At Liv Hospital, we understand the challenges of carcinoma in situ (CIS) of the bladder. It’s a serious form of bladder cancer that can grow quickly. CIS stays in the bladder lining but can turn into invasive cancer if not treated. Carcinoma in situ CIS bladder: A guide to defining this high-grade lesion and the standard treatment, often involving BCG.
Knowing about CIS is key for diagnosis and treatment. It makes up about 10% of non-muscle-invasive bladder cancer cases. This type of cancer is common, making up 75 to 80% of all bladder cancers. Our team uses the latest technology and proven treatments to help patients with CIS.
CIS of the bladder is a tough diagnosis because it’s flat and doesn’t invade. We’ll dive into CIS, its definition, cell details, and how it’s different from other bladder tumors.
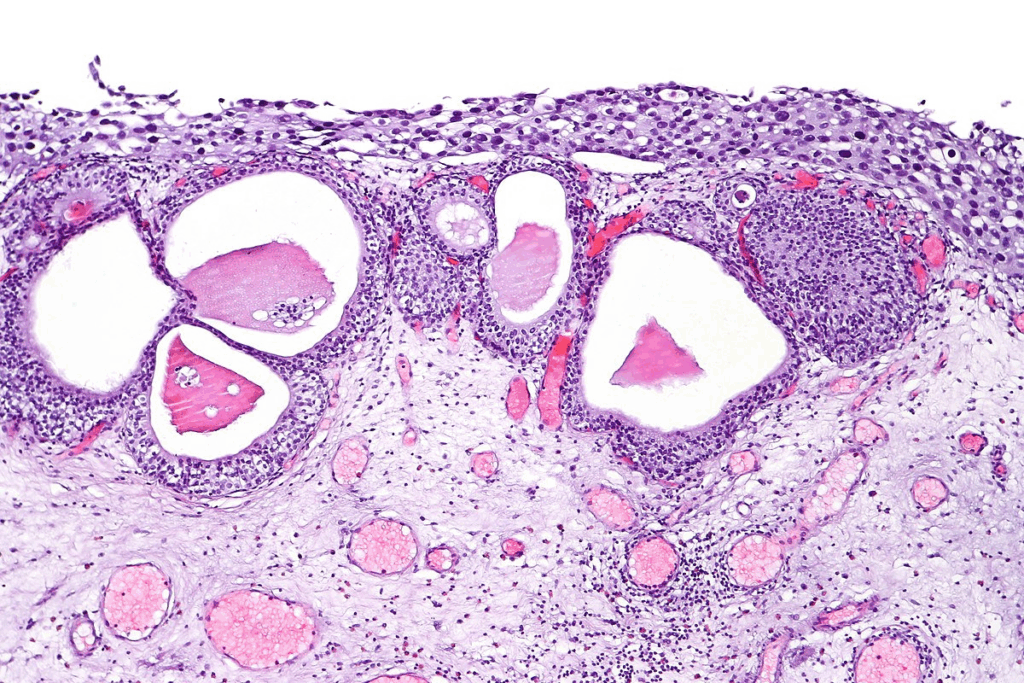
Carcinoma in situ (CIS) of the bladder is a serious, non-invasive urothelial carcinoma. It stays in the top layer of the bladder without breaking through. CIS looks flat, unlike the usual papillary tumors.
Its cells show big changes, like losing shape and having bigger nuclei. These signs mean CIS is a high-grade tumor with big cancer risk. It’s a step before invasive bladder cancer and has a high chance of getting worse.
CIS is flat and hard to see, unlike papillary tumors that stick out. This makes finding CIS tough. Doctors need to be very careful and use special tests to find it.
| Characteristics | CIS | Papillary Bladder Tumors |
| Appearance | Flat | Exophytic |
| Visibility during Cystoscopy | Often not visible | Easily visible |
| Malignant Potentia | High-grade, significant risk | Varies by grade |
Knowing the difference between CIS and papillary tumors is key for right diagnosis and treatment. We’ll keep looking into CIS’s impact and how to manage it in the next parts.

It’s important to know how common CIS bladder cancer is. This helps us find better ways to prevent and treat it. CIS is a serious type of bladder cancer that is hard to diagnose and manage.
Non-muscle-invasive bladder cancer (NMIBC) makes up 75 to 80% of all bladder cancers worldwide. CIS is about 10% of these cases. This shows how important CIS is in NMIBC.
The number of bladder CIS cases varies around the world. This depends on where people live, their age, and what they are exposed to. CIS is more common in Europe and North America than in other places.
There are several things that can increase your risk of getting bladder CIS:
Knowing these risk factors helps us find who is most at risk. We can then take steps to prevent CIS bladder cancer. It’s key to use this knowledge when trying to catch and treat CIS early.
CIS bladder cancer symptoms can be like those of other bladder and urethra issues. This makes it hard to diagnose because the signs are not clear. They don’t always point to cancer right away.
People with CIS might have urinary problems. They often feel the need to pee a lot, have painful urination, and sometimes see blood in their pee. These issues can really affect their life and make them want to see a doctor.
But, these symptoms can also happen with other bladder problems. So, it’s key to get a detailed check-up to figure out what’s going on.
At times, CIS doesn’t show any symptoms. This makes finding out you have it very hard. People might not go to the doctor until it’s too late.
Not having symptoms can cause a delay in finding out you have cancer. It’s why it’s so important for people at risk to get regular check-ups and screenings.
It’s very important to correctly identify CIS of the bladder for the best treatment. To do this, doctors use different methods to find and understand the disease.
Cystoscopy helps doctors see inside the bladder. But CIS lesions are flat and hard to spot with just cystoscopy. Using blue light cystoscopy can make CIS lesions easier to see.
Urine cytology is a key tool for finding CIS. It checks urine for abnormal cells. Even though it’s very specific, it might miss some low-grade tumors. Biomarkers are also used to help diagnose and watch bladder cancer, including CIS.
| Diagnostic Method | Sensitivity | Specificity |
| Urine Cytology | Variable | High |
| Cystoscopy | High | High |
| Biopsy | High | Very High |
A biopsy is the best way to diagnose CIS. It takes a tissue sample from the bladder lining for detailed examination. This can confirm CIS and rule out other issues.
Getting a CIS bladder cancer diagnosis can be tough. But with the right diagnosis and treatment, patients can do well. Our healthcare team is here to give you the best care and support every step of the way.
It’s key for doctors to accurately stage and classify urothelial CIS. This helps them plan the best treatment. Staging shows how far the disease has spread. Classification tells us about the tumor’s features.
The TNM system is a common way to stage bladder cancer, including CIS. It looks at the tumor size (T), nearby lymph nodes (N), and if it has spread (M). CIS is usually Tis in the TNM system, showing it’s a flat, high-grade tumor stuck to the urothelium.
CIS is a high-grade tumor because of its aggressive nature and risk of growing. Histological grading checks the tumor cells’ look and behavior. This helps predict how the tumor might act and how it will react to treatment. Also, studying the tumor’s molecular makeup, like genetic changes and biomarkers, helps us understand CIS better and make treatment choices.
Knowing the stage and grade of CIS is critical for predicting outcomes and treatment plans. We use the TNM system and histological grading to guide our treatment for CIS bladder cancer.
CIS bladder cancer has a high risk of getting worse if not treated right away. It’s a serious type of cancer that can spread if not caught early. This makes it very important to start treatment quickly and effectively.
CIS bladder cancer can turn into a more serious form of cancer if not treated. High-grade tumors, which are linked to CIS, have a high chance of coming back and getting worse. CIS in the bladder is a sign that the cancer might spread.
Many patients with CIS bladder cancer see their cancer come back. This can happen even after treatment. Some cancers come back quickly, while others take longer.
| Recurrence Pattern | Description | Implications |
| Early Recurrence | Recurrence within 12 months of initial treatment | Indicates potentially resistant to initial therapy |
| Late Recurrence | Recurrence after 12 months post-treatment | May need changes in follow-up care |
Knowing how and when cancer might come back helps doctors plan better care. They can adjust treatment plans as needed.
For those with CIS of the bladder, BCG immunotherapy is the first choice. It has changed how we treat bladder cancer, making treatments better.
BCG immunotherapy boosts the body’s immune system to fight bladder cancer cells. It involves putting BCG into the bladder to start an immune reaction. This helps lower the chance of cancer coming back or getting worse.
The immune response from BCG gets immune cells like macrophages and T lymphocytes to kill tumor cells. It uses the body’s own defenses to target cancer, making it a focused treatment for CIS.
BCG treatment follows a set plan. The induction phase includes weekly BCG in the bladder for six weeks. Then, there’s a maintenance phase with more BCG at set times to keep the immune response going and stop cancer from coming back.
| Phase | Description | Duration |
| Induction | Weekly BCG instillations | 6 weeks |
| Maintenance | Periodic BCG instillations | Up to 3 years |
BCG immunotherapy is very effective against CIS of the bladder. Research shows it can greatly lower the risk of cancer coming back or getting worse. Its success comes from its strong immune response against bladder cancer cells.
BCG treatment results can differ, but it’s a key part of CIS treatment. Knowing how BCG works helps doctors give the best care to CIS patients.
Dealing with BCG-refractory disease is tough in treating bladder CIS. About 30 to 40% of patients don’t respond to BCG, so new treatments are needed.
BCG failure means CIS stays or comes back after treatment. We break it down into types like refractory disease, recurrence, and intolerance. Knowing these helps decide what to do next.
For BCG-refractory CIS, we look at other treatments. These include:
These options aim to control the disease and stop it from becoming worse.
Radical cystectomy is a strong treatment for BCG-refractory CIS, mainly for high-risk cases. We consider it when:
Radical cystectomy often leads to better survival rates. But, the choice to have surgery depends on the patient’s wishes and health.
When managing BCG-refractory CIS, weighing the pros and cons of each treatment is key. This ensures patients get the best care for their situation.
Managing carcinoma in situ of the bladder involves close surveillance. After a CIS diagnosis, regular follow-up is key to catch any signs of recurrence or growth early. A structured surveillance plan helps monitor patients effectively.
Regular cystoscopy and urine cytology are essential for CIS bladder cancer surveillance. Cystoscopy lets us see the bladder lining directly, spotting any unusual growths. Urine cytology checks for abnormal cells that could signal a problem.
How often these tests are done matters a lot. We usually do cystoscopy and urine cytology every 3-6 months for the first two years. This depends on the patient’s risk level. If they stay disease-free, we can space out these tests further.
Long-term CIS management goes beyond just watching for signs. It also includes ways to stop the disease from coming back or getting worse. Sticking to the surveillance schedule and reporting any new symptoms quickly is vital.
We also look at several factors that might affect the risk of the disease coming back. These include the type of CIS at first, any previous treatments, and the patient’s overall health.
By taking a proactive and personalized approach to surveillance and follow-up, we can better help patients with CIS bladder cancer.
Getting a CIS diagnosis can be tough. We know patients with CIS need full care and support to handle their condition well.
CIS of the bladder, or cis bladder cancer, is a non-invasive type of bladder cancer. It needs quick treatment and ongoing care. With the right treatment, like BCG immunotherapy, and regular checks, many patients do well.
Dealing with CIS means having a detailed care plan. This includes regular visits, watching for signs of cancer coming back, and help with side effects. We help patients create a care plan that fits their needs and helps them stay healthy.
Understanding CIS bladder cancer helps us give better care and support. This way, we help patients through their diagnosis and treatment.
Carcinoma in situ (CIS) of the bladder is a type of bladder cancer. It stays in the top layer of the bladder lining. This makes it hard to spot during regular checks.
CIS is flat and serious, unlike papillary tumors which stick out. Papillary tumors can be small or big. CIS is harder to find because it’s flat.
Smoking and being around certain chemicals increase your risk. Having had bladder cancer before also raises your risk. Knowing these helps find who’s at risk.
Symptoms include blood in the urine, painful urination, and needing to urinate often. But some people don’t show symptoms, so regular checks are key.
Doctors use cystoscopy, urine tests, and biomarkers to find CIS. A biopsy and looking at the tissue under a microscope confirm it. Accurate diagnosis is key for treatment.
BCG immunotherapy is the main treatment for CIS. It puts BCG in the bladder to fight cancer. It’s effective in managing CIS and stopping it from coming back.
If BCG doesn’t work, other treatments or surgery might be options. The best choice depends on the patient and how far the disease has spread.
CIS is staged using the TNM system. Its seriousness is based on how it looks under a microscope. Knowing this helps plan treatment and predict outcomes.
The outlook for CIS depends on how likely it is to grow and come back. Understanding these risks helps in planning care and talking to patients.
Keeping an eye on CIS is important to catch any signs early. Regular cystoscopy, urine tests, and imaging are part of the follow-up plan.
Carcinoma in situ means cancer cells that haven’t spread. In the bladder, CIS is a non-muscle-invasive cancer type.
Urothelial carcinoma in situ is CIS that starts in the bladder lining. It’s a type of non-muscle-invasive bladder cancer.
Symptoms include blood in the urine, painful urination, and needing to urinate often. Some people might not show symptoms, so regular check-ups are important.
National Center for Biotechnology Information. (2025). What Is Carcinoma In Situ of the Bladder. Retrieved from https://pubmed.ncbi.nlm.nih.gov/19176205/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us