Heart conditions can feel overwhelming. But, thanks to new medical tech, balloon angioplasty offers hope. This method uses a small angioplasty balloon catheter to widen narrowed arteries. It’s often paired with a heart stent to keep the arteries open.
Cardiac balloon surgery is about making more room in an artery blocked by plaque. A tiny balloon pushes plaque against the artery walls. This lets blood flow freely. A stent or tube is then put in to keep the artery open for good.
Key Takeaways
- Balloon angioplasty is a minimally invasive procedure to open narrowed coronary arteries.
- A small angioplasty balloon catheter is used to force plaque against the artery walls.
- A heart stent is often placed to keep the newly opened artery space open.
- The procedure is a significant advancement in treating heart conditions.
- It provides a long-term solution by ensuring blood flows freely through the arteries.
The Fundamentals of Cardiac Balloon Surgery

Understanding cardiac balloon surgery is key to modern heart care. This surgery, known as balloon angioplasty, opens narrowed or blocked coronary arteries. It’s a vital part of heart treatment.
What is Balloon Angioplasty?
Balloon angioplasty, or PCI, is a non-surgical way to clear blocked heart arteries. It lets blood flow freely to the heart. This method is a big step forward in treating heart disease.
The process uses a balloon catheter to reach the blockage. The balloon is then inflated to push the plaque against the artery walls. This improves blood flow.
Historical Development of Coronary Interventions
The first balloon angioplasty was done in the late 1970s by Andreas Gruentzig. His work started the journey of modern coronary interventions. This included the creation of stents to keep arteries open.
Over time, balloon angioplasty has grown a lot. New technology has made it safer and more effective. A leading cardiologist says, “The growth of balloon angioplasty has been amazing. It’s now a safe and effective way to treat heart disease.”
Now, balloon angioplasty is a common treatment for heart disease. It helps patients recover quickly and feel better by opening blocked arteries.
When Is Putting a Balloon in the Heart Necessary?
Cardiologists often recommend balloon angioplasty for patients with symptoms of coronary artery disease. This procedure helps manage heart conditions and prevent further problems.
Common Indications for Balloon Angioplasty
Balloon angioplasty is considered when there’s a big blockage in the coronary arteries. Symptoms include chest pain, shortness of breath, or signs of coronary artery disease. The decision to do the procedure depends on the patient’s condition and health.
The procedure is used to:
- Relieve symptoms of angina
- Improve blood flow to the heart muscle
- Reduce the risk of heart attack
- Enhance the quality of life for patients with coronary artery disease
Heart Attack and Emergency Interventions
In a heart attack, emergency balloon angioplasty is often done to restore blood flow. This quick action can greatly reduce heart damage and improve survival chances.
During a heart attack, the blockage is treated with balloon angioplasty. Often, a stent is placed to keep the artery open. This is critical in minimizing heart muscle damage.
| Scenario | Procedure | Benefits |
| Stable Angina | Balloon Angioplasty | Relieves symptoms, improves quality of life |
| Heart Attack | Emergency Balloon Angioplasty + Stent | Restores blood flow, reduces damage |
| Diagnostic Purposes | Balloon Angioplasty | Assesses coronary artery disease severity |
Diagnostic Uses of Heart Procedure Balloon
Balloon angioplasty is not just for treatment. It also helps diagnose coronary artery disease. Cardiologists can see how severe the disease is and plan the best treatment.
The info from balloon angioplasty helps plan further treatments or manage the condition with medication and lifestyle changes.
Understanding when a balloon angioplasty is needed helps patients and doctors make the best treatment choices for heart conditions.
Comprehensive Patient Assessment Before the Procedure
Before balloon angioplasty, a detailed patient assessment is key. It helps us spot risks and tailor a plan for each patient.
Required Medical Evaluations and Tests
We do many medical tests to understand the patient’s health. These include:
- Electrocardiogram (ECG): Checks the heart’s electrical activity.
- Echocardiogram: Looks at the heart’s structure and function.
- Stress Test: Sees how the heart works under stress.
- Blood Tests: Finds conditions like diabetes or high cholesterol.
- Coronary Angiography: Shows blockages in the coronary arteries.
| Test | Purpose | Significance |
| Electrocardiogram (ECG) | Assess heart’s electrical activity | Detects arrhythmias and ischemia |
| Echocardiogram | Evaluate heart structure and function | Assesses valve function and ventricular performance |
| Stress Test | Measure heart performance under stress | Identifies ischemia and assesses cardiac reserve |
Patient Preparation Instructions
We give patients clear instructions for balloon angioplasty. These include:
- Fasting before the procedure
- Stopping certain medications
- Arranging for a ride home
Medication Management Protocol
We manage medications carefully before, during, and after the procedure. This includes:
- Changing or stopping medications that might cause bleeding
- Using anticoagulants to prevent clots
- Checking medication levels
By doing a thorough patient assessment and giving clear instructions, we can make balloon angioplasty safer and more effective.
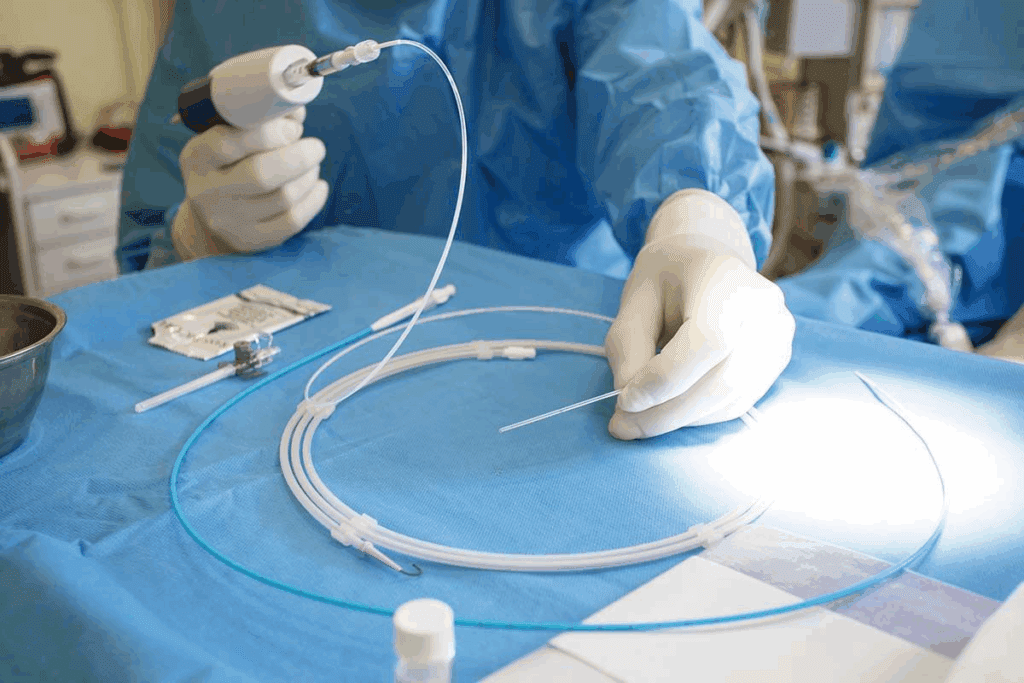
Essential Equipment for Balloon Angioplasty with Stenting
The success of balloon angioplasty with stenting depends on the advanced equipment used. We use top-notch medical devices to ensure the best care and results for our patients.
Types of Angioplasty Balloon Catheters
Angioplasty balloon catheters are key in the procedure. They have a balloon tip that inflates to push plaque against artery walls, improving blood flow. There are different types, including:
- Compliant Balloons: Flexible and can stretch to fit different artery sizes.
- Non-Compliant Balloons: Rigid and keep their size when inflated for precise dilation.
- Drug-Eluting Balloons: Coated with medication that is released during inflation to prevent re-narrowing.
Choosing the right balloon catheter is important. It depends on the patient’s condition, the blockage’s location and severity, and the operator’s preference.
Stent Selection Criteria
Stents are small, mesh-like tubes that keep the artery open after angioplasty. The type of stent chosen depends on several factors, including:
- Bare-Metal Stents: Simple stents that provide structural support.
- Drug-Eluting Stents: Stents coated with medication to prevent re-narrowing.
- Bioresorbable Stents: Stents that dissolve over time, potentially reducing complications.
The selection process involves considering the patient’s needs and the characteristics of the lesion to be treated.
Imaging and Monitoring Equipment
Advanced imaging and monitoring equipment are vital for safe and effective balloon angioplasty with stenting. We use:
- Angiography: To see the coronary arteries and guide the procedure.
- Intravascular Ultrasound (IVUS): To get detailed images of the artery’s interior.
- Fractional Flow Reserve (FFR): To check the severity of coronary stenosis.
These tools help us navigate the arteries precisely, place the stent accurately, and monitor the patient’s response in real-time.
Step 1: Vascular Access Techniques
Vascular access techniques are key to the success of balloon angioplasty. The access site choice depends on the patient’s anatomy, the procedure, and the operator’s preference.
Femoral vs. Radial Approach: Pros and Cons
The femoral artery in the groin and the radial artery in the wrist are the main access sites. Each has its own benefits and drawbacks.
The femoral approach is simpler but carries a higher risk of complications. It also means patients need to rest longer after the procedure.
The radial approach is safer and lets patients move sooner. But, it can be harder for less skilled operators.
| Approach | Advantages | Disadvantages |
| Femoral | Straightforward access, easier to access coronary arteries | Higher risk of vascular complications, longer bed rest required |
| Radial | Lower risk of vascular complications, quicker patient mobilization | Technical challenges, potentially more difficult to access coronary arteries |
Local Anesthesia Administration
Local anesthesia is used at the access site to reduce pain. The type and amount depend on the patient and the procedure’s length.
Effective local anesthesia helps keep patients calm and ensures a smooth procedure. We use lidocaine or similar agents, watching for any bad reactions.
Sheath Insertion and Management
After anesthesia, a small cut is made, and a sheath is inserted into the artery. The sheath lets us use catheters and devices for the angioplasty.
Correct sheath insertion and management are critical to avoid complications. We make sure the sheath is in place and watch the access site closely during the procedure.
Choosing the right access site, using the right local anesthesia, and managing the sheath well improve the safety and success of balloon angioplasty.
Step 2: Navigating to the Coronary Arteries
First, we get vascular access. Then, we use a guide catheter to reach the coronary arteries. This step is key for the balloon angioplasty to work well.
Guide Catheter Selection and Advancement
We pick the right guide catheter based on the patient’s heart anatomy and the procedure needs. We choose one that fits well and aligns with the coronary ostium.
We then push the guide catheter into the coronary ostium under X-ray. This step needs to be done carefully to not harm the artery.
Coronary Angiography for Lesion Identification
With the guide catheter in place, we do coronary angiography. This lets us see the heart’s arteries and find the problem area. We use a contrast agent for this.
The contrast agent shows the heart’s blood vessels. This helps us see where the problem is, how bad it is, and what it looks like.
Assessing Lesion Characteristics
We look closely at the lesion characteristics during angiography. We check its length, width, and if it’s calcified. This info helps us choose the right balloon and stent.
Knowing the details of the lesion helps us customize the treatment. This makes the treatment more likely to succeed for the patient.
Step 3: The Heart Ballooning Procedure in Detail
As we move into the heart ballooning procedure, precision is key. This step is vital in coronary interventions. It needs both technical skill and clinical judgment.
Guidewire Selection and Crossing the Lesion
The first step is picking the right guidewire. We choose it based on the lesion’s details, like its location and complexity. We look at wire stiffness, tip shape, and coating for successful navigation.
Guidewire selection is critical for crossing the lesion safely. A study in the Journal of the American College of Cardiology shows its importance for success.
Balloon Sizing and Selection
After placing the guidewire, we size and select the balloon catheter. We pick it based on the lesion’s diameter and length. Accurate sizing is key for effective dilation without harming the artery.
| Lesion Characteristic | Balloon Size Consideration |
| Lesion Diameter | Balloon diameter should match or slightly exceed the reference vessel diameter |
| Lesion Length | Balloon length should be sufficient to cover the entire lesion |
Inflation Techniques and Pressure Management
Inflation techniques and pressure management are vital. We slowly inflate the balloon to the right pressure, watching for dilation signs. The inflation method depends on the lesion and patient response.
“The art of balloon inflation lies in balancing the need for adequate dilation with the risk of arterial injury.” -Expert Interventional Cardiologist
Monitoring Hemodynamic Response
We watch the patient’s hemodynamic response closely. We track vital signs and look for signs of ischemia or complications.
By managing each step carefully, we can achieve great results and improve patient care.
Step 4: Stent and Balloon Deployment Process
After finding the problem area, we move on to placing the stent and balloon. This step is very important. It makes sure the stent fits right and the artery opens up well.
Stent Selection Based on Lesion Characteristics
Picking the right stent is key. We look at the size, shape, and how complex the problem is. We also think about the patient’s past health and any special needs they might have.
- We measure the size of the problem to pick the right stent size.
- We choose the type of stent based on what’s best for the patient.
Positioning the Stent Delivery System
After picking the stent, we place the delivery system at the right spot. We use X-rays to guide us for accuracy.
- We move the delivery system over a wire to the problem area.
- We check with X-rays to make sure it’s in the right place.
Deployment Techniques and Post-Dilation
To put in the stent, we inflate the balloon slowly. Sometimes, we need to inflate more to make sure the stent fits perfectly.
Important steps during deployment include:
- We inflate the balloon slowly to the right pressure.
- We check if the stent is expanded and fits well against the artery.
- If needed, we use a special balloon to make sure it fits perfectly.
Angiographic Assessment After Deployment
After putting in the stent, we check with X-rays to see how it went. We look for any problems or if the artery is open.
What we aim for in the post-deployment check is to:
- Make sure the stented area is open.
- Find any issues that need quick action.
Balloon Angioplasty vs Stent: Making the Right Clinical Decision
Choosing between balloon angioplasty alone or with stenting depends on many factors. We look at patient characteristics and the specifics of the lesion to pick the best treatment.
Scenarios for Balloon Angioplasty Alone
Balloon angioplasty without stenting is often used for certain patients. This includes those with small vessels or simple lesions. “In selected cases, balloon angioplasty alone can be an effective treatment with fewer complications,” as noted in recent studies.
Here are some scenarios where balloon angioplasty alone might be preferred:
- Lesions in small coronary arteries where stent placement might increase the risk of complications.
- Patients with a high risk of bleeding, as they may require shorter durations of dual antiplatelet therapy.
- Lesions that are not complex and have a low risk of restenosis.
Benefits of Combined Approach
Using both balloon angioplasty and stenting is a common practice. Research shows it reduces the risk of artery re-narrowing. The combined approach offers several benefits, including:
- Improved vessel patency rates.
- Reduced risk of acute vessel closure.
- Enhanced flexibility in treating complex lesions.
Stenting after balloon angioplasty helps keep the artery open. It provides a scaffold that prevents the vessel from collapsing or re-narrowing.
Latest Research on Outcomes and Efficacy
Recent studies have compared balloon angioplasty alone versus a combined approach with stenting. According to a
“study published in a leading cardiology journal, the combined approach resulted in significantly lower rates of target lesion revascularization compared to balloon angioplasty alone.”
We see advancements in both balloon angioplasty and stenting technologies. Ongoing research aims to improve outcomes and reduce complications. The choice between balloon angioplasty and stenting, or using both in combination, will evolve with new evidence and guidelines.
Managing Complications During Heart Balloon Operation
Handling complications well is key to the success of heart balloon procedures. We know that problems can happen even with the best care. Being ready is very important.
Coronary Dissection and Perforation
Coronary dissection and perforation are serious issues that can happen during these operations. Coronary dissection is when the inner lining of the coronary artery tears. This can cause the artery to close suddenly. Perforation is worse, where the artery gets punctured, which can lead to cardiac tamponade.
We handle these problems by stopping the procedure right away and checking how bad the dissection or perforation is. Sometimes, we use a stent to seal the tear or perforation.
Acute Vessel Closure and No-Reflow Phenomenon
Acute vessel closure is when the artery suddenly closes after the procedure. This can cause a heart attack. The no-reflow phenomenon is when the artery opens but blood flow is blocked.
To deal with these issues, we use different methods. We give vasodilators to help blood flow better. In some cases, we use mechanical devices to keep blood flowing.
Stent Thrombosis and Restenosis
Stent thrombosis is when a blood clot forms in the stent, which can cause a heart attack. Restenosis is when the artery narrows again after the procedure.
| Complication | Description | Management Strategy |
| Stent Thrombosis | Blood clot forms within the stent | Emergency thrombectomy, antiplatelet therapy |
| Restenosis | Re-narrowing of the artery | Repeat angioplasty, drug-coated balloon, or stent |
Emergency Protocols and Bailout Strategies
Having emergency plans and backup strategies is vital for heart balloon operations. We make sure our team is ready to act fast and well in emergencies.
Our emergency plans include having the right tools ready, like covered stents for perforations and devices for removing clots.
Post-Procedure Care After Balloon in Heart Procedure
Managing care after a heart balloon procedure is key to avoiding problems and helping you heal. We know the recovery time is as important as the procedure itself. We’re here to help you through this important phase.
Immediate Post-Procedure Monitoring
Right after the procedure, we watch patients closely in a recovery area. We check their heart rate and blood pressure and look for any bleeding or issues at the access site.
Vascular Access Site Management
Taking care of the access site is very important. We give you clear instructions on how to care for it. We also tell you what to look out for, like signs of infection. The site is usually managed with a compression device or manual pressure to stop bleeding.
Dual Antiplatelet Therapy Regimen
To stop clots from forming on the stent, we use a special treatment. This treatment includes aspirin and another medicine, like clopidogrel. It’s very important to take these medicines as directed to avoid problems with the stent.
Activity Restrictions and Recovery Timeline
We tell you what activities to avoid to prevent problems and help you heal. This means no heavy lifting, bending, or hard work for a while. We also give you a timeline for recovery, so you know what to expect and when you can start doing normal things again.
By following these care guidelines, you can help ensure a good outcome and a smooth recovery. Our team is here to support you every step of the way, answering any questions or concerns you may have.
Conclusion: Advancements and Future of Cardiac Balloon Procedures
Cardiac balloon procedures, like balloon angioplasty with stenting, have changed how we treat heart issues. New research keeps making these treatments better. We expect even more progress in technology and methods soon.
The future of these procedures is bright. New stent designs, drug-eluting balloons, and bioabsorbable stents are on the horizon. These innovations will help treat coronary artery disease and other heart problems better.
We’re excited about the future of cardiac balloon surgery. It will likely lead to better results, shorter recovery times, and a better life for those who undergo these treatments. As medical tech advances, we’re dedicated to top-notch healthcare for everyone.
FAQ
What is cardiac balloon surgery, and how does it differ from other heart procedures?
Cardiac balloon surgery, also known as balloon angioplasty, is a minimally invasive procedure. It’s used to widen narrowed or obstructed coronary arteries. Unlike other heart procedures, it uses a balloon catheter to dilate the artery, often with stent placement.
What are the common indications for balloon angioplasty?
It’s often used for patients with coronary artery disease, acute coronary syndrome, or stable angina. It’s also used in emergency heart attack situations.
How is balloon angioplasty performed, and what are the key steps involved?
The procedure starts with vascular access. Then, it involves navigating to the coronary arteries and crossing the lesion with a guidewire. Next, the lesion is ballooned, and a stent might be deployed. The steps can vary based on the patient’s condition and the doctor’s approach.
What is the difference between balloon angioplasty and stenting?
Balloon angioplasty uses a balloon to widen the artery. Stenting involves placing a metal mesh tube (stent) to keep the artery open. Often, both are used together, with the stent deployed during balloon inflation.
What are the possible complications of heart balloon operations, and how are they managed?
Complications include coronary dissection, acute vessel closure, stent thrombosis, and restenosis. Emergency protocols and bailout strategies, like additional stenting or medication, are used to manage these issues.
What is the recovery process like after a balloon in heart procedure?
Post-procedure care includes monitoring, managing the vascular access site, and dual antiplatelet therapy. Activity restrictions are also part of the care. Most patients can return to normal activities within a few days to a week.
How does stent selection impact the outcome of balloon angioplasty?
Stent selection depends on the lesion’s characteristics, like length, diameter, and complexity. Choosing the right stent can improve outcomes and reduce complications.
What is the role of imaging and monitoring equipment during balloon angioplasty?
Imaging and monitoring equipment, like fluoroscopy and hemodynamic monitoring, are key. They guide the procedure, assess the lesion, and monitor the patient’s response.
Can balloon angioplasty be used as a diagnostic tool?
While mainly therapeutic, balloon angioplasty can also provide diagnostic information. It does this through coronary angiography and hemodynamic assessment, helping to identify and characterize coronary lesions.
What advancements are being made in cardiac balloon procedures, and how might they impact treatment?
Advances include better stent technology, improved balloon catheter design, and new imaging modalities. These advancements are expected to make procedures safer, more effective, and better for patients.
References
Valgimigli, M., Bueno, H., Byrne, R. A., Collet, J. P., Costa, F., Jeppsson, A., Jüni, P., Kastrati, A., Kolh, P., Mauri, L., Montalescot, G., Neumann, F. J., Petricevic, M., Roffi, M., Steg, P. G., Windecker, S., Zamorano, J. L., & Levine, G. N. (2018). 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS: The Task Force for dual antiplatelet therapy in coronary artery disease of the European Society of Cardiology (ESC) and of the European Association for Cardio-Thoracic Surgery (EACTS).
Reference
European Heart Journal, 39(3), 213–260. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5837222/







