors Influencing Test Selection
Choosing the right test for CTS isn’t simple. We consider how bad the symptoms are, the patient’s health history, and what insurance covers.
- Symptom Severity: People with mild symptoms might need different tests than those with severe ones.
- Medical History: What health issues a patient has can guide us to the right tests.
- Insurance Coverage: What tests are available can depend on the patient’s insurance.
Severity-Based Testing Approach
The severity of symptoms is key in picking the right test. For mild CTS, we might start with simple exams. But for severe cases, we might use MRI or other advanced tests.
| Symptom Severity | Typical Diagnostic Approach |
| Mild | Clinical examination, possibly followed by nerve conduction studies |
| Moderate | Nerve conduction studies, possibly with ultrasound |
| Severe | Advanced imaging like MRI, possibly with electromyography |
Insurance and Cost Considerations
Insurance and cost are big factors in choosing tests. We help patients understand their insurance and find affordable options without sacrificing accuracy.
Personalized Diagnostic Pathways
We focus on personalized care, including in diagnosis. We tailor tests to each patient’s needs and situation.
This approach ensures patients get the right tests. It leads to accurate diagnoses and effective treatments.
Interpreting Your Carpal Tunnel Test Results
Carpal tunnel test results give you important insights into your health. They help decide the best treatment for you. Knowing what these results mean is key to managing your carpal tunnel syndrome.
Understanding Diagnostic Reports
Diagnostic reports for carpal tunnel syndrome come from tests like nerve conduction studies (NCS) or electromyography (EMG). These reports show any problems with nerve function or muscle activity.
Nerve conduction studies check how fast electrical signals move through a nerve. For carpal tunnel syndrome, they see if the median nerve is slowed down as it goes through the carpal tunnel.
“The diagnostic report will typically include measurements of nerve conduction velocity, amplitude, and latency, which are critical for assessing the severity of nerve compression.”
Grading Systems for Carpal Tunnel Severity
There are grading systems to show how severe carpal tunnel syndrome is. These systems use test results to classify it as mild, moderate, or severe. They look at nerve conduction velocity and EMG findings.
- Mild: Symptoms are intermittent, and nerve conduction studies may show slight abnormalities.
- Moderate: Symptoms are more persistent, with moderate nerve conduction abnormalities.
- Severe: Symptoms are constant, with significant nerve damage indicated by pronounced abnormalities on NCS and EMG.
What Negative Test Results Mean
Negative test results for carpal tunnel syndrome don’t always mean you’re clear. It could be that the tests were too early, or your symptoms aren’t severe enough. Sometimes, more tests or trying treatments first are suggested.
It’s essential to discuss your results with your healthcare provider to understand what they mean for your symptoms and health.
Discussing Results With Your Healthcare Provider
When talking about your carpal tunnel test results with your healthcare provider, cover a few important points:
- What the test results say about your carpal tunnel syndrome.
- How the results affect your treatment plan.
- If more tests or evaluations are needed.
- Treatment options, like non-surgical methods, injections, or surgery, based on your condition’s severity.
By understanding your test results and working with your healthcare provider, you can make a plan to manage your carpal tunnel syndrome. This will help improve your quality of life.
Treatment Options Based on Diagnostic Findings
Understanding the severity of Carpal Tunnel Syndrome is crucial. It helps choose the right treatment. Treatments range from simple steps to surgery, based on how severe it is.
Conservative Treatments for Mild Cases
For mild Carpal Tunnel Syndrome, simple treatments work first. These include:
- Wrist splinting to keep the wrist straight and reduce pressure on the median nerve
- Physical therapy to improve wrist and hand mobility
- Activity modification to avoid exacerbating the condition
- Nonsteroidal anti-inflammatory drugs (NSAIDs) to reduce pain and inflammation
These steps can manage symptoms well and stop it from getting worse.
Interventional Approaches for Moderate Cases
For moderate cases, more steps are needed. These include:
- Corticosteroid injections to reduce swelling and relieve pressure on the median nerve
- Platelet-rich plasma (PRP) therapy to promote healing
These methods help when simple treatments don’t work.
Surgical Options for Severe Cases
Severe cases or when other treatments fail, surgery is needed. Surgery cuts the ligament to free the median nerve.
There are different surgical techniques, including:
- Open release surgery
- Endoscopic surgery
The right surgery depends on the patient’s health and the doctor’s advice.
Recovery Expectations Based on Diagnosis
Recovery time varies with the severity and treatment. Generally, patients can expect:
| Treatment Approach | Recovery Time | Expected Outcome |
| Conservative Treatments | Several weeks to months | Significant improvement in symptoms |
| Interventional Approaches | Variable, often quicker than surgery | Relief from pain and improved function |
| Surgical Options | Several months | Permanent relief for most patients |
Following your doctor’s post-treatment care is key for the best results.
Conclusion
Obtaining an accurate diagnosis is essential for effectively treating Carpal Tunnel Syndrome.pal Tunnel Syndrome (CTS) well. We’ve looked at different ways to diagnose it, like clinical exams, tests, and imaging like X-rays and MRI.
Knowing how to use these tools helps doctors create treatment plans that fit each patient. This includes both non-surgical and surgical options. We’ve highlighted the importance of a personalized approach to care.
Managing CTS well can make a big difference in a person’s life. It shows that the right diagnosis and treatment are essential for the best results for those with CTS.
FAQ
Obtaining an accurate diagnosis is essential for effectively treating Carpal Tunnel Syndrome.
Carpal tunnel syndrome happens when the median nerve gets compressed in the wrist. This can cause numbness, tingling, and other symptoms in the hand.
How is carpal tunnel syndrome diagnosed?
Doctors use a mix of clinical checks, patient history, and tests like nerve conduction studies (NCS) and electromyography (EMG). They also use ultrasound and MRI.
Can you see carpal tunnel syndrome on MRI?
MRI can show the median nerve and other wrist structures. It helps spot nerve compression and other signs of carpal tunnel syndrome. But, it doesn’t directly show the condition.
What does an MRI show in carpal tunnel syndrome?
An MRI might show swelling or flattening of the median nerve. It can also reveal increased signal intensity within the nerve. These signs suggest compression or damage.
When is an MRI necessary for diagnosing carpal tunnel syndrome?
An MRI is usually needed for atypical symptoms or when other conditions need to be ruled out. It’s also used when planning surgery.
How does electrodiagnostic testing work for carpal tunnel syndrome?
Tests like NCS and EMG check the median nerve’s electrical activity. They help find out how severe the nerve damage is.
What is the role of ultrasound in diagnosing carpal tunnel syndrome?
Ultrasound can show the median nerve’s movement and any compression. It provides important information for diagnosing carpal tunnel syndrome.
Can at-home tests diagnose carpal tunnel syndrome?
At-home tests can suggest issues but aren’t definitive. Always get a professional evaluation for a sure diagnosis.
How do doctors decide on the right diagnostic tests for carpal tunnel syndrome?
Doctors choose tests based on symptoms, patient history, and clinical findings. They also consider insurance and cost. The goal is a personalized diagnostic plan.
What are the treatment options for carpal tunnel syndrome based on diagnostic findings?
Treatment varies. Mild cases might get wrist splints and physical therapy. Moderate cases might get corticosteroid injections. Severe cases might need surgery.
How do I interpret my carpal tunnel test results?
Understanding your results means knowing about nerve function and damage. Talk to your healthcare provider to figure out what to do next.
Can X-rays detect carpal tunnel syndrome?
X-rays aren’t used to directly diagnose carpal tunnel syndrome. But, they can help rule out other wrist pain causes like fractures or arthritis.
References
- Padua, L., Coraci, D., Erra, C., Pazzaglia, C., Paolasso, I., Loreti, C., Rossini, P. M., & Hobson-Webb, L. D. (2016). Carpal tunnel syndrome: Clinical and electrophysiological diagnostic criteria. Clinical Neurophysiology, 127(6), 2548–2555. https://pubmed.ncbi.nlm.nih.gov/27040851/





