Anterior uveitis is a serious eye condition that can cause permanent vision loss if not treated. We know how important it is to diagnose and treat it quickly to save blindness sight.
At Liv Hospital, we combine top ophthalmology skills with care focused on the patient. We aim to understand anterior uveitis well, giving our patients the best care.
This condition affects many people, mostly between 20 and 60 years old. It impacts about 1 in 4,500 people. Knowing the treatment options is key.
Key Takeaways
- Anterior uveitis is a serious inflammatory eye condition.
- Prompt diagnosis is key to avoid vision loss.
- Liv Hospital offers complete care for anterior uveitis.
- Knowing the causes and symptoms is essential for good treatment.
- World-class ophthalmology expertise is available for patients.
Understanding Anterior Uveitis
Anterior uveitis is an inflammation of the iris and the front part of the ciliary body. It causes symptoms like pain, light sensitivity, and vision issues. This condition is a big problem for eye health and can happen to people of all ages.
Definition and Anatomical Involvement
It affects the front part of the uvea, which includes the iris and the ciliary body. The uvea is the middle layer of the eye, important for blood supply and color. When it gets inflamed, it can cause eye pain, light sensitivity, and vision problems.
The parts affected are the iris and the front of the ciliary body. This can happen for many reasons, like autoimmune diseases, infections, or injuries.
Prevalence and At-Risk Demographics
Anterior uveitis is the most common type of uveitis, making up most cases. It usually happens to people between 20 and 60 years old. Some groups are more likely to get it.
How common it is can vary in different groups. Some studies show it’s more common in people with certain genetic markers, like HLA-B27.
Demographic | Characteristics | Risk Factors |
Age | 20-60 years | Increased risk with certain genetic predispositions |
Genetic Markers | HLA-B27 positive | Higher risk of developing anterior uveitis |
Associated Conditions | Autoimmune disorders, infections | Increased susceptibility to anterior uveitis |
Types of Anterior Uveitis
It’s important to know the different types of anterior uveitis for better care. This condition can be acute or chronic, affecting treatment plans.
Acute vs. Chronic Presentations
Acute anterior uveitis starts suddenly and lasts less than three months. It’s often linked to sudden inflammation and diseases like HLA-B27-related ones.
Chronic anterior uveitis lasts more than three months. It can cause serious issues like synechiae, cataract, and glaucoma. Long-term treatment and monitoring are needed for chronic cases.
Characteristics | Acute Anterior Uveitis | Chronic Anterior Uveitis |
Duration | Less than 3 months | More than 3 months |
Onset | Sudden | Gradual or persistent |
Associated Conditions | HLA-B27-related diseases | Various autoimmune or infectious conditions |
Granulomatous vs. Non-Granulomatous Forms
Anterior uveitis can be granulomatous or non-granulomatous. Granulomatous anterior uveitis has granulomas, seen in sarcoidosis and tuberculosis.
“The presence of granulomas in anterior uveitis indicates a specific type of inflammatory response that requires tailored treatment strategies.” – Expert Opinion
Non-granulomatous anterior uveitis doesn’t have granulomas. It’s more common in HLA-B27-related diseases or other autoimmune conditions. Knowing the difference helps in diagnosis and treatment.
Understanding the types of anterior uveitis helps doctors manage it better. This leads to better patient outcomes.
Recognizing Symptoms of Anterior Uveitis
It’s key to spot the signs of anterior uveitis early to avoid serious issues. This condition, also called anterior iritis, shows different symptoms that can really affect a person’s life.
Primary Clinical Manifestations
The main signs of anterior uveitis are eye pain, redness, photophobia, and blurred vision. These happen because of inflammation in the eye, mainly in the uveal tract.
Eye pain is a big issue, feeling like a dull ache or sharp stab. The eye often looks red, or has conjunctival injection, because of more blood flow.
Photophobia, or light sensitivity, is really tough for people. It makes everyday tasks hard. Blurred vision also happens because the inflammation messes with the eye’s focus.
Warning Signs Requiring Immediate Medical Attention
While these symptoms are common, some signs mean you need to see a doctor right away. Severe eye pain, big vision loss, or intense light sensitivity are red flags.
If you’re experiencing these severe symptoms, get medical help fast. Waiting too long can cause serious problems like secondary glaucoma, cataract formation, or permanent vision loss.
It’s really important to act quickly when dealing with anterior uveitis. Spotting symptoms early and knowing when to get help can greatly improve your chances of a good outcome.
Endogenous Anterior Uveitis: Pathophysiology and Causes
The causes of endogenous anterior uveitis are varied. They include autoimmune, infectious, and unknown factors. Knowing these causes helps in creating better treatment plans.
Autoimmune Mechanisms
Autoimmune responses are key in endogenous anterior uveitis. Autoimmune diseases make the body attack its own tissues. This can cause inflammation in the eye’s front chamber.
Diseases like ankylosing spondylitis often lead to anterior uveitis. This shows a strong link between autoimmune issues and this eye condition.
Infectious Triggers
Infections can also start endogenous anterior uveitis. Bacterial, viral, and fungal infections can cause eye inflammation. This can happen through direct infection or an immune reaction.
For example, herpes simplex virus can infect the eye’s tissues. This leads to anterior uveitis.
Idiopathic Cases
Many cases of endogenous anterior uveitis have no known cause. Despite detailed investigations, the reason remains a mystery.
In these cases, genetic predisposition and environmental factors might be involved. This makes the condition complex.
Understanding the causes of endogenous anterior uveitis is vital for treatment. Knowing if it’s due to autoimmunity, infections, or is unknown helps doctors tailor treatments. This ensures the best care for each patient.
Genetic Factors in Anterior Uveitis
Genetics play a big role in getting anterior uveitis. Some genes make you more likely to get it. We’ll look at the HLA-B27 link and other genes involved.
The HLA-B27 Connection
The HLA-B27 gene is closely tied to anterior uveitis. This is true for people with ankylosing spondylitis and other spondyloarthropathies. Research shows that having HLA-B27 ups your risk of getting anterior uveitis.
HLA-B27 Association: Having HLA-B27 is a big risk factor for anterior uveitis. This is true, even more so for those with ankylosing spondylitis.
Genetic Marker | Association with Anterior Uveitis | Clinical Significance |
HLA-B27 | Strongly associated | Increased risk in patients with ankylosing spondylitis |
Other HLA alleles | Moderately associated | Variable risk depending on the specific allele |
Other Genetic Associations
Other genes also play a part in getting anterior uveitis. Studies have found several genes that might affect your risk.
“The genetic landscape of anterior uveitis is complex, involving multiple genetic variants that interact with environmental factors to trigger the onset of the disease.” – Medical Expert, Ophthalmology Expert
Knowing about these genes is key for better treatment plans. It helps improve how well patients do.
Systemic Conditions Associated with Anterior Uveitis
Anterior uveitis is connected to many autoimmune diseases. This shows we need to treat patients in a more complete way. It’s key to know these connections for better care.
Ankylosing Spondylitis and Spondyloarthropathies
Ankylosing spondylitis and other spondyloarthropathies often go hand in hand with anterior uveitis. Research shows people with ankylosing spondylitis are more likely to get anterior uveitis. This usually starts suddenly and can happen many times.
Key characteristics include:
- Acute onset of symptoms
- Recurrent episodes
- Association with HLA-B27 positivity
Inflammatory Bowel Disease
Inflammatory bowel disease (IBD), like Crohn’s and ulcerative colitis, is also linked to anterior uveitis. The inflammation in IBD can cause eye problems, including uveitis.
“The link between IBD and anterior uveitis shows we need a team effort to care for these patients.”
Other Autoimmune Conditions
Other autoimmune diseases, like psoriatic arthritis and reactive arthritis, can also cause anterior uveitis. These cases show how autoimmune diseases affect our eyes.
It’s important for doctors to understand these connections. By knowing how anterior uveitis relates to other diseases, we can give better care. This helps us create more effective treatment plans.
Diagnostic Approach to Anterior Uveitis
To diagnose anterior uveitis, we use a detailed method. This includes a clinical exam, lab tests, and imaging studies.
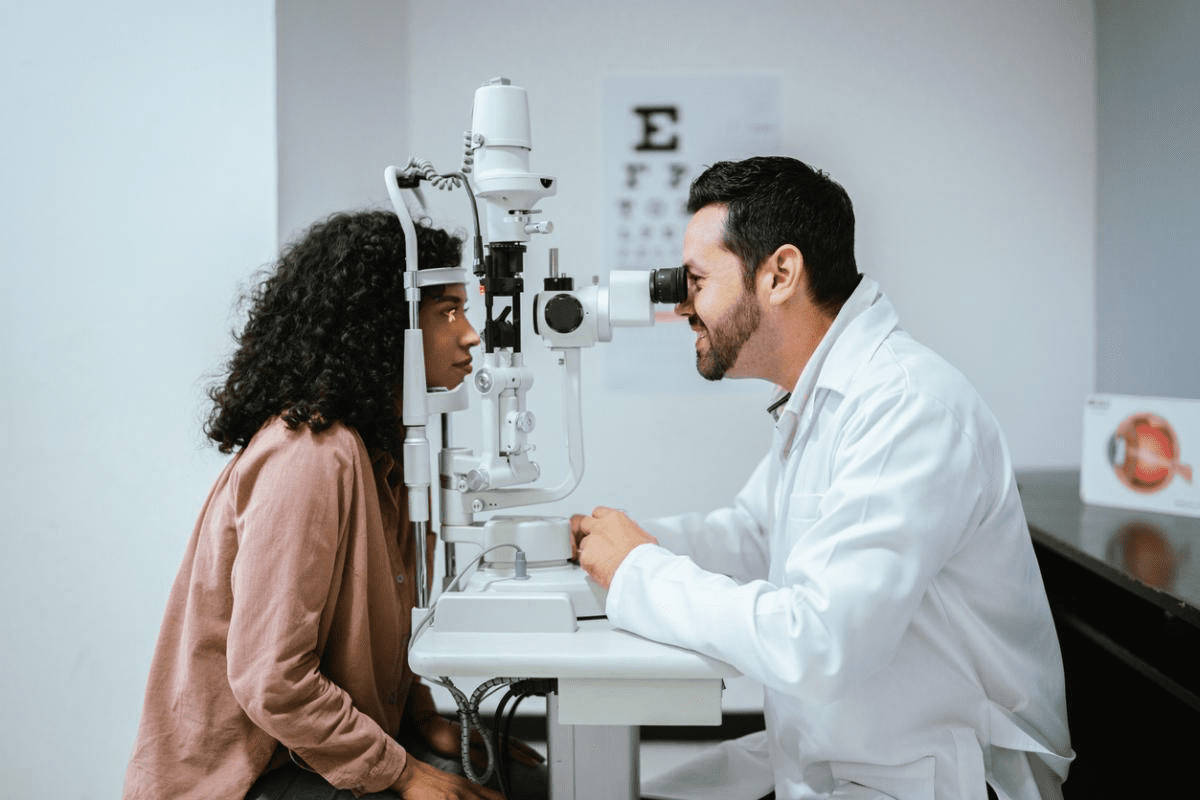
Clinical Examination Techniques
A detailed clinical exam is key for diagnosing anterior uveitis. We use a slit-lamp examination to check the front part of the eye for inflammation. This helps us see how severe the inflammation is and if there are any complications.
We also check your vision, eye pressure, and the back of the eye for other issues.
Laboratory Testing
Lab tests are important to find out why you have anterior uveitis. We test for infections, autoimmune diseases, and other conditions that might be linked to it.
- Complete Blood Count (CBC): To check for infections or inflammation.
- Erythrocyte Sedimentation Rate (ESR) or C-Reactive Protein (CRP): To see how much inflammation there is.
- Serological Tests: Like HLA-B27 typing to look for genetic links.
Imaging Studies
Imaging studies help us see how much inflammation there is and if there are any complications. We often use:
- Optical Coherence Tomography (OCT): To check the retina for problems like macular edema.
- Ultrasound Biomicroscopy (UBM): To get a close look at the front part of the eye, even if it’s hard to see with a slit-lamp.
First-Line Treatment Protocols
Treating anterior uveitis starts with a mix of topical corticosteroids and cycloplegic agents. This approach aims to cut down inflammation, ease pain, and stop complications like synechiae.
Topical Corticosteroid Therapy
Topical corticosteroids are key in treating anterior uveitis. They help reduce inflammation and prevent tissue damage. The type and how often you use it depends on how bad the uveitis is.
Corticosteroid Options:
- Prednisolone acetate 1% is often chosen for its strong anti-inflammatory effects.
- Dexamethasone is another choice, with different strength and how long it lasts.
Cycloplegic and Mydriatic Agents
Cycloplegic and mydriatic agents ease pain from ciliary spasm and stop synechiae from forming. They also help keep the blood-aqueous barrier stable and lower the risk of problems.
Cycloplegic Options:
- Atropine sulfate is a common choice for its pain relief and synechiae prevention.
- Cyclopentolate is another option, known for its quick action.
Treatment Duration and Tapering
How long you treat and tapering corticosteroids and cycloplegics are key to avoid issues like steroid-induced glaucoma or cataracts. Tapering should be slow, based on how well you’re doing.
Treatment Phase | Medication | Frequency | Duration |
Acute Phase | Prednisolone acetate 1% | Every 1-2 hours | 1-2 weeks |
Tapering Phase | Prednisolone acetate 1% | Gradually reduced | 4-6 weeks |
By following these first-line treatment protocols, doctors can manage anterior uveitis well. This reduces the chance of complications and improves patient results.
Advanced Treatment for Refractory Cases
When first treatments don’t work, patients with anterior uveitis need stronger help. Advanced treatments are key to managing tough cases and avoiding serious problems later.
Systemic Corticosteroids
Systemic corticosteroids are used when inflammation is too strong or local treatments don’t work. They help reduce inflammation but can have side effects that need watching.
Key Considerations for Systemic Corticosteroid Use:
- Dosage and how long to use it
- Watching for side effects like bone loss, diabetes, and high blood pressure
- Slowly reducing the dose to avoid withdrawal
Immunomodulatory Therapy
For long-term inflammation control, immunomodulatory therapy (IMT) is a good choice. IMT helps lessen the need for corticosteroids and manages the immune system.
Therapeutic Agent | Mechanism of Action | Common Use in Anterior Uveitis |
Methotrexate | Inhibits DNA synthesis, reducing inflammation | Chronic anterior uveitis |
Cyclosporine | Suppresses T-cell activation | Severe, refractory cases |
Azathioprine | Suppresses immune cell proliferation | Chronic cases, often in combination therapy |
Biologic Agents
Biologic agents are a new type of treatment that targets the immune system. They’re great for cases where usual treatments don’t work.
Examples of Biologic Agents Used:
- Adalimumab: Anti-TNF alpha agent used in non-infectious uveitis
- Infliximab: Another anti-TNF alpha agent effective in refractory cases
These advanced treatments offer hope for patients with tough anterior uveitis. They help control inflammation well and may improve outcomes.
Managing Complications and Preventing Recurrence
Managing anterior uveitis is more than just treating it. It’s about tackling complications and stopping it from coming back. We know it’s a big challenge. It involves treating the condition, improving the patient’s life, and stopping future episodes.
Addressing Secondary Complications
Anterior uveitis can cause problems like cataracts, glaucoma, and macular edema. It’s important to spot and manage these issues quickly to avoid vision loss. We suggest regular checks and quick action to handle these problems well.
Cataracts in patients with anterior uveitis might need surgery. But, it’s key to control the inflammation first. For glaucoma, treatments or surgery might be needed to lower eye pressure.
Strategies for Preventing Flare-ups
Stopping flare-ups of anterior uveitis is key. We tell patients about lifestyle changes and sticking to their treatment. This means avoiding triggers and following their treatment plan closely.
Also, seeing your doctor regularly is important. It helps keep an eye on the condition and makes any needed changes. This way, patients can lower their chance of flare-ups and complications.
Understanding anterior uveitis and using a full management plan can help patients. It can also lower the risk of chronic anterior uveitis complications.
Conclusion
Understanding anterior uveitis is key to managing it well. It’s a type of eye inflammation that hits the uvea, the eye’s middle layer. We’ve looked at its different types, like acute and chronic, and granulomatous and non-granulomatous forms.
The reasons for anterior uveitis vary, from autoimmunity to infections. Finding out why it happens is vital for the right treatment. We talked about the need for a detailed check-up, including tests and scans.
Treatment for anterior uveitis includes eye drops and sometimes stronger medicines. It’s also important to handle any complications and stop it from coming back. This is all part of caring for patients with this condition.
Knowing about anterior uveitis and its causes helps doctors give better care. To manage it well, we need to tackle both the symptoms and the root causes. This way, we can offer complete care to our patients.
FAQ
What is anterior uveitis?
Anterior uveitis is a type of eye inflammation. It affects the front part of the eye, like the iris and ciliary body. Symptoms include eye pain, redness, and vision problems.
What are the symptoms of anterior uveitis?
Symptoms include eye pain, redness, and sensitivity to light. You might also see blurred vision or have trouble seeing clearly. These symptoms can get worse over time.
What causes anterior uveitis?
It can be caused by many things, like autoimmune diseases or infections. Sometimes, we don’t know what causes it, and it’s called idiopathic.
How is anterior uveitis diagnosed?
Doctors use a slit-lamp exam and lab tests to diagnose it. They also use imaging to see how bad the inflammation is.
What is the treatment for anterior uveitis?
Treatment includes eye drops to reduce inflammation. They might also use other medicines to help with pain and prevent complications. In some cases, they might need to use stronger treatments.
What are the complications of anterior uveitis?
If not treated well, it can cause serious problems. These include cataracts, glaucoma, and vision loss. It’s important to keep an eye on it and treat it properly.
Can anterior uveitis recur?
Yes, it can come back. The chance of it coming back depends on the cause and how well it was treated. To prevent it, managing any underlying conditions and following treatment plans is key.
Is anterior uveitis associated with other systemic conditions?
Yes, it can be linked to other diseases like ankylosing spondylitis and inflammatory bowel disease. Knowing this helps doctors take a more complete approach to treatment.
What is the role of genetics in anterior uveitis?
Genetics, like the HLA-B27 gene, play a big role in getting anterior uveitis. Other genes are also involved, showing how important genetics are in this condition.
How can anterior uveitis be managed long-term?
Long-term management means watching for complications and taking steps to prevent flare-ups. Treatment plans need to be adjusted as needed to keep the condition under control.
References
National Center for Biotechnology Information. Anterior Uveitis: Causes and Treatment Solutions. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2841369/