At Liv Hospital, we know that cardiomyopathy and congestive heart failure are related but different heart issues.
StatPearls says heart failure, or congestive heart failure (CHF), is when the heart can’t pump blood well.
We’ll look at how these conditions differ. This will help patients get the best medical care.
Key Takeaways
- It’s important to know the difference between cardiomyopathy and congestive heart failure for good care.
- Cardiomyopathy is diseases of the heart muscle.
- Congestive heart failure is when the heart can’t pump enough blood.
- Both need detailed treatment and support.
- Liv Hospital has new ways to treat heart problems.
Understanding Heart Disease: The Cardiovascular Burden

Cardiovascular diseases, like cardiomyopathy and congestive heart failure, are big threats to global health. These conditions are very common, affecting many people. They also put a big strain on healthcare systems and economies worldwide.
Heart disease is a major cause of illness and death globally. In the United States, it affects millions. This puts a huge burden on healthcare resources.
The Impact of Heart Conditions in America
The numbers on heart disease are scary. There are about 64.34 million cases of congestive heart failure worldwide. This leads to 9.91 million years lost due to disability. The cost is also huge, with CHF costing $346.17 billion globally.
| Condition | Prevalence | Economic Burden |
| Congestive Heart Failure | 64.34 million cases | $346.17 billion |
| Cardiomyopathy | Varied, depending on type | Significant, though specific global figures are not available |
We really need to understand heart conditions. Knowing about cardiomyopathy and congestive heart failure helps us tackle these challenges.
Why Understanding These Conditions Matters
Learning about heart disease is important for patient care and managing healthcare. A leading cardiology expert said:
“The distinction between cardiomyopathy and congestive heart failure is key for creating effective treatments and improving patient results.”
By knowing the differences, we can improve how we manage heart disease. This leads to better health and more efficient use of healthcare resources.
As we dive deeper into cardiomyopathy and congestive heart failure, it’s clear we need a detailed understanding. This is vital for improving cardiac care.
What is Cardiomyopathy? Definition and Types
Cardiomyopathy refers to various heart muscle disorders with different causes and symptoms. It is a group of diseases that make the heart’s ventricles enlarge and function poorly. We will look into its definition, prevalence, and main types to grasp its impact on heart health.
Definition and Prevalence Statistics
Cardiomyopathy is a disease that affects the heart muscle, making it harder for the heart to pump blood. The American Heart Association says it affects about 1 in 500 adults. The prevalence can change based on the type and the population studied.
A study in the Journal of the American College of Cardiology found a 0.2% prevalence in adults. But, it’s higher in people with a family history of heart disease.
“Cardiomyopathy is a major cause of morbidity and mortality worldwide, and its prevalence is expected to increase due to an aging population and improved survival from other cardiovascular diseases.”
Major Types of Cardiomyopathy
There are several major types of cardiomyopathy, each with unique characteristics:
- Hypertrophic Cardiomyopathy: Thickening of the heart muscle obstructs blood flow.
- Dilated Cardiomyopathy: The heart chambers enlarge, reducing pumping ability.
- Restrictive Cardiomyopathy: The heart muscle stiffens, making it hard for chambers to fill.
- Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC): Fatty tissue replaces muscle in the right ventricle, leading to arrhythmias.
- Left Ventricular Noncompaction Cardiomyopathy: The left ventricle doesn’t develop properly, causing poor function.
| Type | Characteristics | Common Symptoms |
| Hypertrophic | Thickened heart muscle | Chest pain, shortness of breath |
| Dilated | Enlarged heart chambers | Fatigue, swelling in legs |
| Restrictive | Stiffened heart muscle | Shortness of breath, fatigue |
Knowing the different types of cardiomyopathy is key to effective treatment. We will dive deeper into cardiomyopathy and its link to congestive heart failure next.
What is Congestive Heart Failure? Definition and Classification
Congestive heart failure is a long-term condition where the heart can’t pump blood well. This leads to tiredness, swelling in the legs, and shortness of breath. It greatly affects a person’s life quality.
Definition and Prevalence in the US
Congestive heart failure (CHF) is when the heart can’t pump blood fast enough for the body’s needs. In the US, over 6 million adults have heart failure. This number is expected to grow by 46% by 2030, reaching over 8 million adults.
Heart failure gets more common with age. It affects about 1 in 100 people aged 65 to 69. By age 80, it affects about 1 in 10. Knowing about congestive heart failure is key to managing it better.
Classification Systems
Congestive heart failure is sorted into different types based on how well the heart pumps and symptoms. The American College of Cardiology/American Heart Association (ACC/AHA) stages help understand the disease’s progression:
- Stage A: At high risk of heart failure without heart disease or symptoms.
- Stage B: Has heart disease but no symptoms.
- Stage C: Has heart disease and symptoms.
- Stage D: Has severe heart disease and symptoms even at rest.
The New York Heart Association (NYHA) Functional Classification also helps. It rates heart failure based on symptoms and how well a person can function:
- Class I: No limits on activities; no symptoms from everyday activities.
- Class II: Slight limit in activities; feels okay at rest or with light effort.
- Class III: Big limit in activities; feels okay only at rest.
- Class IV: Very limited; feels symptoms even at rest, mostly bedbound.
These systems help doctors diagnose, manage, and treat congestive heart failure better.
Cardiomyopathy and Congestive Heart Failure: The Relationship
To understand heart disease fully, we must see how cardiomyopathy can cause congestive heart failure. Cardiomyopathy weakens the heart muscle, making it hard to pump blood. This weakness can lead to heart failure.
How Cardiomyopathy Can Lead to Heart Failure
Cardiomyopathy can cause heart failure in several ways. First, it can change the heart’s structure, making it less efficient. For example, in dilated cardiomyopathy, the heart gets bigger, making it harder to pump blood. Second, it can cause electrical problems in the heart, leading to arrhythmias that harm the heart’s function.
Key factors in the progression from cardiomyopathy to heart failure include:
- Progressive weakening of the heart muscle
- Increased stiffness of the heart muscle
- Electrical disturbances leading to arrhythmias
- Neurohormonal activation that further stresses the heart
Other Causes of Heart Failure
Cardiomyopathy is a big cause of heart failure, but it’s not the only one. Other causes include coronary artery disease, high blood pressure, heart valve problems, and congenital heart defects. Knowing all these causes helps doctors create better treatment plans.
| Cause of Heart Failure | Description | Impact on Heart Function |
| Coronary Artery Disease | Narrowing or blockage of coronary arteries | Reduces blood flow to the heart muscle, potentially leading to heart failure |
| Hypertension | High blood pressure | Increases workload on the heart, potentially leading to hypertrophy and failure |
| Heart Valve Disorders | Abnormalities in heart valves | Can lead to inefficient blood flow and increased strain on the heart |
In conclusion, the link between cardiomyopathy and congestive heart failure is complex. Knowing how cardiomyopathy can lead to heart failure and other causes is key to helping patients with heart disease.
Difference #1: Pathophysiology – Disease vs. Syndrome
It’s important to know the differences between cardiomyopathy and congestive heart failure. These differences help doctors diagnose and treat patients better. They also show how these conditions progress and how to manage them.
Cardiomyopathy as a Structural Heart Disease
Cardiomyopathy directly affects the heart muscle. It causes structural and functional problems. This disease can lead to hypertrophy, dilation, or restrictive changes in the heart’s ventricles.
The changes in cardiomyopathy can make it hard for the heart to pump blood well. For example, hypertrophic cardiomyopathy can block blood flow. Dilated cardiomyopathy can lower the heart’s pumping ability. These issues can greatly affect a patient’s life and future.
Heart Failure as a Clinical Syndrome
Heart failure is a syndrome, not a disease. It happens when the heart can’t supply enough blood and oxygen. It can be caused by many things, like cardiomyopathy, coronary artery disease, and high blood pressure.
Heart failure can start suddenly or slowly. Symptoms range from mild shortness of breath to severe fluid buildup in the lungs.
The Cause-Effect Relationship
Cardiomyopathy and heart failure are closely linked. Cardiomyopathy can make the heart pump less well, leading to heart failure. As the disease gets worse, the heart’s problems can turn into heart failure symptoms.
Doctors need to understand this link to help patients with cardiomyopathy. This can prevent or delay heart failure. Knowing the causes of heart failure is also key for better treatment and outcomes.
Difference #2: Etiology and Risk Factors
Cardiomyopathy and congestive heart failure have different causes and risk factors. It’s important to understand these differences for effective treatment. Healthcare providers need to know this to create the right treatment plans.
Causes of Different Cardiomyopathies
Cardiomyopathy is a group of heart muscle diseases. The causes can vary, including genetics, infections, and toxic substances.
- Genetic Factors: Many cardiomyopathies are caused by genetic mutations, affecting heart muscle proteins.
- Infections: Viral infections can cause myocarditis, leading to cardiomyopathy.
- Toxic Substances: Exposure to certain chemicals and drugs can also cause cardiomyopathy, showing the impact of lifestyle and environment.
Let’s look at the causes of different cardiomyopathies:
| Type of Cardiomyopathy | Common Causes |
| Hypertrophic Cardiomyopathy | Genetic mutations, often familial |
| Dilated Cardiomyopathy | Genetic factors, myocarditis, toxic exposures |
| Restrictive Cardiomyopathy | Amyloidosis, sarcoidosis, genetic factors |
Risk Factors for Developing Heart Failure
Heart failure has its own set of risk factors. These include high blood pressure, diabetes, and coronary artery disease.
- Hypertension: Chronic high blood pressure puts extra strain on the heart.
- Diabetes Mellitus: Diabetes increases heart failure risk, affecting the heart and blood vessels.
- Coronary Artery Disease: CAD can damage the heart muscle, leading to heart failure.
Knowing these risk factors is key to preventing and treating heart failure early.
| Risk Factor | Description | Impact on Heart Failure Risk |
| Hypertension | Chronic high blood pressure | Increases heart workload, leading to failure |
| Diabetes Mellitus | Chronic metabolic disorder | Associated with cardiovascular complications |
| Coronary Artery Disease | Narrowing or blockage of coronary arteries | Can lead to myocardial infarction and heart failure |
By understanding the causes and risk factors of cardiomyopathy and heart failure, healthcare providers can give better diagnoses and treatments. This helps improve patient outcomes.
Difference #3: Diagnostic Approaches and Criteria
It’s important to know how doctors diagnose cardiomyopathy and congestive heart failure. These two heart conditions are different, even though they both affect the heart. Their tests and criteria are not the same.
Diagnosing Cardiomyopathy
To find out if someone has cardiomyopathy, doctors use imaging and check-ups. Echocardiography is often the first test. It shows how well the heart works and its shape. Magnetic Resonance Imaging (MRI) is also used for its clear pictures of the heart.
Doctors also use electrocardiograms (ECGs) to check the heart’s rhythm. They might look for signs of cardiomyopathy. Genetic tests are used if the condition runs in families.
| Diagnostic Test | Purpose |
| Echocardiography | Assesses heart structure and function |
| MRI | Provides detailed images of the heart |
| ECG | Evaluates heart rhythm |
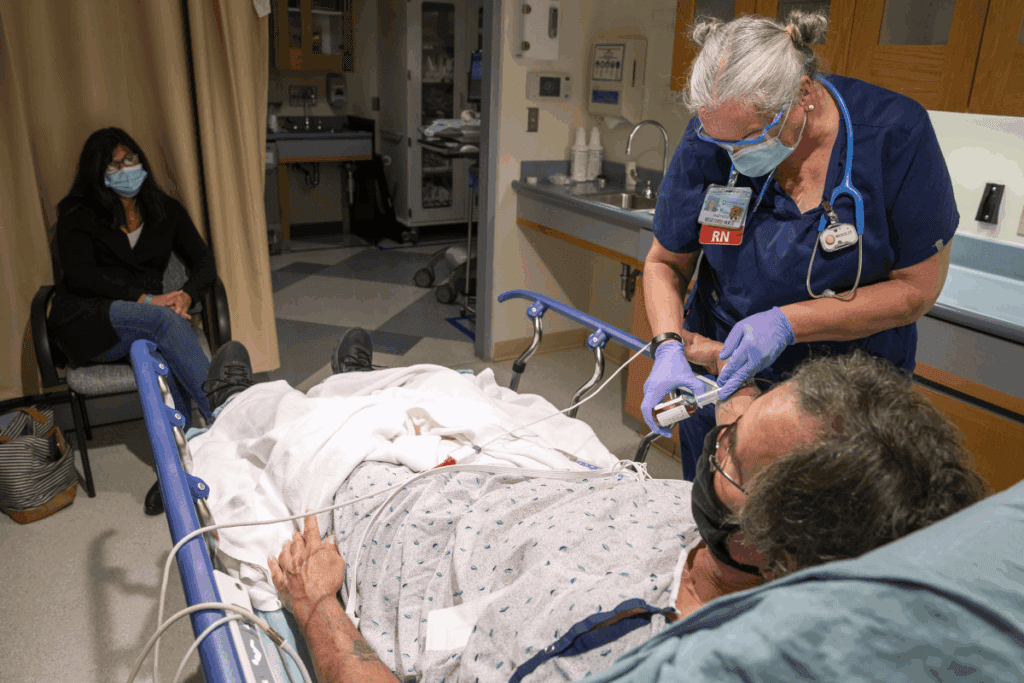
Diagnosing Congestive Heart Failure
Doctors use a few ways to diagnose congestive heart failure. They check biomarkers like B-type natriuretic peptide (BNP) or NT-proBNP. These levels can show if the heart is failing.
Echocardiography is a key tool again. It helps see how well the heart is working. Doctors might also use chest X-rays, ECGs, and stress tests to check the heart’s function under stress.
| Diagnostic Approach | Components |
| Clinical Assessment | Medical history, symptoms, physical examination |
| Biomarkers | BNP or NT-proBNP levels |
| Imaging Studies | Echocardiography, chest X-ray |
In conclusion, diagnosing cardiomyopathy and congestive heart failure has some similarities but also differences. Knowing these differences helps doctors make the right diagnosis and treatment plan.
Difference #4: Clinical Presentation and Symptoms
It’s important to know the symptoms of cardiomyopathy and congestive heart failure to get the right treatment. Both conditions affect the heart but show different signs and symptoms.
Cardiomyopathy Symptoms by Type
Cardiomyopathy symptoms change based on the type. For example, hypertrophic cardiomyopathy causes chest pain and shortness of breath when you’re active. Dilated cardiomyopathy leads to fatigue and swelling in the legs and feet because of fluid buildup.
Hypertrophic cardiomyopathy makes the heart muscle thick, blocking blood flow. Symptoms include syncope or fainting spells. In severe cases, it can cause sudden cardiac death.
Congestive Heart Failure Symptoms
Congestive heart failure (CHF) has its own set of symptoms. The heart can’t pump enough blood, leading to shortness of breath, fatigue, and swelling in the legs, ankles, and feet.
“Heart failure is a complex clinical syndrome characterized by symptoms such as breathlessness, leg or ankle swelling, and fatigue.”
CHF symptoms can get worse over time if not treated. It’s key to catch these symptoms early and start treatment to improve outcomes.
Symptom Progression and Overlap
Symptoms in cardiomyopathy and congestive heart failure can change a lot from person to person. Some may see symptoms get worse slowly, while others stay the same for a long time.
Some symptoms can be the same in both conditions. For instance, shortness of breath is common in both advanced cardiomyopathy and congestive heart failure. Knowing this helps doctors make the right diagnosis.
Difference #5: Treatment Strategies and Management
Treatment for cardiomyopathy and congestive heart failure is different. This is because they affect the heart in unique ways. Each condition needs its own approach based on its specific cause.
Treating Specific Cardiomyopathies
The treatment for cardiomyopathy depends on its type and cause. For example, hypertrophic cardiomyopathy might need medicines for chest pain and shortness of breath. Dilated cardiomyopathy might need treatments to boost heart function and avoid problems.
Medications are key in managing cardiomyopathy. Beta-blockers and anti-arrhythmic drugs help control symptoms and prevent issues. Sometimes, device therapy like ICDs is needed to stop sudden cardiac death.
Managing Congestive Heart Failure
Managing congestive heart failure involves many steps. This includes medicines, lifestyle changes, and device therapy. The main goal is to ease symptoms, slow disease progress, and improve life quality.
- Medications like ACE inhibitors, beta-blockers, and diuretics help manage symptoms and reduce heart workload.
- Lifestyle modifications such as diet changes, regular exercise, and quitting smoking are vital for heart failure management.
- Device therapy, including pacemakers and ICDs, helps by ensuring proper heart rhythm and preventing dangerous arrhythmias.
Understanding the unique treatments for cardiomyopathy and congestive heart failure helps healthcare providers give better care. They can tailor treatment to each patient’s needs.
Difference #6: Prognosis and Disease Progression
Knowing how cardiomyopathy and congestive heart failure progress is key to managing them well. Each condition has its own outcome and rate of getting worse. This affects how we care for patients and what treatments we use.
Cardiomyopathy Outcomes by Type
The outlook for cardiomyopathy changes based on its type. For example, hypertrophic cardiomyopathy usually has a better outlook than dilated cardiomyopathy. This is because dilated cardiomyopathy can lead to severe heart failure. It’s important to know the type of cardiomyopathy to understand the patient’s outcome.
- Hypertrophic Cardiomyopathy: Often has a stable course, but sudden cardiac death can happen.
- Dilated Cardiomyopathy: Can get worse and lead to severe heart failure, needing treatments like heart transplantation.
- Restrictive Cardiomyopathy: Has a poor outlook because of limited treatment options and quick worsening.
Heart Failure Progression and Staging
Heart failure gets worse in stages, as defined by the American College of Cardiology/American Heart Association (ACC/AHA). This staging helps us understand how the disease is getting worse and guides our treatment.
- Stage A: At high risk of heart failure without structural heart disease.
- Stage B: Has structural heart disease but no symptoms.
- Stage C: Has structural heart disease and symptoms.
- Stage D: Has severe heart failure needing advanced treatments.
Factors Affecting Long-term Outlook
Many things can affect how long-term cardiomyopathy and congestive heart failure do. These include other health problems, sticking to treatment, making lifestyle changes, and using advanced treatments.
- Comorbidities: Other health issues like diabetes or high blood pressure can make things worse.
- Treatment Adherence: Following treatment plans can greatly improve outcomes.
- Lifestyle Modifications: Changes like diet, exercise, and quitting smoking can help slow disease progression.
By understanding these factors and the unique traits of each condition, doctors can give more tailored care. This can lead to better results for patients.
Difference #7: Prevention Strategies
Preventing cardiomyopathy and heart failure needs a mix of medical care and lifestyle changes. We’ll look at how a full approach tackles different risks and promotes better living.
Preventing Cardiomyopathy Development
To stop cardiomyopathy, we must handle risks like high blood pressure, diabetes, and stay away from harmful substances. Here’s how to lower your risk:
- Managing hypertension through lifestyle changes and medication
- Controlling diabetes effectively to prevent diabetic cardiomyopathy
- Avoiding excessive alcohol consumption to prevent alcoholic cardiomyopathy
- Maintaining a healthy weight to reduce the risk of cardiomyopathy
Preventing Heart Failure Progression
To stop heart failure from getting worse, we use medicine and lifestyle changes. Important steps include:
- Adhering to prescribed medications such as ACE inhibitors, beta-blockers, and diuretics
- Making lifestyle changes like reducing salt intake, increasing physical activity, and quitting smoking
- Monitoring symptoms closely to catch any signs of worsening heart failure early
These steps can slow down heart failure and make life better for those affected.
Importance of Early Intervention
Early action is key in stopping cardiomyopathy and managing heart failure. It’s vital to:
- Regular check-ups with healthcare providers to monitor cardiovascular health
- Screening for risk factors and underlying conditions that could lead to cardiomyopathy or heart failure
- Prompt treatment of any identified issues to prevent progression
By focusing on prevention and early action, we can lower the number of cases and their effects.
Conclusion: Understanding the Distinction for Better Cardiac Health
It’s key to know the difference between cardiomyopathy and congestive heart failure. This knowledge helps in managing these conditions better. We’ve looked at 7 main differences between them, highlighting their unique traits and how they affect heart health.
Healthcare providers can offer better care by understanding these differences. This knowledge lets them tailor treatments for each patient. It leads to better heart health results for everyone.
As cardiology advances, knowing the fine details between these conditions is vital. This understanding helps us provide better care. It improves the lives of those with these heart issues and boosts overall heart health.
FAQ
Is cardiomyopathy the same as congestive heart failure?
No, they are not the same. Cardiomyopathy is a disease of the heart muscle. Congestive heart failure is when the heart can’t pump enough blood.
What is the difference between cardiomyopathy and heart failure?
Cardiomyopathy is a disease of the heart muscle. Heart failure is when the heart can’t pump enough blood. Cardiomyopathy can cause heart failure, but not all cases do.
Can cardiomyopathy lead to congestive heart failure?
Yes, it can. When the heart muscle is diseased, it can’t pump blood well. This can lead to heart failure.
What are the risk factors for developing heart failure?
High blood pressure, diabetes, and coronary artery disease are risks. So are smoking and obesity.
How is cardiomyopathy diagnosed?
Tests like echocardiography and electrocardiogram (ECG) are used. Cardiac MRI and genetic testing may also be needed.
How is congestive heart failure diagnosed?
Doctors look at symptoms and medical history. They do tests like echocardiography and ECG. Blood tests also help.
What are the treatment strategies for cardiomyopathy?
Treatment varies by type and severity. It may include medicines, lifestyle changes, and devices like pacemakers.
What are the treatment strategies for congestive heart failure?
Treatment includes medicines and lifestyle changes. Devices or surgery may also be needed to improve heart function.
Can cardiomyopathy be prevented?
Some types are genetic and can’t be prevented. But managing risk factors like high blood pressure can help.
Can congestive heart failure be prevented?
Yes, by managing risk factors like high blood pressure and diabetes. A healthy lifestyle is also key.
Is ischemic cardiomyopathy the same as congestive heart failure?
No, they are not the same. Ischemic cardiomyopathy is heart muscle damage from reduced blood flow. It can lead to heart failure, but they are different conditions.
What is the prognosis for cardiomyopathy?
It depends on the type and how well it responds to treatment. Some types can be managed well, while others may worsen.
What is the prognosis for congestive heart failure?
It depends on the cause, treatment, and other health conditions. Treatment has improved, but it’s a serious condition.
References
- Martinez-Lemus, L. A. (2012). The dynamic structure of arterioles. Basic & Clinical Pharmacology & Toxicology, 110(1), 5-11. https://pubmed.ncbi.nlm.nih.gov/21989114/