Last Updated on November 20, 2025 by Ugurkan Demir
Sickle cell anemia is a genetic disorder that affects how red blood cells are made. It makes these cells misshapen and prone to breaking down. This can lead to anemia, blood clots, and organ damage.
Many people wonder, can sickle cell anemia cause blood clots? Recent studies have found that sickle cell anemia does increase the risk of clot formation. These clots often form in veins, which can lead to serious health complications. Understanding this link is key to managing and treating the condition effectively.
Key Takeaways
- Sickle cell anemia is a genetic disorder affecting hemoglobin production.
- Misshapen red blood cells can cause various complications.
- The condition increases the risk of blood clots, particular in veins.
- Understanding the link between sickle cell anemia and blood clots is key.
- Liv Hospital offers advanced care for related issues.
Understanding Sickle Cell Anemia

Sickle cell anemia is a complex genetic disorder. It affects how red blood cells make hemoglobin, a key protein. This condition is caused by abnormal hemoglobin, known as sickle hemoglobin or HbS.
What Is Sickle Cell Anemia?
Sickle cell anemia changes how red blood cells work. It comes from a gene mutation in the HBB gene. This mutation makes HbS, causing red blood cells to change shape and break down. This leads to anemia, pain episodes, and a higher risk of infections.
Genetic Basis of Sickle Cell Disease
The genetic cause of sickle cell disease is a point mutation in the HBB gene. It’s inherited in an autosomal recessive pattern. This means you need two defective copies of the gene (one from each parent) to have the condition.
The National Institutes of Health says, “Sickle cell disease is caused by a mutation in the HBB gene. This mutation leads to sickle hemoglobin production.”
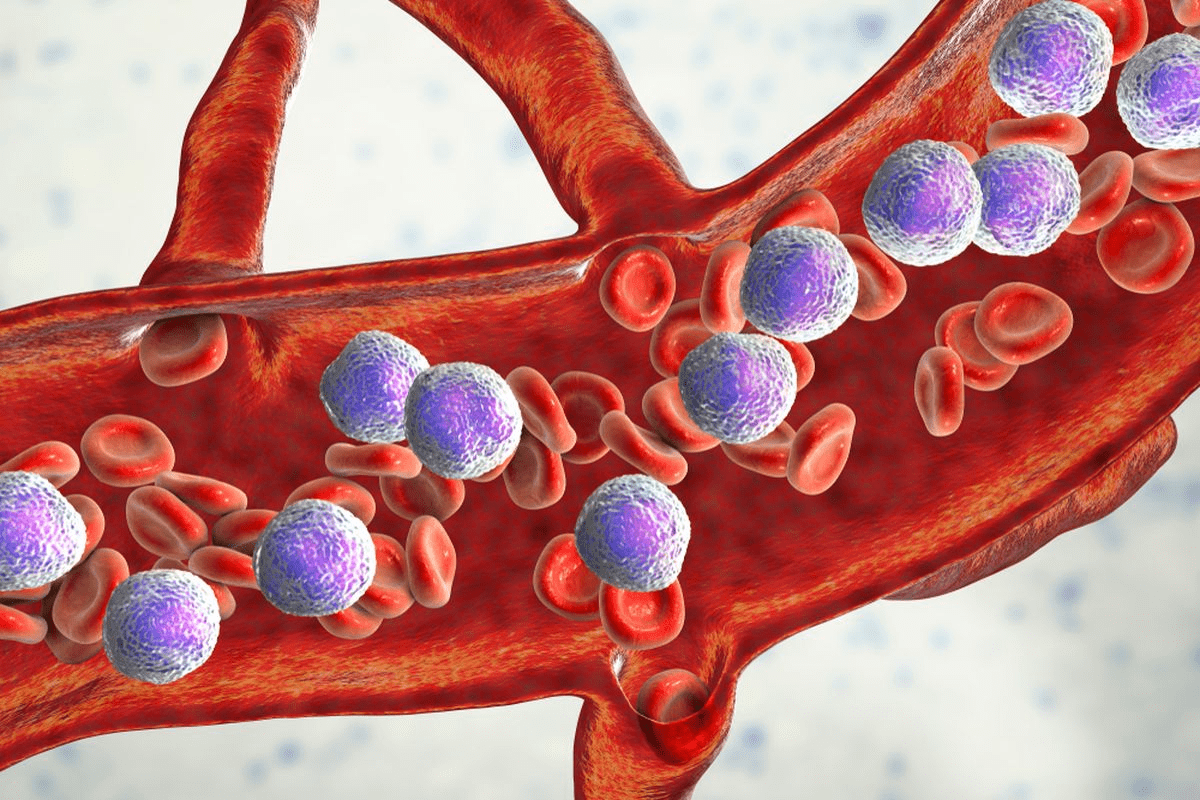
How Sickle Cell Affects Red Blood Cells
Red blood cells with HbS become rigid and sickle-shaped in low oxygen. These sickled cells are more likely to be destroyed, causing anemia.
These abnormal cells can also block small blood vessels, causing vaso-occlusive crises. According to
“Sickle cell disease is associated with a significant risk of vascular complications, including vaso-occlusive crises and increased risk of stroke.”
–
Knowing how sickle cell anemia affects red blood cells is key. It helps in finding better ways to manage and treat the condition.
The Relationship Between Blood Cells and Clotting
Blood clotting is a complex process that involves many cell types. These include red blood cells, platelets, and white blood cells. Knowing how these cells work together is key to understanding clot formation and how problems with these cells can cause clotting issues.
Normal Blood Clotting Process
Blood clotting is essential to stop bleeding when a blood vessel is hurt. It starts with platelets getting activated, sticking together, and forming a fibrin clot. Red blood cells are important because they help the clot form and shape it.
Role of Red Blood Cells in Clot Formation
Red blood cells are vital for clotting. They release ADP, which helps platelets stick together. They also get trapped in the clot, making it thicker and changing its shape.
The role of red blood cells in clotting can be summarized in the following table:
| Role | Description |
| Release of ADP | Promotes platelet activation and aggregation |
| Trapping within fibrin mesh | Adds bulk to the clot and influences its structure |
How Abnormal Blood Cells Affect Clotting
Abnormal blood cells, like those in sickle cell anemia, can change how clots form. Sickled red blood cells are stiffer and stickier, leading to more and different clots. This can increase the risk of blood clots.
“The presence of sickled red blood cells can lead to a prothrombotic state, characterized by increased clot formation and stability.” This highlights the need to understand the impact of abnormal red blood cells on clotting.
In conclusion, the connection between blood cells and clotting is complex. Understanding how different cells contribute to clotting and how problems with these cells can cause issues is key to finding effective treatments.
Can Sickle Cell Anemia Cause Blood Clots?
It’s important to understand how sickle cell anemia and blood clots are connected. Sickle cell anemia is a genetic disorder that affects how red blood cells make hemoglobin. This makes the cells misshapen and prone to breaking down.
The Direct Connection Between Sickled Cells and Clotting
Sickled red blood cells tend to clump together and block blood vessels. This can cause blood clots to form. Sickled cells stick together more easily, raising the risk of blood clots.
- Sickled cells are more likely to stick together and form clots.
- The abnormal shape of sickled cells can cause them to get stuck in small blood vessels.
- This can lead to a reduction in blood flow and increase the risk of clot formation.
Scientific Evidence Supporting the Link
Recent studies have shown a link between sickle cell anemia and blood clots. People with sickle cell anemia are more likely to get venous thromboembolism. This is when blood clots form in the deep veins.
These findings stress the need to watch for clotting signs in those with sickle cell anemia. It’s also important to take steps to prevent blood clots.
Mechanisms Behind Increased Clotting Risk
The reasons for the higher clotting risk in sickle cell anemia are complex. The abnormal shape and behavior of sickled red blood cells play a big role. Inflammation and the activation of clotting pathways also contribute.
- Abnormal sickled red blood cells can cause chronic inflammation.
- Inflammation can activate the body’s clotting mechanisms.
- The combination of these factors increases the risk of blood clot formation.
In conclusion, there’s solid scientific evidence linking sickle cell anemia to blood clots. This highlights the need for careful management and monitoring. It helps prevent serious blood clot complications.
Venous Thromboembolism in Sickle Cell Disease
Venous thromboembolism is a serious issue in sickle cell disease. It includes deep vein thrombosis and pulmonary embolism, both dangerous. Sickle cell disease and venous thromboembolism have a complex relationship, involving many pathological processes.
Prevalence of VTE in SCD Patients
People with SCD face a higher risk of VTE. The rate of VTE in SCD patients is much higher than in the general population. This is due to chronic hemolysis, inflammation, and damage to blood vessels.
Key statistics highlighting the prevalence include:
- Increased incidence of VTE in SCD patients compared to those without the disease.
- Higher rates of recurrence of VTE in SCD patients.
Risk Factors for Developing Blood Clots with SCD
Several factors increase the risk of blood clots in SCD patients. These include:
- Genetic predispositions that affect coagulation pathways.
- Chronic inflammation and oxidative stress.
- Previous episodes of VTE.
- Immobilization and surgery.
Understanding these risk factors is key to managing and preventing VTE in SCD patients.
Unique Characteristics of Clots in SCD Patients
The clots in SCD patients are different from those in the general population. They are denser and harder to break down.
| Characteristics | Description |
| Increased Density | Clots in SCD patients are denser due to the altered red blood cell morphology. |
| Resistance to Fibrinolysis | The clots are more resistant to breakdown, contributing to the increased risk of VTE. |
Managing VTE in SCD patients requires a detailed approach. It must consider the unique clot characteristics and underlying risk factors.
Deep Vein Thrombosis and Sickle Cell Disease
People with sickle cell disease face a higher risk of deep vein thrombosis. This is when blood clots form in the deep veins, usually in the legs. It can cause serious problems and even be life-threatening if not treated quickly.
Recognizing DVT in SCD Patients
It’s hard to spot deep vein thrombosis in sickle cell disease patients. Symptoms like pain, swelling, and warmth in the leg can also show up in other SCD issues. This makes it tough to diagnose.
Clinical vigilance is key to catching DVT early. Doctors need to watch patients closely, even more so when they’re sick or in the hospital.
Why DVT Is More Common in Sickle Cell Disease
The abnormal blood cells in SCD make it easier for clots to form. These cells can damage blood vessel walls and cause inflammation. This makes it more likely for clots to develop.
Other things like genetic predispositions, immobility, and previous history of thrombotic events also play a role. Knowing these factors helps in finding ways to prevent and treat DVT in SCD patients.
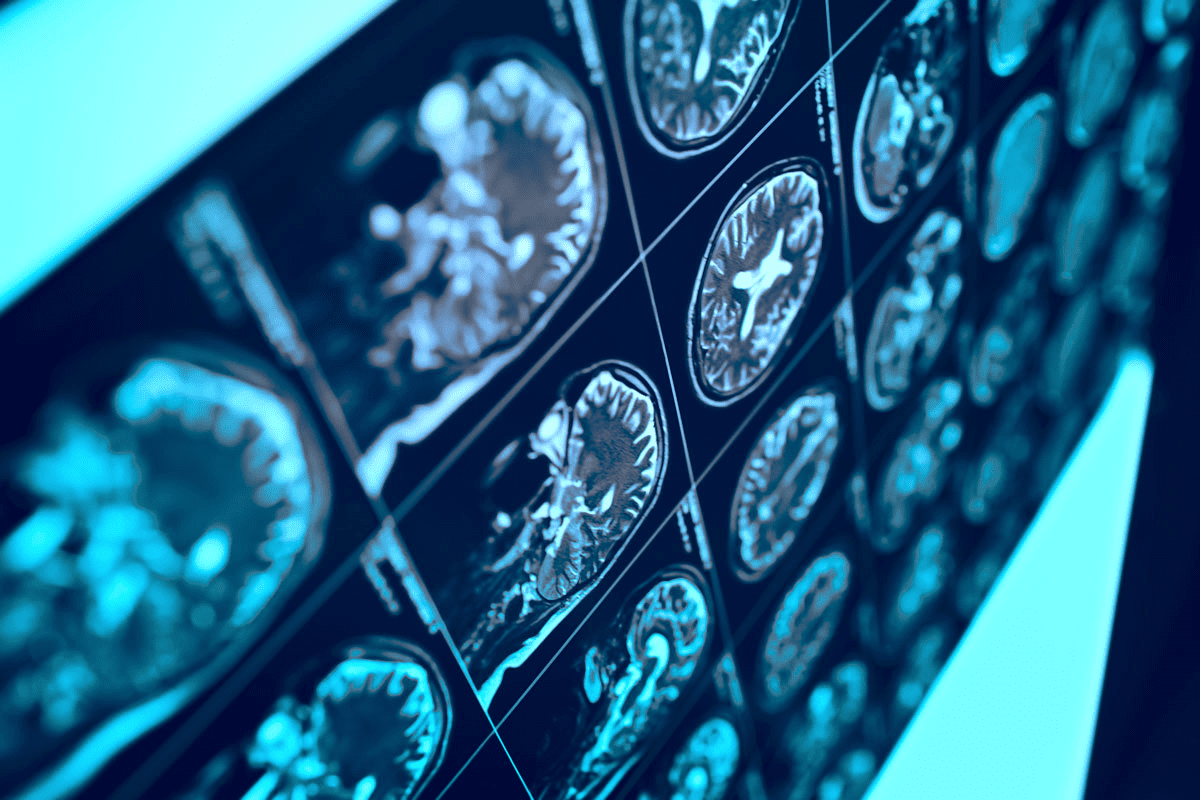
Diagnostic Challenges in SCD Patients
Diagnosing DVT in SCD patients is tricky. Symptoms can be similar to other conditions, and the D-dimer test can be misleading. This is because SCD patients often have ongoing hemolysis and inflammation.
So, a detailed approach is needed. This includes clinical assessment, imaging studies like ultrasound, and careful lab test interpretation. This helps doctors accurately diagnose DVT and start the right treatment.
Pulmonary Embolism Risks in Sickle Cell Patients
People with sickle cell disease (SCD) face a higher risk of pulmonary embolism (PE). This is because their red blood cells can stick together and block blood flow. This blockage can be very dangerous.
Increased PE Risk with Sickle Cell Trait
Those with sickle cell trait (SCT) also have a higher risk of PE. Research shows that SCT can make blood more likely to clot. This increases the chance of blood clots forming.
Sickle cell trait is usually seen as harmless. But, it can cause problems during hard exercise or at high altitudes. These situations can lead to blood clots.
Warning Signs and Symptoms
It’s important to know the signs of PE. Look out for shortness of breath, chest pain, and hemoptysis. Doctors need to watch for these in SCD patients.
Emergency Management of PE in SCD Patients
Handling PE in SCD patients needs a team effort. Hematologists, cardiologists, and emergency doctors all play a role. Anticoagulation therapy is key to stop more clots from forming.
SCD patients with PE need close monitoring. Watch for signs of heart problems or more clots. In serious cases, thrombolytic therapy might be used.
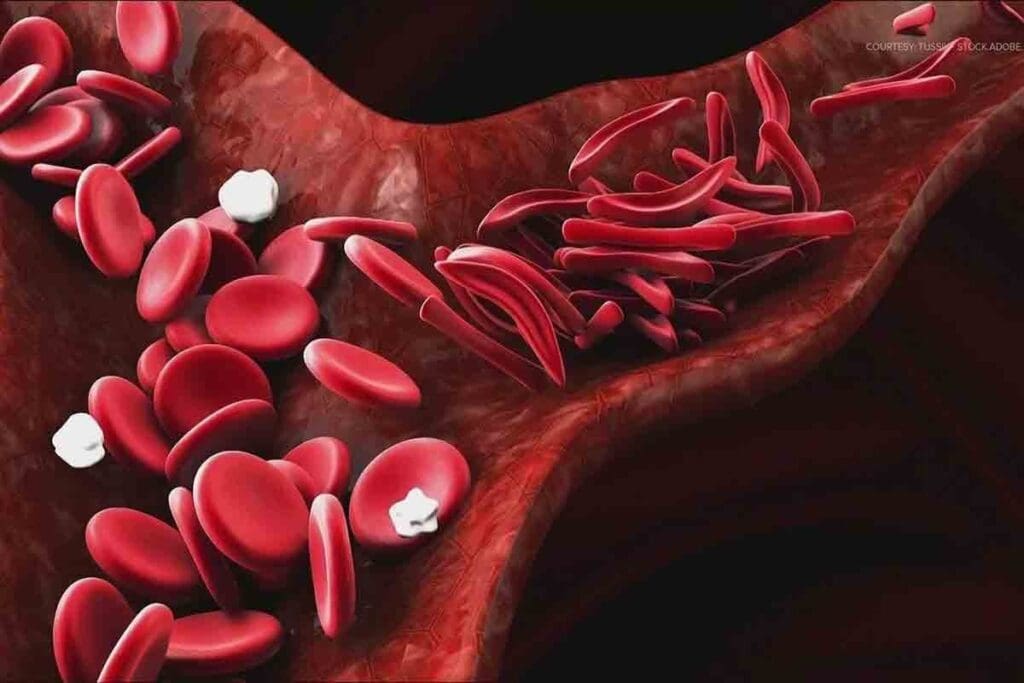
How Sickle Cell Anemia Alters Clot Structure
Sickle cell anemia changes blood clots, making them denser and harder to break down. This is mainly because of the abnormal red blood cells found in sickle cell disease (SCD).
The abnormal red blood cells in SCD can trigger inflammatory responses that affect how clots form. These responses release cytokines and chemokines, which help clots form.
Density and Resistance of Clots in SCD
Research shows that SCD clots are denser and harder to dissolve than normal clots. This is because of the sickled red blood cells, which change the clotting process.
Clot density in SCD patients can be measured in labs. Here’s a table comparing clot density in SCD patients and healthy people:
| Parameter | SCD Patients | Healthy Controls |
| Clot Density (g/cm³) | 1.25 ± 0.05 | 1.15 ± 0.03 |
| Fibrinolysis Time (min) | 45 ± 10 | 30 ± 5 |
Inflammatory Responses and Clot Formation
Inflammatory responses are key in changing clot structure in SCD. Sickled red blood cells start an inflammatory cascade that helps clots form and stay stable.
Abnormal Activation of Clotting Pathways
The clotting pathways are also abnormally activated in SCD. Sickled red blood cells activate the coagulation cascade, leading to denser clots.
In summary, SCD’s clot structure changes involve clot density, inflammatory responses, and clotting pathway activation. Understanding these changes is vital for managing clotting issues in SCD.
Comparing Clotting Risks: Sickle Cell vs. Other Anemias
SCD has a unique way of affecting the body compared to other anemias. Anemia means not enough red blood cells or hemoglobin. This can lead to blood clots, but the risk varies with each type of anemia.
Clotting Tendencies in Different Types of Anemia
Each anemia type affects clotting differently. For example, iron deficiency anemia doesn’t usually raise clotting risk much. But hemolytic anemias, where red cells break down fast, might increase the risk because of pro-coagulant factors from damaged cells.
SCD is a type of hemolytic anemia. It causes red cells to break down, leading to chronic inflammation and blood flow issues. These problems make it more likely for blood clots to form.
Why SCD Carries Higher Thrombotic Risk
SCD’s higher clotting risk comes from several factors. Sickled red cells can block small blood vessels, causing tissue damage. This damage triggers inflammation and activates the coagulation system, raising clotting risk even more.
- Abnormal red blood cells can cause vaso-occlusion.
- Chronic hemolysis releases pro-coagulant factors.
- Endothelial dysfunction promotes clotting.
The Bidirectional Relationship Between Anemia and Clots
Anemia and clotting risks are linked in a complex way. Anemia can increase clotting risk due to the body’s efforts to make more red blood cells. But clots can also worsen anemia by using up clotting factors and causing more problems.
In SCD, this relationship is very important. The disease causes both chronic anemia and a higher risk of blood clots. Knowing this helps doctors manage SCD patients better and lower their clotting risks.
Treatment Approaches for Preventing Blood Clots in SCD
Stopping blood clots is key in managing SCD. Several treatments are available to help. SCD patients face a higher risk of blood clots because of sickled red blood cells. This can cause vaso-occlusive crises and other problems.
Anticoagulation Therapy Considerations
Anticoagulation therapy is a common way to prevent blood clots in SCD patients. It uses medicines that stop clots from forming. But, it also raises the risk of bleeding.
Starting anticoagulation therapy needs careful thought. It depends on the patient’s risk factors, medical history, and current health. Regular monitoring is essential to avoid bad effects.
- Assessing the patient’s risk of bleeding and clotting
- Selecting the appropriate anticoagulant medication
- Monitoring the patient’s response to therapy
Hydroxyurea and Other SCD Treatments
Hydroxyurea can reduce vaso-occlusive crises and other SCD complications. It increases fetal hemoglobin production. This helps reduce red blood cell sickling.
Other treatments for SCD include blood transfusions, pain meds, and antibiotics. The right treatment depends on the patient’s needs and medical history.
“The use of hydroxyurea has been shown to significantly reduce the risk of complications associated with SCD, including blood clots.”
Source: National Heart, Lung, and Blood Institute
Balancing Bleeding and Clotting Risks
Managing SCD is about finding a balance. We need to prevent blood clots but also avoid bleeding. Anticoagulation therapy and other treatments must be carefully adjusted.
| Treatment Approach | Bleeding Risk | Clotting Risk |
| Anticoagulation Therapy | High | Low |
| Hydroxyurea | Low | Moderate |
Understanding the risks and benefits of treatments helps healthcare providers manage SCD. They can then prevent blood clots effectively.
Conclusion
Sickle cell disease (SCD) is a complex condition that needs careful management. This is to prevent blood clots and their serious health effects. People with SCD are at a higher risk of getting blood clots.
A recent study looked at data from over four million people. It found that those with the sickle cell trait face a 1.45 times higher risk of venous thromboembolism. This risk is the same for all genetic backgrounds. Carriers of the sickle cell trait are more likely to get pulmonary embolism than deep vein thrombosis.
Healthcare providers can help SCD patients by acknowledging the risks. They can also use the right treatments. This can help reduce the risk of blood clots and improve their quality of life.
FAQ
Can sickle cell anemia cause blood clots?
Yes, sickle cell anemia can lead to blood clots, mainly in veins. The sickle-shaped red blood cells can cause clots to form. This can lead to serious issues like deep vein thrombosis and pulmonary embolism.
What is the relationship between anemia and blood clots?
Anemia, like sickle cell anemia, can raise the risk of blood clots. The sickle-shaped red blood cells can trigger inflammation and start clotting pathways. This leads to blood clots forming.
Can anemia cause blood clots in legs?
Yes, anemia, like sickle cell anemia, can increase the risk of blood clots in legs. This can cause deep vein thrombosis. The sickle-shaped red blood cells can form clots, which can be dangerous if not treated.
How does sickle cell disease affect blood clotting?
Sickle cell disease can change how clots form, making them denser and harder to break down. The sickle-shaped red blood cells can also cause inflammation and start clotting pathways. This leads to blood clots forming.
What are the risks associated with blood clots in sickle cell disease?
Blood clots in sickle cell disease can lead to serious problems. These include deep vein thrombosis, pulmonary embolism, and organ damage. It’s important to treat them quickly to prevent these issues.
Can blood clots cause anemia?
Blood clots are not a direct cause of anemia. But, they can be a complication of anemia, like sickle cell anemia. The sickle-shaped red blood cells can cause clots, leading to more complications.
What is the treatment for preventing blood clots in sickle cell disease?
There are treatments to prevent blood clots in sickle cell disease. These include anticoagulation therapy and hydroxyurea. The goal is to reduce the risk of blood clots and manage the disease.
Does anemia cause blood clots?
Certain anemias, like sickle cell anemia, can increase the risk of blood clots. The sickle-shaped red blood cells can cause inflammation and start clotting pathways. This leads to blood clots forming.
What is the connection between sickle cell trait and blood clots?
Sickle cell trait can increase the risk of blood clots, like pulmonary embolism. People with sickle cell trait should watch for signs of blood clots. If they notice anything unusual, they should seek medical help.
Can fever and blood clots be related to sickle cell disease?
Yes, fever and blood clots can be related to sickle cell disease. Fever can be a sign of infection or inflammation. This can increase the risk of blood clots in people with sickle cell disease.
References
- Noubiap, J. J., Temgoua, M. N., Tankeu, R., Ondongo-Bekama, J. P., Sinouira, E., Kingue, S., & Wonkam, A. (2018). Sickle cell disease, sickle trait and the risk for venous thromboembolism: A systematic review and meta-analysis. Thrombosis Journal, 16(1), 27. https://pmc.ncbi.nlm.nih.gov/articles/PMC6171302/