Last Updated on November 25, 2025 by Ugurkan Demir
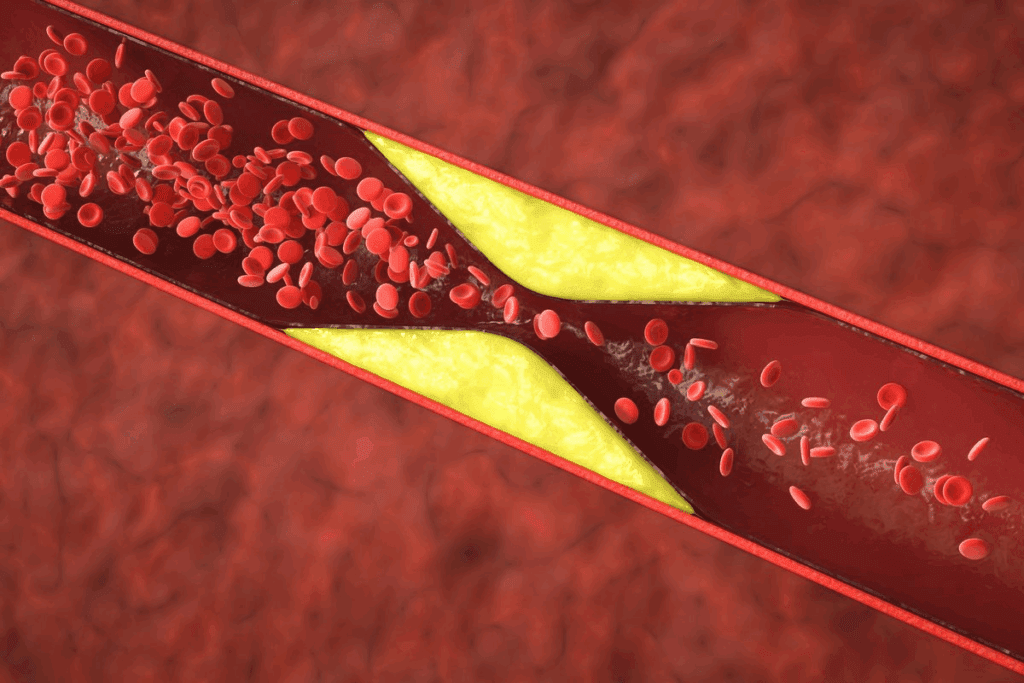
At Liv Hospital, we know that low or normal cholesterol doesn’t mean your arteries are safe. Atherosclerosis, or plaque buildup in arteries, is caused by more than just cholesterol. Other factors play a big role too.Discover if you can you have clogged arteries with low cholesterol and why it happens.
High blood pressure, genetics, diabetes, obesity, and lifestyle choices all affect artery health. A study in the Journal of the American College of Cardiology found nearly half of heart attacks in women under 65 were caused by non-traditional factors. This shows how complex heart disease can be.
We believe in a detailed check-up to find heart risks, even with normal cholesterol. Our focus on advanced, patient-focused cardiac care means you get a thorough check and the right treatment.
Key Takeaways
- Low or normal cholesterol levels do not guarantee clear arteries.
- Various factors contribute to atherosclerosis, including high blood pressure and genetics.
- Heart disease can be caused by non-traditional factors.
- A thorough evaluation is key to spotting heart risks.
- Liv Hospital offers top-notch, patient-centered cardiac care.
The Cholesterol-Plaque Paradox
New research is uncovering the complex link between cholesterol and plaque in arteries. For years, high cholesterol was seen as a major heart disease risk. Yet, many with normal or low cholesterol levels can get clogged arteries, causing heart problems.
The Conventional Wisdom About Cholesterol and Heart Disease
Traditionally, high levels of LDL cholesterol, or “bad” cholesterol, were thought to cause artery plaque. This idea has shaped how doctors treat heart disease, focusing on lowering LDL. Dr. Steven Nissen, a cardiologist at the Medical organization, noted, “The focus on LDL cholesterol has been a cornerstone of cardiovascular risk reduction strategies.”
“The focus on LDL cholesterol has been a cornerstone of cardiovascular risk reduction strategies.” – Dr. Steven Nissen, Medical organization
The Surprising Reality: When Numbers Don’t Tell the Full Story
Recent studies show that cholesterol and plaque are more connected than we thought. Plaque is made of fat, cholesterol, calcium, and waste, influenced by many factors. Inflammation, oxidative stress, and metabolic processes also play big roles in atherosclerosis.
Exploring the cholesterol-plaque paradox shows that cholesterol levels alone don’t tell the whole story. This highlights the need for a broader approach to heart health.
Understanding Atherosclerosis Beyond Cholesterol
To really get atherosclerosis, we need to look at how plaque builds up. Atherosclerosis makes arteries narrow and hard because of plaque buildup. This plaque is a mix of different things.
It’s not just about cholesterol. Other factors like inflammation, genes, and lifestyle play big roles. Knowing these helps us fight atherosclerosis better.
What Really Happens During Plaque Formation
Plaque starts with damage to the artery’s inside. High blood pressure, smoking, or certain blood lipids can cause this damage.
When the artery is damaged, platelets and blood parts stick to it. This starts inflammation. Over time, more plaque builds up, narrowing the artery and blocking blood flow.
The Complex Composition of Arterial Plaque
Arterial plaque is more than just cholesterol. It’s a mix of:
- Lipids (including cholesterol)
- Inflammatory cells
- Smooth muscle cells
- Connective tissue
- Calcium deposits
Each person’s plaque is different. This makes every case of atherosclerosis unique.
| Component | Description | Role in Plaque Formation |
| Lipids | Includes cholesterol and triglycerides | Major contributor to plaque volume |
| Inflammatory Cells | Cells that promote inflammation | Contributes to plaque instability |
| Smooth Muscle Cells | Cells that make up the arterial wall | Proliferate in response to injury |
| Calcium Deposits | Mineral deposits that harden plaque | Contributes to plaque hardening |
Knowing what’s in arterial plaque helps us treat it better. By seeing atherosclerosis as a complex issue, doctors can give more tailored care.
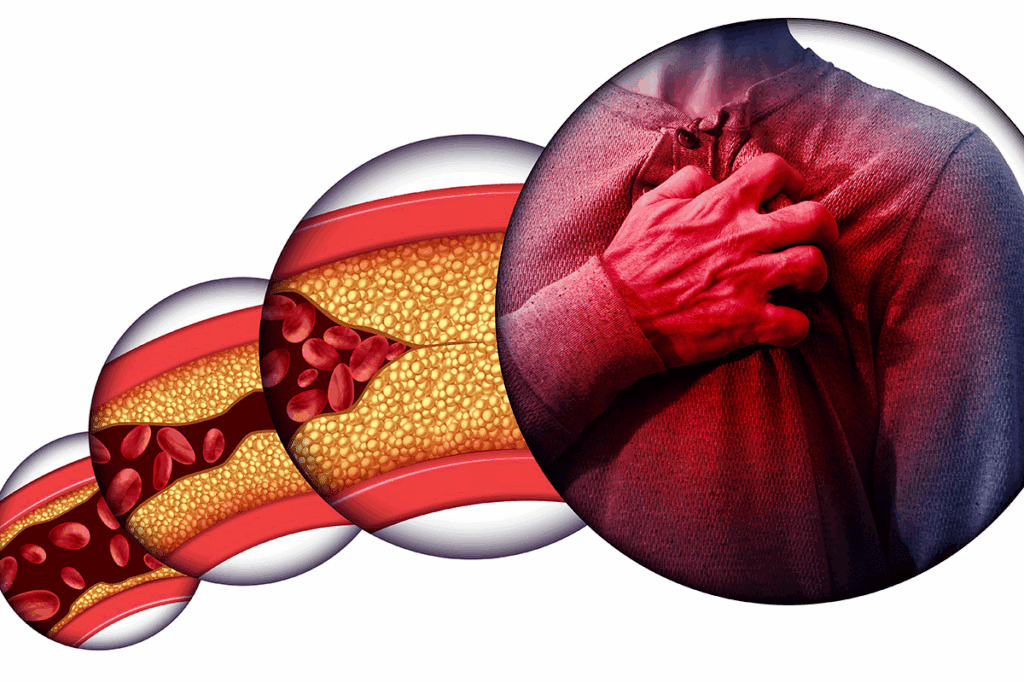
Can You Have Clogged Arteries With Low Cholesterol?
Many think low cholesterol means clear arteries. But, it’s not that simple. Even with low cholesterol, arteries can get clogged. This shows how complex heart health is and the need to understand more about what causes plaque buildup.
Research Evidence and Clinical Observations
Studies have looked into cholesterol and heart disease. High cholesterol is a known risk, but heart attacks happen in people with normal or low cholesterol too. For example, a study in the Journal of the American College of Cardiology found that many heart attacks in women under 65 were not caused by cholesterol.
Doctors have also seen patients with good cholesterol levels get heart disease. This shows other factors, not just cholesterol, are important in heart health.
Case Studies: Heart Attacks in Patients With Optimal Lipid Profiles
There are stories of people with low cholesterol getting heart attacks. For instance, a patient in the New England Journal of Medicine had low LDL cholesterol but had a heart attack. These stories show low cholesterol doesn’t always mean you’re safe from heart problems.
These stories stress the need to look at all risk factors, not just cholesterol. They also show we need better tests to find hidden risks that traditional tests miss.
Why Traditional Risk Assessment May Fall Short
Traditional risk checks focus on cholesterol, blood pressure, and other known risks. But, they might miss other important factors. New research points to inflammation, genetics, and metabolic issues as key players in heart disease.
Healthcare providers should use a broader approach to check heart risks. This could include new tests and imaging to find people at risk, even if their cholesterol is low.
The Role of Inflammation in Arterial Damage
Understanding inflammation’s role in artery health is key to avoiding heart disease. Inflammation is a complex response that affects atherosclerosis development and growth.
How Inflammation Initiates and Accelerates Plaque Formation
Inflammation starts plaque buildup by damaging artery walls. This makes them more likely to collect lipids and other substances. Factors like high blood pressure, smoking, and high cholesterol often trigger this.
As inflammation grows, it speeds up plaque buildup. It does this by attracting more platelets and inflammatory cells. This creates a cycle that quickly worsens atherosclerosis.
Inflammatory Markers as Predictors of Heart Disease
Studies have found certain markers that signal heart disease risk. These include C-reactive protein (CRP), interleukin-6 (IL-6), and tumor necrosis factor-alpha (TNF-alpha). High levels of these markers show chronic inflammation, raising heart event risk.
| Inflammatory Marker | Association with Heart Disease |
| C-reactive protein (CRP) | Predicts cardiovascular events and mortality |
| Interleukin-6 (IL-6) | Indicates chronic inflammation and cardiovascular risk |
| Tumor Necrosis Factor-alpha (TNF-alpha) | Involved in systemic inflammation and atherosclerosis |
The Connection Between Chronic Inflammation and Arterial Health
Chronic inflammation deeply affects artery health, leading to atherosclerosis. It’s vital to manage chronic inflammation through lifestyle changes and treatments. This helps keep arteries healthy and lowers heart disease risk.
Dealing with inflammation needs a full approach. This includes diet changes, exercise, stress management, and possibly anti-inflammatory drugs. By grasping inflammation’s role in artery damage, we can create effective ways to lessen its effects and improve heart health.
High Blood Pressure But Low Cholesterol: A Dangerous Combination
Hypertension is a big worry for heart health, even with low cholesterol. High blood pressure can harm arterial walls, leading to plaque and heart risks.
Damage to Arterial Walls
High blood pressure puts too much pressure on arterial walls, causing damage. This damage can lead to plaque formation and narrowed arteries.
This damage affects more than just the walls. It also impacts the heart, making it work harder. This can lead to heart enlargement and more problems.
Synergistic Effect of Multiple Risk Factors
Having multiple risk factors can greatly harm cardiovascular health. For example, high blood pressure with smoking or diabetes raises heart risks a lot.
| Risk Factor | Impact on Cardiovascular Health |
| High Blood Pressure | Damages arterial walls, increases risk of plaque formation |
| Smoking | Increases oxidative stress, damages blood vessels |
| Diabetes | Damages blood vessels, increases risk of cardiovascular events |
Blood Pressure Management for Arterial Health
Keeping blood pressure in check is key for artery health. This can be done through lifestyle changes and, if needed, medication.
Healthy eating, regular exercise, and a good weight can help manage blood pressure. Stress reduction through meditation or yoga also helps.
For those with hypertension, it’s important to monitor blood pressure and follow treatment plans. This can greatly reduce heart risks and keep cardiovascular health good.
Genetic Factors That Influence Arterial Health
Understanding the genetic factors that affect arterial health is key to assessing cardiovascular risk. Our genes play a big role in how likely we are to get atherosclerosis and other diseases of the arteries.
Hereditary Predispositions to Atherosclerosis
Studies show that people with a family history of heart disease are more at risk for atherosclerosis. This is because they inherit certain genes that affect how their body handles fats, inflammation, and blood vessel function.
For example, some genes can cause high levels of LDL cholesterol, known as “bad” cholesterol. Others can make the lining of blood vessels more prone to damage and plaque buildup.
Genetic Variations That Affect Plaque Formation
Many genetic variations have been found to impact plaque formation in arteries. These include genes involved in fat metabolism, like APOE and LDLR, and those that affect inflammation.
| Gene | Function | Impact on Arterial Health |
| APOE | Lipid metabolism | Influences LDL cholesterol levels |
| LDLR | LDL cholesterol receptor | Affects clearance of LDL cholesterol |
| PCSK9 | LDLR degradation | Regulates LDL cholesterol levels |
Family History as a Non-Modifiable Risk Factor
While lifestyle changes can help, family history is a risk factor we can’t change. Knowing your family history helps assess your risk and may lead to more aggressive prevention or earlier treatment.
Early screening and preventive care are vital for those with a strong family history of heart disease. This might include regular health checks, lifestyle changes, and possibly medication to manage risk factors.
Metabolic Disorders and Arterial Plaque
It’s important to know how metabolic disorders like diabetes and insulin resistance affect our blood vessels. These conditions can lead to the buildup of arterial plaque, which is a major risk for heart disease.
Diabetes and Its Impact on Vascular Health
Diabetes is a big risk factor for heart disease. High blood sugar can damage blood vessel linings, making them more likely to develop plaque. Research shows that people with diabetes are more likely to get atherosclerosis, a condition where plaque builds up in arteries.
High blood sugar causes oxidative stress and inflammation, which are key in forming plaque. Diabetes often comes with other heart disease risk factors like high blood pressure and bad cholesterol levels. This makes the risk of damage to blood vessels even higher.
Insulin Resistance and Arterial Damage
Insulin resistance, which can lead to type 2 diabetes, also raises the risk of heart disease. It happens when the body can’t use insulin well, leading to high insulin levels and metabolic problems. This condition increases inflammation and oxidative stress, which help plaque form in arteries.
| Condition | Impact on Arterial Health | Associated Risks |
| Diabetes | Damages inner lining of blood vessels | Atherosclerosis, Cardiovascular Disease |
| Insulin Resistance | Increases inflammation and oxidative stress | Type 2 Diabetes, Cardiovascular Disease |
| Metabolic Syndrome | Combination of insulin resistance, hypertension, and dyslipidemia | Significantly increased risk of Cardiovascular Disease |
Metabolic Syndrome: A Perfect Storm for Atherosclerosis
Metabolic syndrome is a group of conditions that raise the risk of heart disease and type 2 diabetes. It includes insulin resistance, high blood pressure, and bad cholesterol levels. Having metabolic syndrome is like a perfect storm for atherosclerosis, combining many risk factors that harm blood vessels.
Understanding how metabolic disorders affect our blood vessels helps us spot those at risk. We can then take steps to lower their heart disease risk.
Lifestyle Factors That Contribute to Arterial Plaque
Knowing what lifestyle factors lead to arterial plaque is key to keeping your heart healthy. Our daily habits greatly affect our artery health. Making smart choices can lower the risk of plaque buildup.
Dietary Patterns Beyond Cholesterol Intake
Diet is very important for artery health. It’s not just about cholesterol. Foods high in processed items, sugars, and fats can cause inflammation and stress. These are big factors in plaque formation.
Eating a balanced diet with lots of fruits, veggies, whole grains, and lean proteins is good. Foods like salmon and walnuts, rich in omega-3s, help protect your heart.
| Dietary Component | Effect on Arterial Health |
| High Processed Foods | Increases risk of plaque formation |
| High Fruits and Vegetables | Supports healthy arteries |
| Omega-3 Rich Foods | Protects against heart disease |
Physical Inactivity and Vascular Function
Regular exercise is vital for artery health. It boosts blood flow, lowers blood pressure, and cuts down inflammation. All these help lower the risk of plaque.
Being inactive, though, raises the risk of heart disease. Long periods without moving can harm artery function and lead to more plaque.
Smoking and Oxidative Stress in Blood Vessels
Smoking is a big risk for plaque buildup. It damages blood vessel linings, boosts oxidative stress, and causes inflammation. All these speed up plaque growth.
Quitting smoking greatly lowers heart disease risk and slows plaque growth. Staying away from secondhand smoke is also important for artery health.
By changing these lifestyle habits, you can lower your risk of plaque and improve heart health.
Advanced Testing for Hidden Cardiovascular Risks
Our understanding of heart disease is growing, and so is the tech to find its early signs. New tests can spot hidden heart risks that simple lipid panels can’t.
Beyond Standard Lipid Panels
Lipid panels check total cholesterol, LDL, HDL, and triglycerides. But they don’t show the whole picture of heart risk. Advanced tests give deeper insights into cholesterol types and other lipid factors.
For example, LDL particle number (LDL-P) and apolipoprotein B (ApoB) tests give a clearer risk picture than LDL cholesterol alone. They help find people with higher or lower risk than their LDL cholesterol suggests.
Imaging Tests That Detect Early Plaque Formation
Imaging tests are key in spotting early heart disease signs. The Coronary Artery Calcium (CAC) scan measures artery calcium. A high score means more plaque and higher heart risk.
Carotid Intima-Media Thickness (CIMT) ultrasound also plays a role. It checks artery wall thickness. Thicker walls mean higher risk of heart attack and stroke.
| Imaging Test | What It Measures | Clinical Significance |
| Coronary Artery Calcium (CAC) Scan | Amount of calcium in coronary arteries | Indicates burden of coronary artery plaque and risk of future cardiovascular events |
| Carotid Intima-Media Thickness (CIMT) Ultrasound | Thickness of carotid artery walls | Associated with risk of myocardial infarction and stroke |
Specialized Blood Tests for Cardiovascular Risk Assessment
There are blood tests beyond lipid profiles that help assess heart risk. High-sensitivity C-reactive protein (hs-CRP) tests show inflammation levels. High levels mean higher heart event risk.
Lipoprotein(a) [Lp(a)] tests check a genetic LDL variant linked to heart risk. Homocysteine tests measure an amino acid linked to atherosclerosis risk.
| Blood Test | What It Measures | Clinical Significance |
| High-sensitivity C-reactive Protein (hs-CRP) | Level of inflammation | Associated with increased risk of cardiovascular events |
| Lipoprotein(a) [Lp(a)] | Genetic variant of LDL cholesterol | Associated with increased cardiovascular risk |
| Homocysteine | Level of homocysteine amino acid | Linked to higher risk of atherosclerotic disease when elevated |
Conclusion: A Comprehensive Approach to Arterial Health
Keeping your arteries healthy is more than just checking your cholesterol. We’ve seen how things like inflammation, genes, metabolic issues, and lifestyle play big roles. Even if your cholesterol looks good, these factors can lead to atherosclerosis.
To fight cardiovascular risk, we need a big plan. This includes making lifestyle changes, managing risk factors, and using new testing methods. Eating right, staying active, and not smoking can greatly lower your heart disease risk.
We stress the need for a proactive stance on artery health. It’s key to work with your doctor to check and manage your heart risk. This way, we can cut down heart disease and improve overall health.
FAQ
Can you have clogged arteries with normal cholesterol levels?
Yes, it’s possible to have clogged arteries even with normal cholesterol. Other factors like inflammation, high blood pressure, and metabolic disorders can cause plaque buildup.
How does inflammation affect arterial health?
Inflammation can start and speed up plaque formation. It damages arterial walls and raises heart disease risk. Inflammatory markers help predict cardiovascular risk.
What is the relationship between high blood pressure and clogged arteries?
High blood pressure can harm arterial walls, making them more prone to plaque. Keeping blood pressure in check is key for artery health.
Can genetic factors influence the risk of clogged arteries?
Yes, genetics can play a role in plaque formation and atherosclerosis risk. Family history is a non-modifiable risk factor.
How do metabolic disorders impact vascular health?
Metabolic disorders like diabetes and insulin resistance can damage blood vessels. They contribute to arterial plaque formation.
What lifestyle factors contribute to the formation of arterial plaque?
Lifestyle choices like diet, lack of exercise, and smoking can lead to clogged arteries. Changing these habits can lower cardiovascular risk.
Are standard lipid panels enough to assess cardiovascular risk?
No, standard lipid panels don’t fully show cardiovascular risk. Advanced tests like imaging and specialized blood tests can reveal hidden risks.
Can you have normal blood pressure and yet have clogged arteries?
Yes, normal blood pressure doesn’t rule out clogged arteries. Other factors like high cholesterol, smoking, and metabolic disorders can cause plaque.
How does cholesterol contribute to the formation of arterial plaque?
Cholesterol is one factor in plaque formation. The process involves inflammation and damage to arterial walls.
What is the average cholesterol level of heart attack victims?
Many heart attack victims have normal cholesterol levels. This shows the importance of looking at other risk factors.
Can plaque formation be reversed or slowed down?
Yes, managing risk factors like high blood pressure and cholesterol, and living a healthy lifestyle can slow or reverse plaque formation.
References:
- Ruel, M. (2024). Coronary artery bypass grafting: Past and future. Circulation, 150(10), 763-766. https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.124.068312





