Understanding cancer in situ is key for early treatment and better patient care. We aim to give our patients the best care and support. The cancer in situ meaning explained: a non-invasive cancer that is confined to the original layer of cells and has not broken through the basement membrane.
Cancer in situ, or CIS, means abnormal cells that haven’t spread. It’s the first stage of cancer, where cells stay in their original place.
At Liv Hospital, we focus on patient care. We use detailed diagnostics and proven treatments. These can often cure cancer in situ before it gets worse.

Grasping the basics of cancer in situ is key. It’s a condition where cancer cells are present but haven’t spread. This is often shortened to CIS.
The term ‘in situ’ comes from Latin, meaning ‘in its place.’ It describes cells that stay in one place, within epithelial tissues. They haven’t invaded deeper or surrounding tissues. This stage is important because it means the cancer is contained and can be cured if treated right.
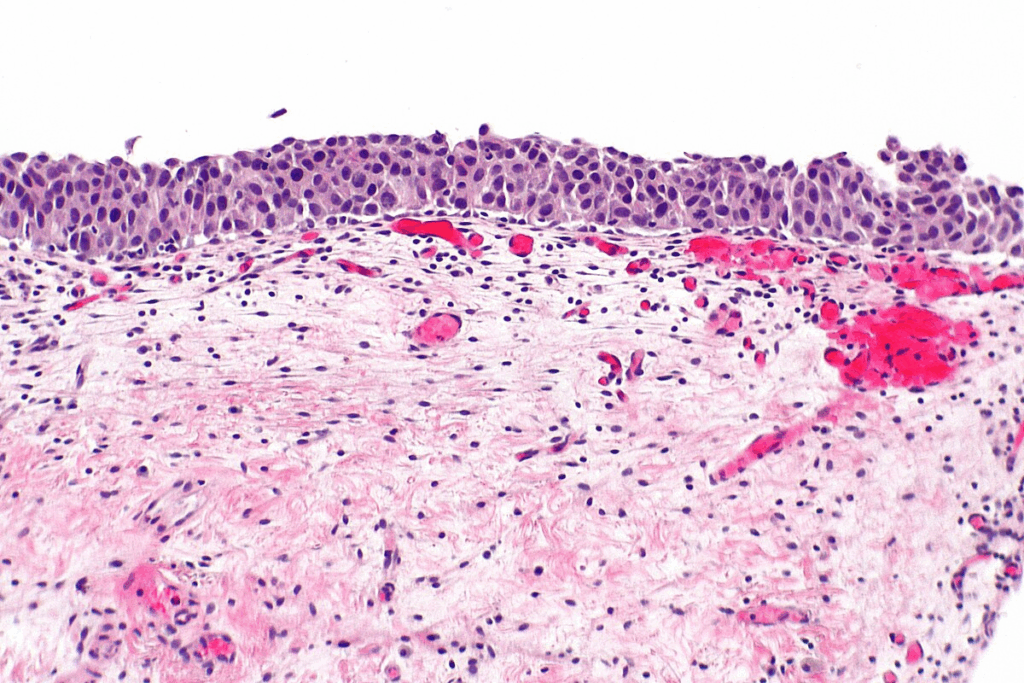
Cancer in situ is different from invasive cancer because it stays in one place. CIS hasn’t broken through the basement membrane. This means it hasn’t invaded deeper tissues or spread to other parts of the body. Knowing this is key for figuring out the cancer’s stage and treatment.
The main distinguishing features are:
Cancer in situ is an early stage and is often treatable. It’s vital for both patients and healthcare providers to understand it. This knowledge helps in making informed decisions about diagnosis, treatment, and management.

It’s important to understand the biology of cancer in situ to grasp its role in cancer diagnosis. Cancer in situ, or carcinoma in situ, is when cancer cells are present but haven’t spread to healthy tissues. These cells are different from normal cells, and knowing how they differ is key to treating cancer in situ.
Cancer cells are different from normal cells in many ways. In cancer in situ, cells show specific traits, such as:
These traits are important for spotting cancer in situ under a microscope.
Under a microscope, cancer in situ cells look different from normal cells and invasive cancer cells. The key features include:
Pathologists look at tissue samples to find these signs, which are vital for diagnosing cancer in situ.
Genetic and Molecular Features
Cancer in situ also has specific genetic and molecular changes. These include:
Knowing these genetic and molecular changes helps in creating targeted treatments. This improves outcomes for patients with cancer in situ.
Cancer in situ, or carcinoma in situ, is called Stage 0 cancer. It’s the earliest stage of cancer. In this stage, abnormal cells stay in their original place without spreading to other tissues.
To understand why cancer in situ is Stage 0, we look at the TNM staging system. This system helps figure out how far cancer has spread.
The TNM system has three parts: T (Tumor size and extent), N (lymph node involvement), and M (metastasis). For cancer in situ, the T category is “Tis.” This means the tumor is in situ and hasn’t spread to other tissues.
| TNM Component | Description for Cancer in Situ |
| T (Tumor) | Tis – Tumor in situ, non-invasive |
| N (Node) | N0 – No regional lymph nodes involvement |
| M (Metastasis) | M0 – No distant metastasis |
Cancer in situ is pre-invasive because it hasn’t spread to other tissues or parts of the body. This stage is key for early treatment before it becomes invasive.
Early detection of cancer in situ is key. It allows for early treatment, which can stop it from becoming invasive cancer. Screening and tests are important for finding cancer early.
Knowing about cancer in situ as Stage 0 cancer helps doctors and patients make better treatment plans.
Carcinoma in situ, or stage 0 cancer, includes different forms based on where and what type of cells are affected. These types are non-invasive, meaning the abnormal cells haven’t spread. Knowing about these types is key for the right treatment.
Ductal carcinoma in situ (DCIS) is when abnormal cells are in the breast’s milk ducts. It’s non-invasive because the cells haven’t spread. DCIS is often found during mammograms and can be treated well if caught early.
Lobular carcinoma in situ (LCIS) is abnormal cell growth in the breast’s lobules. Unlike DCIS, LCIS is not a true cancer but a sign of higher breast cancer risk.
Important aspects of LCIS:
Cervical carcinoma in situ, also known as cervical intraepithelial neoplasia (CIN), is abnormal cells on the cervix’s surface that haven’t become invasive. Regular Pap smears can find these cells early, allowing for quick action.
| Stage | Description |
| CIN 1 | Mild dysplasia |
| CIN 2 | Moderate dysplasia |
| CIN 3 | Severe dysplasia or carcinoma in situ |
Squamous cell carcinoma in situ happens when abnormal squamous cells are found on the skin or mucous membranes, like in the mouth. If not treated, it can turn into invasive cancer.
Early detection and treatment of these common types of carcinoma in situ are critical for preventing invasive cancer and improving patient outcomes.
Less common types of cancer in situ, like melanoma in situ, bring unique challenges and chances for early treatment. While many know about ductal carcinoma in situ (DCIS) of the breast, others are less known but just as important. It’s key to understand these types to fully grasp carcinoma in situ and its many forms.
Melanoma in situ, or stage 0 melanoma, is when cancer cells stay in the skin’s outer layer without spreading. It’s very treatable if caught early. Doctors diagnose it through a biopsy, checking skin cells for any odd changes.
Vulvar intraepithelial neoplasia (VIN) is when abnormal cells on the vulva might turn into cancer. It’s a sign of cancer coming and often linked to HPV. Catching it early through regular check-ups is key to managing it well.
Penile intraepithelial neoplasia (PeIN) is abnormal cell growth on the penis that could become invasive cancer. Like VIN, it’s often caused by HPV. Spotting it early can stop it from getting worse.
Bronchial carcinoma in situ is when abnormal cells in the bronchial tubes might turn into lung cancer. It’s linked to smoking and harmful chemicals. Catching it early through screenings can greatly improve treatment chances.
| Type of Cancer in Situ | Location | Associated Risk Factors |
| Melanoma in Situ | Skin (Epidermis) | UV Radiation, Fair Skin |
| Vulvar Intraepithelial Neoplasia (VIN) | Vulva | HPV Infection, Smoking |
| Penile Intraepithelial Neoplasia (PeIN) | Penis | HPV Infection, Poor Hygiene |
| Bronchial Carcinoma in Situ | Bronchial Tubes | Smoking, Carcinogen Exposure |
Studying cancer in situ helps us prevent and manage it better. By knowing who gets it and why, doctors can create better screening plans. This helps catch cancer early.
In the U.S., cancer in situ is a big health issue. About 56,000 people get diagnosed with ductal carcinoma in situ (DCIS) each year. This is a type of breast cancer in situ.
Let’s look at some numbers to understand cancer in situ better:
| Type of Cancer in Situ | Estimated Annual Diagnoses |
| Ductal Carcinoma in Situ (DCIS) | 56,000 |
| Lobular Carcinoma in Situ (LCIS) | Not separately tracked, often found incidentally |
| Cervical Carcinoma in Situ | Varies by age and screening practices |
Age matters a lot when it comes to cancer in situ. DCIS often hits women over 50, while cervical carcinoma in situ affects younger women.
Some groups face higher risks due to genes, environment, or lifestyle. Knowing this helps doctors target their efforts better.
Genes and environment both play a part in cancer in situ risk. Women with a family history of breast cancer, for example, face a higher risk of DCIS. The risk of breast cancer for those with lobular carcinoma in situ is about 25% to 30%.
Exposure to certain chemicals or radiation also raises the risk. Knowing these factors is key to preventing cancer in situ.
To diagnose cancer in situ, doctors use screening, biopsies, and imaging. Finding it early is key to treating it well.
Each type of cancer in situ needs its own screening. For example, ductal carcinoma in situ (DCIS) of the breast is found with mammograms. Cervical carcinoma in situ is spotted with Pap smear tests. Knowing the right screening for each cancer is vital for catching it early.
A medical expert says, “Regular screening is essential for finding cancer in situ. It’s important to stick to the screening guidelines for each cancer type.”
Biopsies are key to confirming cancer in situ. A biopsy takes a small tissue sample for a pathologist to examine. They look for abnormal cells that show CIS.
The biopsy results help doctors understand how much CIS there is and what to do next.
Advanced imaging is also important for diagnosing and treating cancer in situ. Tools like digital mammography, ultrasound, and MRI help see how much CIS there is. This helps doctors plan the best treatment.
“New imaging tech has made it easier to find and treat cancer in situ,” says a top oncologist.
By using screenings, biopsies, and imaging, doctors can find and treat cancer in situ well. This helps patients get better.
Managing cancer in situ well needs a deep understanding of treatment options. The right treatment depends on many things. These include the cancer type, where it is, and how big it is. Also, the patient’s health and what they prefer matters.
Surgery is often the first step for many cancers in situ. For example, surgery is key for melanoma in situ. The aim is to remove the affected area completely to stop it from coming back. The surgery needed can range from simple cuts to more detailed Mohs surgery, based on the tumor’s size and location.
Radiation therapy is sometimes suggested for certain cancers in situ. This is true when surgery can’t get all the cancer or when it’s in a sensitive spot. Modern radiation methods, like IMRT, aim to hit cancer cells hard while keeping healthy tissues safe.
For some cancers in situ, medicines or hormone treatments are used. For instance, in some breast cancers, hormone therapy might be suggested to lower the chance of it coming back. The choice of medicine depends on the cancer’s hormone receptors and other details.
In some cases, watching the cancer closely is a good plan. This means regular check-ups and tests without immediate treatment. Watching closely is often for patients with low-risk cancers or those who can’t handle more aggressive treatments.
Dealing with cancer in situ shows we need a plan that fits each person.
“The key to successful treatment lies in tailoring the approach to the individual patient’s needs and circumstances.”
Healthcare providers can give the best care by looking at each case’s unique details.
Understanding the prognosis for cancer in situ is key for patients and doctors. Early detection helps find cancers like carcinoma in situ (CIS) early. This means better treatment chances and outcomes.
Survival rates for cancer in situ vary by type and location. For example, ductal carcinoma in situ (DCIS) of the breast has a high survival rate with proper treatment. Studies show a nearly 100% 10-year survival rate for DCIS.
Cervical carcinoma in situ also has a good prognosis if caught early. Each cancer type’s survival rate depends on its characteristics and the patient’s health.
Recurrence risks for cancer in situ depend on treatment success and risk factors. Regular monitoring is key to catch any recurrence early. Follow-up care for CIS may include check-ups, imaging, and treatments to prevent recurrence.
For DCIS, annual mammograms are recommended to watch for recurrence or invasive cancer. Patients with cervical carcinoma in situ should also have regular Pap smears as advised by their doctor.
Untreated cancer in situ can progress to invasive cancer. But, with the right treatment, this risk drops. For example, DCIS without treatment may turn into invasive breast cancer over time. Surgery and sometimes radiation can lower this risk.
Not all cancer in situ will turn into invasive cancer, even without treatment. But, it’s hard to predict which ones will. So, treatment and follow-up are very important.
The diagnosis and treatment of cancer in situ affect a patient’s quality of life. This includes physical, psychological, and emotional impacts. Support from healthcare providers, family, and support groups is vital for coping.
Improving the quality of life for patients with cancer in situ is essential. This includes managing side effects, emotional support, and lifestyle changes to enhance well-being.
Getting a cancer in situ diagnosis is just the start of a journey. It’s a time to think carefully and take action. This stage means cancer cells are there but haven’t spread yet. It’s a key moment for treatment.
The news of cancer in situ can be tough on your mind. You might feel scared, worried, or even relieved. Coping strategies are key to get through this. Mindfulness, meditation, and joining support groups can offer a lot of help.
Talking openly with your doctor is also vital. Knowing what’s happening and what to expect can ease your worries. It helps you cope better.
After a cancer in situ diagnosis, regular check-ups are a must. These visits help watch for any signs of cancer growing. How often you need to go depends on your cancer type and health.
For example, people with lobular carcinoma in situ (LCIS) need to get their breasts checked often. Knowing what follow-up care you need helps you stay on top of your health.
Choosing a healthy lifestyle is important when you have cancer in situ. Eating well, staying active, and avoiding harmful substances are good steps. These habits help your health and might lower cancer risk.
Support Resources and Communities
Having support can really help when you’re dealing with cancer in situ. Support groups, online or in-person, let you share and learn from others. It’s a great way to feel less alone.
There are also many organizations that help cancer patients. They offer counseling, educational materials, and help with money issues. Using these resources can make your care journey better and more supportive.
We’ve looked into cancer in situ, where cancer cells are present but haven’t spread. Knowing what cancer in situ means is key for catching it early and treating it well.
Carcinoma in situ, or stage 0 cancer, is a critical point where we can stop cancer from becoming invasive. The meaning of in situ cancer shows how vital early diagnosis and treatment are to stop it from getting worse.
In this article, we’ve talked about the different types of carcinoma in situ, how to diagnose it, and how to treat it. We stress the need for more awareness and research into cancer in situ to help patients more.
By understanding cancer in situ and the importance of catching it early, we can improve how we manage and treat it. Carcinoma in situ needs careful management and follow-up to stop it from turning into invasive cancer.
Cancer in situ, or CIS, is when abnormal cells are present but haven’t spread. It’s the earliest stage of cancer.
Cancer in situ cells stay in one place. Invasive cancer cells spread to other areas of the body.
Common types include ductal carcinoma in situ (DCIS) of the breast and lobular carcinoma in situ (LCIS). There’s also cervical carcinoma in situ and squamous cell carcinoma in situ of the skin and mouth.
Doctors use screening, biopsies, and lab tests to diagnose it. They might also use advanced imaging to help find it.
Treatments vary. They can include surgery, radiation, medicine, hormonal treatments, or watching it closely, depending on the type and where it is.
Yes, it’s stage 0 cancer. This means it’s pre-invasive and hasn’t spread yet.
Risk factors include genetics, environment, age, and demographics. These vary by type of CIS.
Yes, if not treated, CIS can turn into invasive cancer. Early treatment is key to stop this.
Patients with CIS usually have a good prognosis. They have high survival rates and low risk of coming back if treated right.
It can affect mental health. Patients may need ongoing care and lifestyle changes. There are support groups to help.
“In situ” means “in its original place.” In cancer, it means cells are in their place and haven’t spread.
Carcinoma in situ is another name for cancer in situ. It’s when cells grow abnormally but haven’t spread.
Both have abnormal cell growth. But CIS is pre-cancerous. It can turn into invasive cancer if not treated.
National Center for Biotechnology Information. (2025). What Does Cancer in Situ Mean A Complete. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC5161057/)**
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us