Last Updated on November 4, 2025 by mcelik
Osteoarthritis affects millions of people worldwide, causing significant pain and disability. A recent study revealed that individuals with osteoarthritis are at a higher risk of mortality due to related comorbidities.
The condition is often linked to a reduced life expectancy. This is mainly because it limits physical activity and increases the risk of other serious health issues. Understanding the osteoarthritis life expectancy and the factors influencing it is key to managing the condition effectively.
Research indicates that the arthritis mortality rate is significant. This highlights the need for thorough care and management strategies for individuals with osteoarthritis.
Key Takeaways
- Osteoarthritis can significantly impact life expectancy.
- The condition increases the risk of mortality due to related comorbidities.
- Understanding osteoarthritis life expectancy is key for effective management.
- Rheumatoid arthritis life expectancy is also affected by the severity of the condition.
- Comprehensive care strategies are necessary to manage osteoarthritis effectively.
Understanding Osteoarthritis: The Degenerative Joint Disease
Osteoarthritis, also known as degenerative joint disease, is when cartilage and bone in joints wear down. This leads to bone rubbing against bone, causing pain and stiffness.
Definition and Prevalence of Osteoarthritis
Osteoarthritis is a disease that damages cartilage and bones in joints. It’s a major cause of disability, affecting millions globally.
It gets more common with age, hitting many over 65. Being overweight, having a family history, or past injuries can also raise your risk.
Key statistics on osteoarthritis prevalence:
- Over 32.5 million adults in the United States have osteoarthritis.
- It’s more common in women than men.
- It grows more common with age, hitting hard after 45.
How Osteoarthritis Differs from Other Types of Arthritis
Osteoarthritis is different from other arthritis types. Unlike rheumatoid arthritis, which is an autoimmune disease, osteoarthritis comes from wear and tear.
The main differences include:
- Degenerative vs. Inflammatory: Osteoarthritis is degenerative, while conditions like rheumatoid arthritis are inflammatory.
- Cause: Osteoarthritis is mainly due to aging and wear, whereas other forms may be due to autoimmune responses or infections.
- Symptoms: While joint pain is common, osteoarthritis tends to cause more localized pain compared to systemic conditions like rheumatoid arthritis.
Can Arthritis Kill You? Examining the Mortality Risk
Whether arthritis can be fatal depends on several factors, including other health conditions. Both osteoarthritis (OA) and rheumatoid arthritis (RA) can impact a person’s health and life expectancy.
Direct vs. Indirect Effects on Mortality
Arthritis can harm you directly or indirectly. Direct harm might come from severe joint damage or surgery complications. Indirect harm is more common and affects other body systems and overall health.
Rheumatoid arthritis, for example, raises the risk of heart disease, leading to higher death rates. Osteoarthritis causes chronic pain and mobility issues, which can also lower life expectancy.
Arthritis Mortality Statistics in the United States
Arthritis mortality statistics show its impact on public health. The Centers for Disease Control and Prevention (CDC) reports that arthritis and related conditions are major contributors to deaths in the U.S.
| Year | Arthritis-Related Mortality Rate (per 100,000) | Total Arthritis-Related Deaths |
| 2015 | 2.4 | 7,400 |
| 2016 | 2.5 | 7,700 |
| 2017 | 2.6 | 8,100 |
The table shows the trend in arthritis-related deaths in the U.S. over three years. It emphasizes the need to manage arthritis well to reduce mortality.
Studies indicate that arthritis can increase mortality risk, mainly when combined with other health issues. It’s vital to understand and manage the relationship between arthritis and other health problems to improve patient outcomes.
Life Expectancy with Osteoarthritis: What Research Shows
Research on osteoarthritis has given us important insights. It shows how this disease affects life expectancy. Osteoarthritis (OA) is more than just a joint problem. It impacts overall health and can even affect how long we live.
Statistical Data on Osteoarthritis and Longevity
Studies have found that OA can shorten life expectancy. People with OA face a higher risk of death, mainly due to other health issues.
A study in a well-known medical journal found a link between OA and higher death rates. This is because OA causes chronic inflammation, which can harm the body.
Factors That Influence Life Expectancy in OA Patients
Several things can affect how long OA patients live. These include how severe the OA is, other health problems, lifestyle choices, and how well OA is managed.
- Severity of OA: More severe OA means a worse outlook.
- Comorbid Conditions: Other health issues can make OA harder to manage and shorten life.
- Lifestyle Factors: Smoking, not being active, and being overweight can worsen OA and shorten life.
- Management Strategies: Good OA management can improve life quality and might even extend life.
It’s key for doctors to understand these factors. This helps them create better care plans. Plans that tackle OA symptoms and its wider health effects.
Osteoarthritis vs. Rheumatoid Arthritis: Mortality Comparison
Osteoarthritis and rheumatoid arthritis are more than just health issues. They also affect how long we live. Each condition has its own way of impacting patients.
Why Rheumatoid Arthritis Has Higher Mortality Risks
Rheumatoid arthritis (RA) is more dangerous than osteoarthritis (OA) when it comes to death. Several reasons explain this:
- Systemic Inflammation: RA causes inflammation all over the body. This can lead to heart disease, a big killer.
- Comorbid Conditions: People with RA often have other health problems like diabetes and high blood pressure. These add to the risk of dying.
- Immune System Dysfunction: RA messes with the immune system. This makes people more likely to get sick and face other serious problems.
When Osteoarthritis Coexists with Rheumatoid Arthritis
Sometimes, people have both osteoarthritis and rheumatoid arthritis. This makes things harder for their health:
- Having both conditions makes symptoms worse. It makes it harder to manage the health.
- There’s a higher chance of damage to joints and losing the ability to move.
- Doctors need to create detailed plans to treat both conditions well.
It’s important to know the differences and how they can overlap. This helps doctors take better care of patients and improve their health.
The Natural Progression of Osteoarthritis
Knowing how osteoarthritis (OA) progresses is vital for managing its symptoms. OA is a degenerative joint disease. It causes cartilage breakdown, leading to bone-on-bone contact and pain.
Osteoarthritis goes through several stages, each with its own challenges. It’s important to recognize these stages to create effective treatment plans.
Early, Middle, and Late Stages of OA
Osteoarthritis moves from early to late stages, with each stage getting worse.
- Early Stage: Minor cartilage loss and slight joint space narrowing occur. Symptoms may be mild, with occasional pain.
- Middle Stage: Cartilage loss speeds up, and joint space narrowing gets more noticeable. Pain and stiffness grow, worse after rest.
- Late Stage: Big cartilage loss and bone-on-bone contact cause severe pain, swelling, and less mobility.
Timeline of Disease Progression
The timeline of OA progression varies a lot among people. It depends on age, lifestyle, and other health conditions.
| Stage | Characteristics | Typical Duration |
| Early | Minor cartilage loss, occasional pain | 2-5 years |
| Middle | Accelerated cartilage loss, increased pain and stiffness | 3-7 years |
| Late | Significant cartilage loss, severe pain and reduced mobility | Varies, often irreversible |
When Does Osteoarthritis Typically Start?
Osteoarthritis can start at any age but gets more common after 45. Genetics, obesity, and past joint injuries can make it start sooner.
“Osteoarthritis is a leading cause of disability among older adults, stressing the need for early detection and management.”
— Arthritis Foundation
Understanding OA’s progression is key to managing its effects. By knowing the stages and factors that speed it up, healthcare providers can make better treatment plans. This helps improve patient outcomes.
Complications of Untreated Osteoarthritis
Not treating osteoarthritis can lead to serious problems. It affects your physical health, mental well-being, and overall health. Untreated osteoarthritis can cause many issues that lower your quality of life.
Physical Complications
Untreated osteoarthritis can cause several physical problems, including:
- Increased pain and stiffness in the affected joints
- Reduced mobility and flexibility
- Loss of function and disability
- Development of bone spurs and cysts
As osteoarthritis gets worse, the pain and stiffness can become very bad. Reduced mobility makes daily tasks hard. It also leads to other health problems like obesity and heart disease.
Mental Health Impact
Untreated osteoarthritis can deeply affect your mental health. Many people feel:
- Depression
- Anxiety
- Reduced self-esteem
Chronic pain can make you feel frustrated and hopeless. It’s key to get care that helps both your physical and mental health.
“The psychological burden of chronic osteoarthritis should not be underestimated. It is vital to manage the disease effectively to lessen its impact on mental health.”
Systemic Health Effects
Osteoarthritis is more than just a joint problem. It can affect your whole body, if not treated. Studies show that osteoarthritis raises the risk of:
- Cardiovascular disease
- Diabetes
- Obesity
The inflammation and metabolic changes from osteoarthritis can lead to these systemic health issues. This shows why managing osteoarthritis is important for your overall health.
How Osteoarthritis Affects Different Body Parts
It’s important to know how osteoarthritis impacts different parts of the body. This knowledge helps in managing the condition better and improving life quality. Osteoarthritis is a disease that wears down joints, causing pain, stiffness, and less mobility.
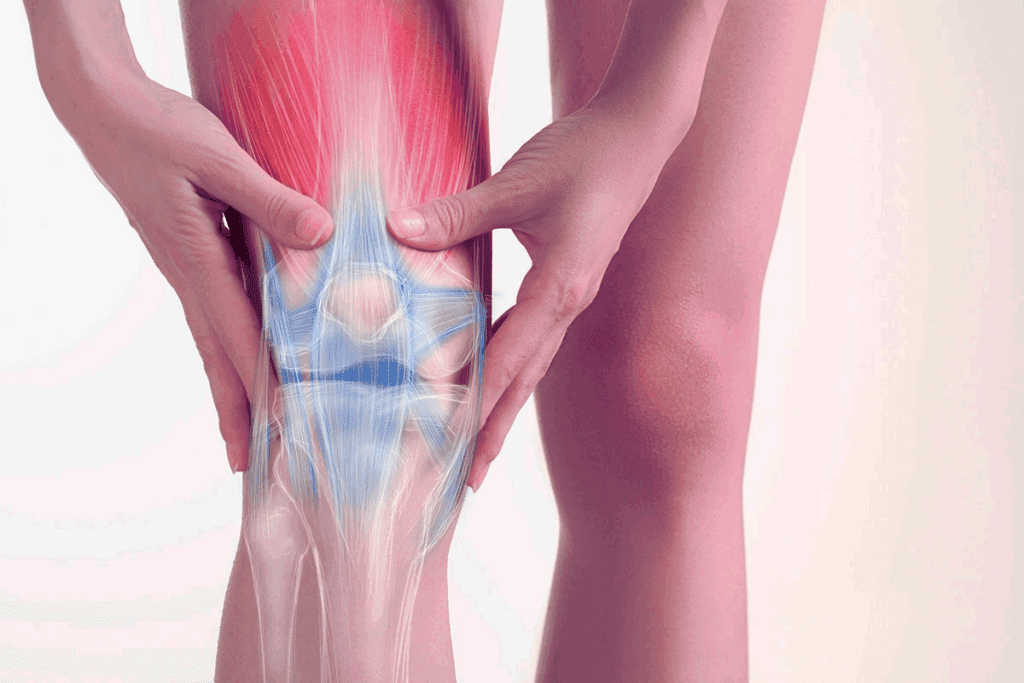
Osteoarthritis of the Knee Joint
Knee osteoarthritis is very common. It happens when the cartilage in the knee wears out. This makes bones rub together, causing pain, swelling, and stiffness. It makes everyday tasks hard to do.
Symptoms of knee osteoarthritis include:
- Pain during movement
- Stiffness after periods of rest
- Swelling and redness around the knee
- Grinding sensation when moving the knee
Osteoarthritis of the Spine and Back
Osteoarthritis in the spine can cause a lot of back pain and stiffness. It affects the facet joints in the spine, leading to cartilage breakdown and bone spurs.
The symptoms can vary based on where and how severe the osteoarthritis is. Common symptoms include:
- Back pain that worsens with activity
- Stiffness in the morning or after rest
- Radiating pain to the arms or legs
Hand, Foot, and Ankle Osteoarthritis
Osteoarthritis can also affect the hands, feet, and ankles, leading to pain and reduced dexterity. In the hands, it often causes Heberden’s nodes, which are bony enlargements of the distal interphalangeal joints.
Symptoms in the hands, feet, and ankles include:
- Pain and stiffness in the affected joints
- Swelling and deformity
- Reduced range of motion
Here is a summary of how osteoarthritis affects different body parts:
| Body Part | Common Symptoms |
| Knee | Pain during movement, stiffness, swelling |
| Spine and Back | Back pain, stiffness, radiating pain |
| Hands, Feet, and Ankles | Pain, stiffness, swelling, deformity |
Risk Factors That May Worsen Prognosis
Knowing what makes osteoarthritis worse is key to managing it well. Many things can affect how the disease progresses. This can really change someone’s life quality.
Age-Related Factors and Aging
Age is a big risk factor for osteoarthritis. The more you age, the more likely you are to get it. Aging joints wear out faster, and cartilage can’t heal as well.
As people get older, the chance of getting osteoarthritis in joints like knees and hips goes up.
Lifestyle and Environmental Factors
Lifestyle and environment also matter a lot. For example, obesity puts more stress on joints. Other factors include past injuries, genes, and jobs or activities that strain joints.
- Obesity: Excess weight puts additional stress on joints.
- Previous joint injuries: Trauma to a joint can increase the risk of developing osteoarthritis.
- Genetic predisposition: Some people are more likely to develop osteoarthritis due to genetic factors.
Comorbid Conditions
Having other health issues can make osteoarthritis harder to manage. Conditions like diabetes, heart disease, and other rheumatic diseases can affect overall health. This makes it tough to handle osteoarthritis well.
Healthcare providers can make better treatment plans if they know these risk factors. This could help improve the outlook for people with osteoarthritis.
Diagnosing Osteoarthritis: From Symptoms to X-rays
Doctors diagnose osteoarthritis by looking at symptoms, doing physical exams, and using X-rays. This method ensures they get it right and can plan the best treatment.
Clinical Symptoms and Physical Examination
The first step in diagnosing osteoarthritis is a detailed check-up. People often say they have pain and stiffness in their joints. This gets worse when they move and feels better when they rest.
They might also notice:
- Joint pain and tenderness
- Stiffness, which gets better with rest
- Limited range of motion
- Crepitus or a grating sensation in the joint
- Bony enlargements or deformities
A physical exam is key to seeing how much damage there is and how much movement is lost. Doctors look for swelling, warmth, or any changes in the joint.
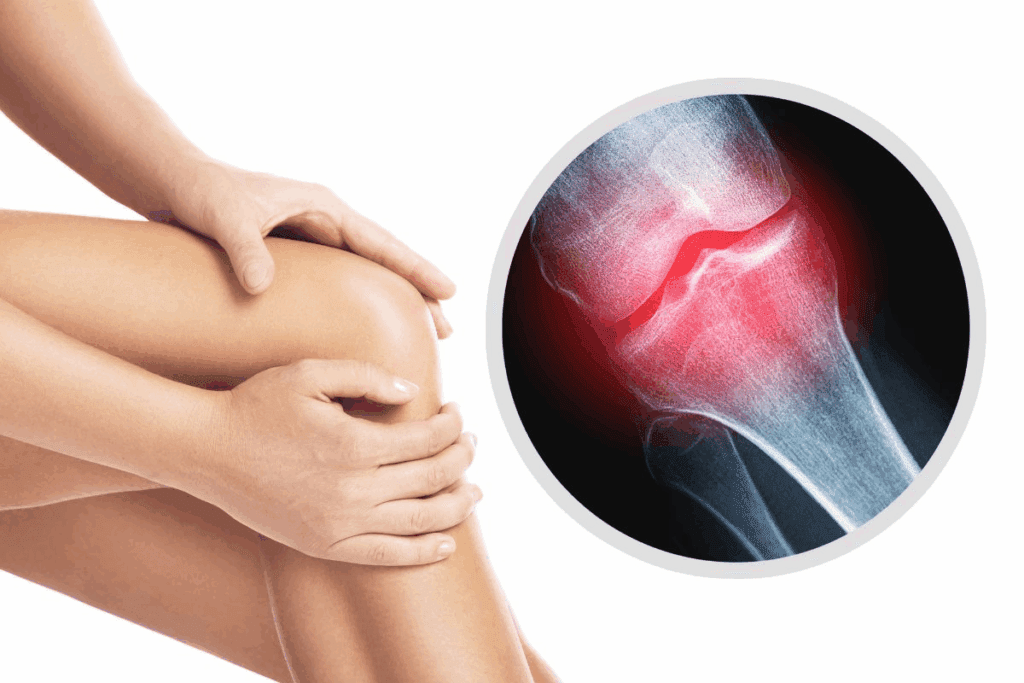
Radiological Findings in Osteoarthritis
X-rays are very important in confirming osteoarthritis. They show signs like:
- Joint space narrowing
- Osteophyte formation
- Subchondral sclerosis
- Cysts within the bone
These signs help doctors understand how severe the disease is and what treatment to use.
Differential Diagnosis
Other arthritis types and joint problems can look like osteoarthritis. So, doctors need to rule out other possibilities. These include:
- Rheumatoid arthritis
- Gout
- Pseudogout
- Traumatic arthritis
By looking at the patient’s history, doing a physical exam, and running tests, doctors can tell osteoarthritis apart from other conditions.
Treatment Options and Their Impact on Longevity
Managing osteoarthritis well means using a mix of treatments. This can really help improve life quality and how long you live. The right treatment depends on how bad the condition is, your overall health, and what you prefer.
Conservative Management Approaches
Usually, the first step in treating osteoarthritis is conservative management. This method aims to ease symptoms and boost function without surgery. It includes:
- Physical Therapy: Exercises to help move joints better and make muscles stronger.
- Pain Management: Using drugs like NSAIDs or acetaminophen to control pain.
- Lifestyle Modifications: Making diet, exercise, and weight changes to lessen joint stress.
- Assistive Devices: Using canes, walkers, or orthotics to ease joint pressure.
These methods can greatly improve life for OA patients and might slow the disease’s progress.
Surgical Interventions
If conservative methods don’t work, surgery might be an option. Surgical treatments for OA include:
- Joint Replacement Surgery: Swapping the damaged joint with an artificial one.
- Osteotomy: Cutting and rearranging bones to better align the joint and reduce pain.
- Arthroscopy: A small surgery to remove damaged cartilage or bone pieces.
Surgery can bring a lot of relief from pain and improve function for many people.
Current Treatment Guidelines for OA
Today’s guidelines suggest a multi-faceted approach to OA care. They focus on educating patients, exercising, managing weight, and using medicine when needed. The American College of Rheumatology (ACR) and the Arthritis Foundation (AF) have set guidelines. They recommend:
| Treatment Aspect | Recommendation |
| Exercise | Regular aerobic and resistance exercises |
| Weight Management | Maintaining a healthy weight to reduce joint stress |
| Pain Management | Using oral NSAIDs or topical agents as first-line treatments |
| Surgical Options | Considering surgery when conservative measures fail |
By following these guidelines, doctors can give care that really helps OA patients.
Pain Management Strategies for Osteoarthritis
Managing pain from osteoarthritis is key to feeling better and moving easier. It’s important to use both medicine and non-medicine ways to help. Each person’s needs are different, so a custom plan is best.
Pharmacological Approaches
Medicine is often the first step in treating osteoarthritis pain. Acetaminophen is often the first choice because it helps with pain. Nonsteroidal anti-inflammatory drugs (NSAIDs) also work well but can have side effects, mainly for older adults.
For more severe pain, doctors might suggest stronger drugs like opioids. But, these are used carefully because of the risk of addiction. Corticosteroid injections can also help by reducing swelling in the joint.
Non-Pharmacological Pain Relief
There are many ways to manage osteoarthritis pain without medicine. Physical therapy can make joints move better and muscles stronger. Exercise programs like swimming or cycling are good for keeping joints working without too much stress.
Weight management is also important because extra weight can make symptoms worse. Using assistive devices like canes can also help by easing the load on joints.
When to Seek Emergency Care for Arthritis Pain
Most osteoarthritis pain can be managed without going to the emergency room. But, there are times when you should go right away. If pain comes on suddenly and is very bad, or if you see swelling, redness, or warmth, get help fast. Also, if you can’t move as well as usual or if pain is with other symptoms, go to the emergency room.
Disability and Quality of Life Considerations
Osteoarthritis affects more than just the joints. It can change how well you live and what you can do every day. As it gets worse, people may find it harder to do simple things.
Functional Limitations in Advanced OA
When osteoarthritis gets bad, it can really limit what you can do. You might find it hard to walk, climb stairs, or even get dressed. These problems can make you feel less independent and affect your happiness.
- Reduced mobility and flexibility
- Difficulty in performing daily activities
- Increased reliance on assistive devices
Is Osteoarthritis Considered a Disability?
In some cases, osteoarthritis can be seen as a disability. This happens when it makes it very hard to work or do everyday things. Whether it’s considered a disability depends on how bad it is and how it affects your life.
Key factors in determining disability include:
- The extent of joint damage and deformity
- The level of pain and its impact on function
- The presence of other comorbid conditions
VA Disability and Other Benefits for Osteoarthritis
Veterans with osteoarthritis caused by their service might get VA disability benefits. The VA helps those who got sick or hurt because of their time in the military. To get help, veterans need to show that their osteoarthritis is related to their service and meets the VA’s rules.
| Disability Rating | Compensation Level | Description |
| 0% | No compensation | Symptoms are present but do not impair function |
| 10%-30% | Partial compensation | Some impairment in function, with symptoms like pain |
| 40% or higher | Significant compensation | Severe impairment, significant loss of function |
Psychological Impact of Living with Chronic Osteoarthritis
Osteoarthritis can deeply affect a person’s mental health. It’s not just about physical pain; it also impacts emotions and mental well-being.
Depression and Anxiety in OA Patients
People with osteoarthritis often face depression and anxiety. The pain and limited movement can make them feel frustrated, sad, and alone.
Research shows that those with osteoarthritis are more likely to feel depressed and anxious. This can make managing the disease even harder, creating a cycle of physical and mental health issues.
Common symptoms of depression and anxiety in OA patients include:
- Persistent feelings of sadness or hopelessness
- Loss of interest in activities once enjoyed
- Increased worry or fear about the future
- Difficulty sleeping or concentrating
Coping Strategies and Mental Health Support
Managing osteoarthritis well means treating both the body and mind. There are many ways to cope with the mental effects of osteoarthritis.
Cognitive-behavioral therapy (CBT) is a helpful method for dealing with the emotional side of chronic illness. Support groups, online or in-person, also offer a sense of community and understanding.
Some recommended coping strategies include:
- Maintaining a positive outlook through mindfulness and relaxation techniques
- Staying connected with friends and family to combat feelings of isolation
- Engaging in activities that bring joy and fulfillment
- Seeking professional help when needed
By tackling both physical and mental aspects of osteoarthritis, people can enhance their quality of life. This helps them manage the challenges of living with chronic osteoarthritis better.
Lifestyle Modifications to Improve Outcomes
Making lifestyle changes is key to managing osteoarthritis symptoms. These changes can greatly improve your overall well-being.
Weight Management and Nutrition
Keeping a healthy weight is important for those with osteoarthritis. Excess weight can stress joints. Eating a balanced diet with fruits, vegetables, and omega-3 fatty acids can help manage weight and reduce inflammation.
Nutritional Tips:
- Add anti-inflammatory foods like turmeric and ginger to your meals.
- Drink plenty of water to stay hydrated.
- Reduce processed foods and sugars to lower inflammation.
Exercise and Physical Activity Recommendations
Regular exercise is essential for keeping joints mobile and muscles strong. Low-impact activities like swimming, cycling, and yoga are great choices.
Exercise Tips:
- Begin with gentle exercises and slowly increase the intensity.
- Add strength training to support your joints.
- Consider physical therapy for a tailored exercise plan.
Assistive Devices and Home Modifications
Using assistive devices and making home changes can lessen joint strain. Simple adjustments can greatly improve daily comfort and function.
Home and Device Suggestions:
- Choose ergonomic furniture and tools to reduce strain.
- Install handrails and non-slip mats in key spots.
- Use a walking aid if you have mobility issues.
By making these lifestyle changes, people with osteoarthritis can better manage symptoms and enjoy a better quality of life.
Special Considerations: Rare and Severe Forms of OA
Osteoarthritis comes in many forms, some rare and severe. It’s important to know and treat these types well to avoid a lot of suffering. Each rare form has its own challenges in diagnosis and treatment.
Generalized Osteoarthritis and Bilateral OA
Generalized osteoarthritis affects many joints at once, often in a symmetrical way. This can lead to a lot of pain and stiffness, making it hard to move. When OA affects both sides of the body, it makes the problem even worse.
Key features of generalized osteoarthritis include:
- Multi-joint involvement
- Symmetrical distribution
- Potential for rapid progression
Erosive and End-Stage Osteoarthritis
Erosive osteoarthritis is more aggressive, causing serious damage to joints. It shows up as erosive lesions on scans. End-stage osteoarthritis is the last stage, where joints are badly damaged and might need surgery.
Erosive osteoarthritis is distinguished by:
- Rapid joint damage
- Erosive changes visible on radiographs
- Increased risk of deformity and disability
Heberden’s Nodes and Other Distinctive Features
Heberden’s nodes are bony growths on the fingers, a sign of osteoarthritis. Other signs include Bouchard’s nodes and joint deformities.
| Distinctive Feature | Description |
| Heberden’s Nodes | Bony enlargements of the distal interphalangeal joints |
| Bouchard’s Nodes | Involvement of the proximal interphalangeal joints |
It’s key to understand these rare and severe forms of osteoarthritis. This knowledge helps doctors give better care and improve patient outcomes. By knowing each condition’s unique traits, doctors can create treatment plans that fit each patient’s needs.
Conclusion: Living Well with Osteoarthritis
Living with osteoarthritis means using a wide range of strategies and making lifestyle changes. Knowing about the condition helps people take action to better their lives.
Managing osteoarthritis involves several steps. This includes losing weight, exercising, and sometimes surgery. It also means finding ways to handle pain, both with and without medicine.
By living healthily and following treatment plans, people with osteoarthritis can lessen its effects. They can make their homes easier to move around in, use tools to help them, and get help for their mental health.
Living well with osteoarthritis means tackling it from all angles. It’s about taking care of the body, mind, and social life. By focusing on management and making smart choices, people can stay happy and healthy.
FAQ
Can osteoarthritis kill you?
Osteoarthritis itself is not usually life-threatening. But, it can lead to serious issues like limited mobility. This can increase the risk of other health problems.
What is the life expectancy of someone with osteoarthritis?
People with osteoarthritis usually live as long as others. But, their quality of life can be affected. The severity of the condition and how well it’s managed play big roles.
Is osteoarthritis considered a disability?
Yes, if osteoarthritis makes it hard to do daily tasks or work. The VA might consider it a disability based on how severe it is.
How does osteoarthritis affect different body parts?
It can hit various joints, like knees, hips, and hands. Each area’s impact varies. Some feel pain and stiffness, while others face bigger challenges.
What are the risk factors that may worsen the prognosis of osteoarthritis?
Older age, obesity, and past injuries can make osteoarthritis worse. So can genetics and lifestyle choices. Other health issues, like diabetes, can also affect outcomes.
How is osteoarthritis diagnosed?
Doctors use symptoms, physical exams, and X-rays to diagnose it. They check for signs and might use imaging tests to confirm.
What are the treatment options for osteoarthritis?
Treatments range from lifestyle changes to surgery. Current guidelines suggest a mix of approaches to manage symptoms and improve life quality.
Can osteoarthritis cause swelling?
Yes, it can cause swelling in joints like hands and knees. This swelling often comes with pain, stiffness, and less mobility.
How can osteoarthritis be managed?
Managing it involves lifestyle changes and pain relief strategies. Effective management can reduce symptoms and improve life quality.
What is the natural progression of osteoarthritis?
It progresses differently for everyone. Early stages might have mild symptoms. But, as it gets worse, pain, stiffness, and mobility issues can become severe.
Can you die from osteoarthritis?
Osteoarthritis itself doesn’t usually cause death. But, it can indirectly lead to mortality through complications like mobility issues and related health problems.
What are the complications of untreated osteoarthritis?
Untreated osteoarthritis can lead to physical and mental health issues. Complications include increased pain, mobility loss, depression, and anxiety.
How does osteoarthritis impact mental health?
It can significantly affect mental health, causing depression and anxiety. Effective management and support can help manage these effects.
References
- Petersen, S. G., & Waehrens, E. E. (2020). Osteoarthritis, mobility-related comorbidities and mortality: An overview of meta-analyses. Journal of Clinical Rheumatology, 27(7), 269–275. https://www.researchgate.net/publication/347972649_Osteoarthritis_mobility-related_comorbidities_and_mortality_an_overview_of_meta-analyses





