Radiation therapy is a key treatment for many cancers. It helps kill cancer cells and reduce tumors. At Liv Hospital, we know how vital this therapy is and its limits, like repeat sessions.
The treatment is painless but might cause skin discomfort over time. The main reason for repeat sessions limits is the cumulative dose to healthy tissues and organs. This can cause serious side effects.
Key Takeaways
- Radiation therapy is used to treat various cancers by killing cancer cells and shrinking tumors.
- The cumulative dose delivered to healthy tissues and organs limits repeat sessions.
- Careful planning is necessary to minimize side effects.
- Liv Hospital is committed to patient safety and innovative care.
- Repeat radiation therapy sessions require careful consideration of previous treatments.
Understanding Radiation Therapy Basics
Radiation therapy is a key tool in fighting cancer. It uses high-energy particles or waves to harm or kill cancer cells. This method targets the DNA of cancer cells, stopping them from growing and dividing.
What Radiation Therapy Does to Cancer Cells
Cancer cells grow and divide quickly. Radiation therapy damages their DNA, either by breaking DNA strands or creating free radicals. This damage stops cancer cells from making copies of themselves, leading to their death.
The success of radiation therapy varies based on the cancer type, location, and treatment start time. Different cancers react differently to radiation, with some being more sensitive.
Types of Radiation Treatment Modalities
There are two main types of radiation therapy: external beam radiation therapy (EBRT) and brachytherapy. External beam radiation therapy sends radiation from outside the body to the cancer. It’s the most common type, allowing for precise targeting of the radiation.
Brachytherapy places radioactive material inside or near the tumor. This method delivers high doses of radiation to the tumor while protecting healthy tissues nearby.
The choice between these options depends on the tumor type, location, and patient factors. Knowing these basics helps patients make better treatment choices.
Standard Radiation Treatment Protocols
It’s important for patients to know about radiation treatment protocols. These plans help make treatment work best and reduce side effects.
Typical Number of Sessions for Different Cancers
The number of radiation sessions changes based on the cancer type and stage. For instance, breast cancer patients might get treatment for weeks. On the other hand, head and neck cancer patients might need a more intense treatment.
| Type of Cancer | Typical Number of Sessions | Duration of Treatment |
| Breast Cancer | 15-25 | 3-5 weeks |
| Prostate Cancer | 20-40 | 4-8 weeks |
| Head and Neck Cancer | 30-35 | 6-7 weeks |
How Treatment Plans Are Determined
Treatment plans depend on many things. These include the tumor’s type, size, and where it is. The patient’s health is also a big factor. Individual tolerance to radiation is very important too.
Healthcare experts use these details to create a treatment plan. They aim to make it effective while keeping side effects low.
Can You Get Radiation Treatment More Than Once?
Many cancer patients wonder if they can get radiation therapy more than once. The decision to repeat treatment depends on several things. These include the type and location of the tumor, the patient’s health, and the dose to healthy tissues.
Scenarios Where Multiple Courses Are Considered
There are specific situations where more than one round of radiation therapy is considered. This includes new primary cancers and local or regional recurrences. Each case is looked at carefully.
We consider how long it’s been, the dose given before, and the benefits of more treatment. Our goal is to help the patient as much as possible while keeping risks low.
Re-irradiation for Recurrent Disease
Deciding on re-irradiation for recurrent disease is complex. We look at the location and size of the recurrence, the dose given before, and the patient’s health.
The table below shows important things to consider for re-irradiation:
| Factor | Consideration |
| Tumor Location | Proximity to critical structures |
| Previous Radiation Dose | Cumulative dose to healthy tissues |
| Time Elapsed | Recovery of normal tissues |
Re-irradiation can be a good option for some patients with recurrent disease. But, we must think about the risks of more side effects and toxicity.
Key Considerations for Re-Irradiation
- Assessment of tumor biology and aggressiveness
- Evaluation of normal tissue tolerance
- Use of advanced radiation techniques to minimize exposure to healthy tissues
By looking at these factors, we can decide if re-irradiation is right. We then create a treatment plan that is safe and effective for each patient.
Biological Limitations of Radiation Exposure
It’s key to know how radiation affects living things to decide if more treatments are safe. Radiation harms both healthy and cancer cells in the treated area. This means we have to watch how much radiation healthy tissues get.
Cumulative Dose Concerns for Healthy Tissues
The total amount of radiation given is a big deal in therapy. Healthy tissues can only handle so much radiation before it becomes toxic. We need to plan therapy carefully to protect healthy areas.
Radiation toxicity can show up in many ways, based on where and how much radiation is used. Symptoms can be mild or severe, like tiredness, skin issues, or organ damage. The chance of lasting side effects grows with higher doses.
Tissue Recovery Between Treatment Courses
How well tissues bounce back between treatments is also important. Recovery times vary based on the tissue, dose, and time between treatments. Some heal fast, others take longer or might not recover fully.
We think about these points when deciding on more treatments. It’s vital to plan and watch closely to make sure the benefits of therapy are worth the risks. Knowing how radiation affects living things helps us care for patients better and improve treatment results.
Factors That Determine Maximum Radiation Exposure
It’s key to know what affects how much radiation a patient can safely get. The dose depends on the tumor’s type and where it is, the patient’s health, and past treatments.
Tumor Type and Location Considerations
The tumor’s type and where it is matter a lot. Tumors near important organs need special care to avoid harm. For example, tumors in the head and neck must be treated carefully to protect nearby tissues.
Individual Patient Tolerance Factors
How well a patient can handle radiation changes with age, health, and genetics. Younger people might handle more radiation than older ones, whose bodies are more sensitive.
Prior Treatment History Impact
What treatments a patient has had before affects how much more radiation they can take. Patients who’ve had radiation before might not be able to handle as much. We look at their history to plan the safest treatment.
| Factor | Influence on Maximum Radiation Exposure | Clinical Considerations |
| Tumor Type | Affects radiation sensitivity and required dose | Different tumors have varying radiosensitivities |
| Tumor Location | Impacts ability to spare surrounding critical structures | Proximity to vital organs dictates treatment planning |
| Patient Age and Health | Influences tissue tolerance and recovery | Older or less healthy patients may require dose adjustments |
| Prior Radiation Therapy | Determines cumulative dose and possible for re-irradiation | Previous radiation exposure limits future treatment options |
Advanced Techniques Enabling Multiple Radiation Treatments
Radiation therapy has evolved with new methods for repeated treatments. These advancements have greatly improved patient care. They make it possible to treat tumors more precisely and effectively.
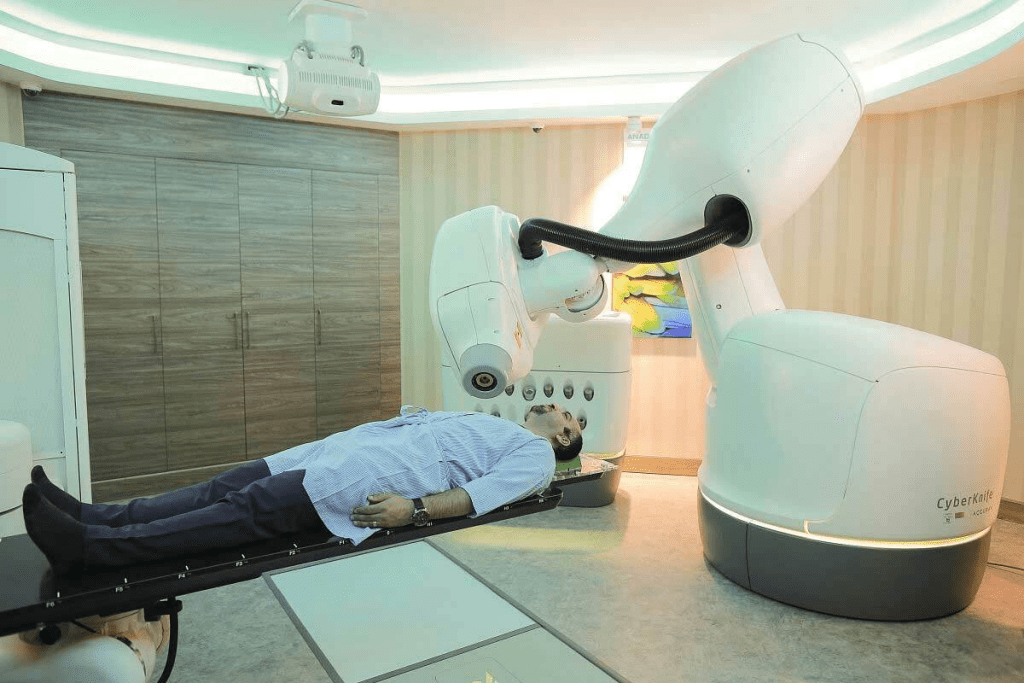
Stereotactic Body Radiotherapy
Stereotactic Body Radiotherapy (SBRT) is a precise radiation therapy. It targets tumors with high accuracy. Recent studies have shown that SBRT is safe and effective for patients with multiple.
SBRT uses advanced imaging and delivery systems. This allows for treating multiple lesions without harming healthy tissues. The benefits of SBRT include:
- High precision: Accurate targeting of tumors
- Minimal side effects: Reduced damage to healthy tissues
- Effective treatment: High success rates for tumor control
High-Precision Methods for Treating Multiple Lesions
High-precision radiation therapy has changed how we treat multiple lesions. These methods allow for treating several tumors at once. They also protect healthy tissues nearby.
One big plus of these methods is treating patients with widespread cancer. Studies have shown the safety and success of these treatments for widespread. The benefits include:
- Improved patient outcomes: Better survival rates and quality of life
- Reduced treatment time: Treating multiple lesions in fewer sessions
- Increased precision: Less risk to healthy tissues
These advanced techniques help healthcare providers offer better care. They improve treatment options for complex cases, leading to better care and patient satisfaction.
Risks and Side Effects of Repeated Radiation Therapy
Repeated radiation therapy is a common treatment for many patients. But, it also has risks and side effects to think about. Knowing these risks is key to making good treatment choices.
Short-Term Side Effects of Multiple Courses
Patients getting multiple radiation treatments may face short-term side effects. These can include fatigue, skin reactions like redness, and stomach problems like nausea. How bad these side effects are can depend on where the treatment is and the patient’s health.
| Side Effect | Description | Management Strategies |
| Fatigue | Feeling tired or lacking energy | Rest, exercise, nutrition counseling |
| Skin Reactions | Redness, irritation, or dryness of the skin | Topical creams, avoiding harsh soaps |
| Gastrointestinal Issues | Nausea, diarrhea, or loss of appetite | Dietary adjustments, anti-nausea medication |
Long-Term Risks to Surrounding Tissues
Repeated radiation therapy can harm tissues around the treated area. Cumulative radiation exposure can cause scarring and damage. This can lead to long-term health problems that affect daily life.
Quality of Life Considerations
It’s important to manage side effects of repeated radiation therapy to keep quality of life good. This includes medical care and support like counseling and nutrition help. Healthcare teams work to help patients deal with these challenges.
Choosing to have repeated radiation therapy should be well thought out. Patients should talk to their healthcare team to understand the risks and benefits. This way, they can make choices that fit their treatment goals and values.
Combining Chemotherapy with Radiation Therapy
Chemotherapy and radiation therapy are often used together to fight cancer better. This method helps us hit cancer cells harder, leading to better results for patients.
Concurrent Administration Approaches
When we give chemotherapy and radiation therapy at the same time, it’s called concurrent administration. This makes radiation therapy work better by making cancer cells more sensitive to it. Studies have shown that this method can lead to better control of cancer and longer life for many patients.
A study by UCLA Health found that high-dose radiotherapy with chemotherapy is effective against some cancers.
- Chemotherapy can make radiation therapy more effective.
- Doing both treatments at the same time can increase success rates.
- It’s important to plan carefully to avoid too many side effects.
Sequential Treatment Strategies
Sequential treatment means giving chemotherapy and radiation therapy one after the other. This method helps protect healthy tissues and reduces side effects.
Sequential treatment is used when cancer is spread out or when a patient’s health is a concern. By planning the order of treatments, doctors can make sure the treatment works well while keeping risks low.
- First, chemotherapy is used to shrink the tumor.
- Then, radiation therapy targets any remaining cancer cells.
- Doctors keep checking to see if the treatment needs to change.
By mixing chemotherapy with radiation therapy, we can create treatment plans that fit each patient’s needs. This approach is key in modern cancer care, bringing hope and better results to patients all over the world.
Time Intervals Between Radiation Treatments
The time between radiation therapy sessions is key to success and fewer side effects. When thinking about radiation therapy, the timing between sessions matters a lot. It affects how well the treatment works and how well the patient feels.
Minimum Safe Waiting Periods for Re-treatment
Finding the right time for re-treatment depends on many things. These include the tumor’s type and location, the first radiation dose, and the patient’s health. Oncologists look at these factors to decide when to start re-treatment. They aim to give healthy tissues time to heal while hitting cancer cells hard.
Re-treatment plans change based on the patient’s situation. For example, some areas might need longer breaks to avoid problems. We work with patients to make a treatment plan that fits their needs.
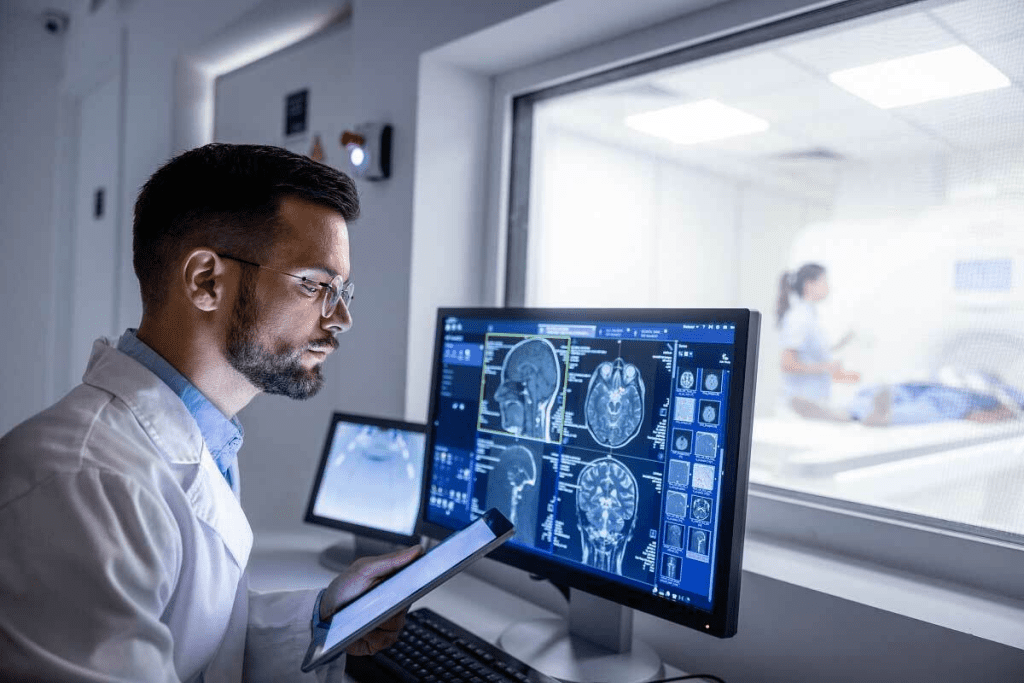
How Oncologists Track Cumulative Radiation Exposure
Keeping an eye on total radiation dose is very important. Oncologists use special systems to track doses to the tumor and healthy tissues. This careful tracking helps us adjust plans to lower risks.
When thinking about re-treatment, looking at total radiation dose is key. We analyze how the patient reacted to previous treatments to decide on the next steps.
Managing radiation therapy well means careful planning and monitoring. Understanding the importance of time gaps and tracking total dose helps us improve treatment results and care for patients.
Conclusion: Making Informed Decisions About Radiation Therapy
Radiation therapy is a complex treatment that needs careful planning. It involves looking at the dose to healthy tissues and organs. Knowing the limits and risks is key for patients to choose wisely.
We’ve looked at the different types of radiation therapy and standard protocols. We’ve also talked about what affects the maximum dose. This helps patients understand their treatment and its risks better.
Choosing the right radiation therapy means knowing all your options and the dose involved. We urge patients to talk to their doctors about their plans. This way, they can get the best care for their needs.
FAQ
Can you have radiation therapy more than once?
Yes, you can have radiation therapy more than once. It depends on several things. These include the type and location of the tumor, the dose of radiation you’ve had before, and your overall health.
Why can’t you have radiation twice?
While you can have radiation therapy again, there are limits. The main concern is the dose to healthy tissues and organs. Doctors consider each case carefully to avoid harm.
What is the maximum number of radiation treatments?
There’s no set limit on the number of radiation treatments. It varies based on your cancer type and stage, and how well you can handle treatment.
How often do you get radiation treatments?
Radiation treatments usually happen daily, from Monday to Friday, for weeks. The exact schedule depends on your treatment plan.
Can you do chemo and radiation at the same time?
Yes, you can get chemotherapy and radiation therapy at the same time. It depends on your cancer type and stage, and what your doctors aim to achieve.
What is the cumulative dose of radiation?
The cumulative dose is the total radiation you’ve received over time. It’s key in assessing the risk of side effects and deciding if you can have more radiation.
How do oncologists track cumulative radiation exposure?
Oncologists track your radiation exposure by looking at your past treatments, imaging, and dosimetry data. This helps them understand your total radiation dose.
What are the risks of repeated radiation therapy?
Repeated radiation therapy can harm healthy tissues and increase the risk of side effects. These can include fibrosis and secondary cancers.
Can you have radiotherapy more than once for recurrent disease?
Yes, you can have radiation therapy again for recurring disease. But, it’s only considered if the risks are low enough and the benefits are high.
How are treatment plans determined for radiation therapy?
A team of doctors plans your radiation therapy. They consider your cancer type and stage, your health, and what you hope to achieve from treatment.
What is stereotactic body radiotherapy (SBRT)?
SBRT is a focused radiation therapy. It delivers high doses to small, precise tumors in a few sessions.
Can chemotherapy and radiation therapy be given concurrently?
Yes, chemotherapy and radiation therapy can be given together. This can make treatment more effective but also raises the risk of side effects.
References
- Noël, G., et al. (2024). Tumor reirradiation: Issues, challenges and perspectives. Radiotherapy and Oncology.https://www.sciencedirect.com/science/article/pii/S1278321824001264
- Yuan, J., et al. (2018). Cumulative doses to brain and other critical structures during stereotactic radiosurgery. PMC.https://pmc.ncbi.nlm.nih.gov/articles/PMC5859351/