Coronary artery disease affects millions worldwide. It often needs stenting to improve blood flow. When a stent is placed, it compresses the plaque against the artery walls, helping blood flow to the heart.
We use a catheter to put the stent in the blocked area. This method has changed how we treat coronary artery disease.
It’s important for patients to understand this process and its effects on plaque.
Key Takeaways
- The stent compresses plaque against the artery wall.
- A catheter is used to deliver the stent.
- Stenting improves blood flow to the heart.
- The procedure is minimally invasive.
- Understanding stenting helps patients make informed decisions.
Understanding Arterial Plaque and Coronary Artery Disease

It’s key to know about arterial plaque to handle coronary artery disease. Arterial plaque is a mix of substances that can build up inside arteries. This can make arteries hard and narrow.
What is arterial plaque?
Arterial plaque is made of fat, cholesterol, calcium, and more. It can harden over time, a process called atherosclerosis. This buildup can block blood flow, causing heart problems.
How plaque builds up in arteries
Plaque buildup starts early and is influenced by genetics, lifestyle, and environment. High LDL cholesterol, smoking, high blood pressure, and diabetes help it grow.
As plaque grows, arteries narrow and harden. This reduces blood flow to important areas. Symptoms include chest pain, shortness of breath, and fatigue.
The dangers of plaque buildup
Plaque buildup is dangerous. It can cause heart attacks and strokes if not treated. A ruptured plaque can block an artery, leading to these serious events.
Knowing these risks shows why managing coronary artery disease is so important. Lifestyle changes, medication, and procedures like catheterization can help. By tackling the causes of plaque buildup, we can avoid severe heart problems.
The Role of Stents in Treating Blocked Arteries

Stents have changed how we treat blocked arteries. They are small, mesh-like tubes that keep arteries open. This improves blood flow to important organs.
What is a stent?
A stent is a medical device that keeps arteries open. It’s made of metal or plastic and can be permanent or temporary. The stent is inserted through a catheter and expands at the blocked area.
Types of stents available
There are many types of stents, each with its own benefits. These include:
- Bare-metal stents: Simple metal stents that provide structural support.
- Drug-eluting stents: Stents coated with medication to prevent the artery from narrowing again.
- Bioabsorbable stents: Stents that dissolve over time, reducing long-term complications.
How stents help restore blood flow
Stents keep the artery open after an angioplasty. They ensure blood flows freely. This is key for the heart and other vital organs.
Understanding stents and their types helps patients grasp treatment options for blocked arteries. Stents are a key tool in cardiology. They improve blood flow and lower the risk of heart problems.
When Stent Placement Becomes Necessary
Doctors decide on stent placement when artery blockages cause symptoms. These blockages can lead to heart attacks and strokes. We’ll look at symptoms, how doctors find blockages, and who might need a stent.
Symptoms Indicating Blocked Arteries
Blocked arteries show certain symptoms that need attention. These include:
- Chest pain or angina, which is discomfort or pain in the chest when the heart doesn’t get enough oxygen.
- Shortness of breath, which happens when the heart can’t pump well because of blocked arteries.
- Leg pain or cramping during activity, known as claudication, which is a sign of peripheral artery disease.
Seeing these symptoms early is key for quick medical help. If you notice any, talk to a doctor right away.
Diagnostic Procedures
To find out about blockages, doctors use several tests. These include:
- Angiography: This uses dye and X-rays to see inside the arteries and find blockages.
- Stress Tests: These check how the heart works under stress, usually from exercise or medicine, to spot blockages.
- Ultrasound: A non-invasive test that uses sound waves to make images of the arteries and check blood flow.
These tools help doctors decide if a stent is needed and plan the best treatment.
Determining Candidacy for Stent Placement
Not everyone with blocked arteries needs a stent. The choice to use a stent depends on several things, like:
- The blockage’s severity and where it is.
- The patient’s overall health and medical history.
- The symptoms and how they affect daily life.
We look at these factors carefully to choose the best treatment for each person. Stents are often used when they’re the best option to improve blood flow.
The Catheter: Essential Tool for Stent Delivery
The catheter is key in placing stents in blocked arteries. It helps guide the stent to the right place. This is done by navigating through the body’s complex blood vessels.
Types of Catheters Used
There are many types of catheters for stent placement. Each has its own purpose. Here are a few:
- Guiding catheters: These support and guide the stent.
- Balloon catheters: They work with balloon angioplasty to widen the artery.
- Diagnostic catheters: These help see the blockage and check the artery’s health.
Navigation Through Blood Vessels
Catheters are made to move through blood vessels with great care. They go in through a small cut in the groin or arm. Then, they use imaging to guide them to the blocked artery.
They are made to be flexible and easy to move. This lets them safely reach the blocked area.
To help them move better, catheters have:
- Hydrophilic coatings to cut down on friction and make them easier to track.
- Pre-shaped tips to help them go through tight spots in the blood vessels.
Advancements in Catheter Technology
New tech in catheter design has made stent placement more successful. Some big improvements include:
- Improved materials: New materials make catheters more flexible and last longer.
- Enhanced imaging capabilities: New imaging tools like IVUS and OCT give doctors feedback in real-time.
- Robotic-assisted catheters: Robots are being used to make the procedure more precise and controlled.
Preparing for a Stent Procedure
The days before a stent procedure are key for getting ready. It’s important to prepare your body and mind for this treatment step. Knowing what to do can make the process smoother and more successful.
Medical Evaluations and Tests
Your healthcare team will do many tests before the procedure. These tests help figure out the best treatment for you. They might include blood work, electrocardiograms, and imaging studies like angiograms or ultrasounds. Your doctor will use this info to plan the procedure just for you.
Medication Adjustments
Changing your medications is a big part of getting ready. Your doctor might tell you to stop taking certain medications to lower bleeding risks. It’s very important to follow these instructions and tell your doctor about all your medications and supplements.
- Anticoagulants and antiplatelet drugs may need to be adjusted or temporarily stopped.
- Inform your doctor about any herbal supplements or over-the-counter medications.
- Follow specific instructions regarding the timing of medication adjustments.
Day-of-Procedure Instructions
On the day of the procedure, there are a few things to do. Plan to arrive at the hospital or catheterization lab with plenty of time to spare. You might need to fast before the procedure. Also, make sure someone can drive you home because you might be sleepy from sedatives.
By following these instructions and preparing ahead, you can help make the stent procedure a success. This will also make your recovery smoother.
The Step-by-Step Process of Stent Placement
Learning about the stent placement process can ease worries for those facing it. It’s a key step for treating blocked arteries.
Anesthesia and Initial Preparation
The first step is giving anesthesia to keep the patient comfortable. We use local anesthesia to numb the area where the catheter goes in.
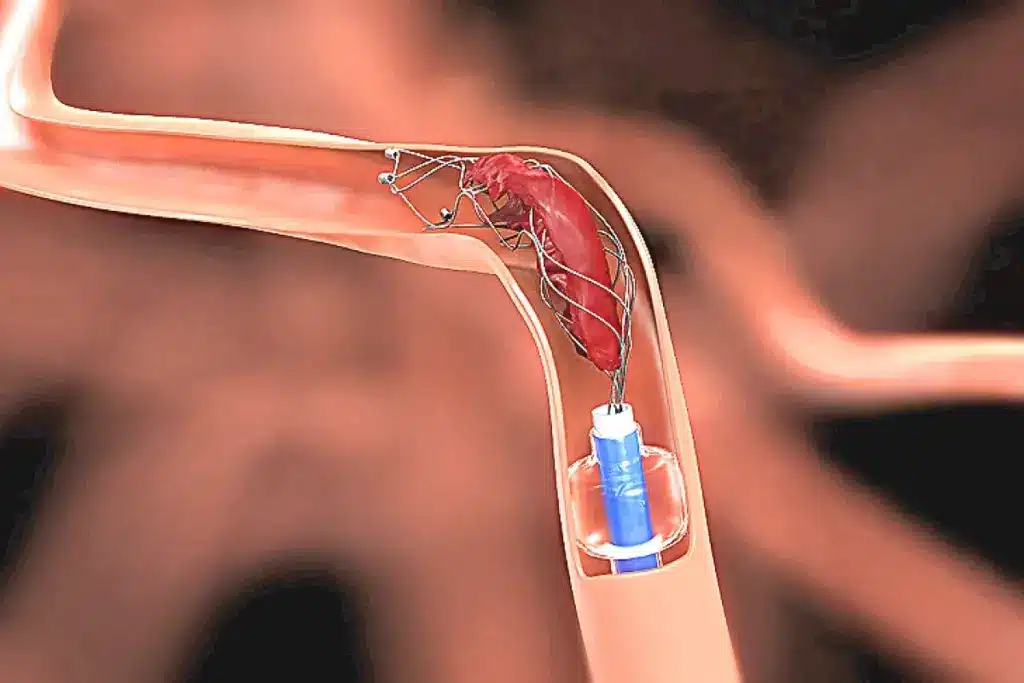
Catheter Insertion and Navigation
Next, we put a catheter into the blocked artery. This catheter is then guided through the blood vessels to the blockage.
Locating the Blockage
With the catheter in place, we use imaging to find the blockage. This is key for placing the stent correctly.
Balloon Angioplasty
Before the stent goes in, we do balloon angioplasty. This step widens the artery by inflating a balloon. It pushes the plaque against the walls, making room for the stent.
|
Step |
Description |
|---|---|
|
Anesthesia and Preparation |
Administering local anesthesia to numb the catheter insertion area. |
|
Catheter Insertion |
Navigating the catheter through blood vessels to the blocked artery. |
|
Locating the Blockage |
Using imaging techniques to identify the exact location of the blockage. |
|
Balloon Angioplasty |
Inflating a balloon to widen the artery and compress plaque. |
What Actually Happens to the Plaque During Stenting
When a stent is put in, it pushes the plaque against the artery walls. This makes blood flow normal again. It changes the plaque and the artery in important ways.
Compression of Plaque Against Arterial Walls
The main way stents work is by pushing the plaque against the artery walls. The stent expands, which moves the plaque outwards. This makes the artery wider.
Key effects of plaque compression include:
- Immediate restoration of blood flow
- Reduction in symptoms related to arterial blockage
- Improved vascular health
Redistribution of Plaque Material
Stenting also moves some plaque material along the artery wall. This can make the plaque spread out more evenly. It might lower the chance of blockages at the same spot later.
Immediate Changes in Blood Flow
Putting in a stent changes blood flow right away. The plaque being pushed against the walls makes the artery wider. This lets blood flow better.
The immediate effects on blood flow include:
- Increased oxygen delivery to the heart muscle
- Reduced symptoms of angina or other ischemia-related conditions
- Enhanced overall cardiac function
Microscopic Changes in Plaque Structure
The stenting process also changes the plaque at a tiny level. The plaque gets compressed and moved around. This can change how the plaque is made and how stable it is.
|
Change |
Description |
Impact |
|---|---|---|
|
Compression |
Plaque is compressed against the arterial wall |
Restores blood flow |
|
Redistribution |
Plaque material is redistributed along the arterial wall |
Potentially reduces future blockage risk |
|
Microscopic Alterations |
Changes in plaque composition and stability |
Influences long-term vascular health |
The stenting process does more than just fix blood flow right away. It also makes long-term changes in the plaque and artery.
Balloon Angioplasty vs. Stent Placement
It’s important to know the difference between balloon angioplasty and stent placement for treating coronary artery disease. Both methods help open blocked arteries. But they work in different ways.
Differences in Approach and Technique
Balloon angioplasty uses a balloon-tipped catheter to push plaque against the artery walls. This widens the artery. Stent placement, on the other hand, uses a mesh-like device (stent) to keep the artery open after the balloon is removed. The stent adds extra support to prevent the artery from narrowing again.
Key differences in technique include:
- The use of a balloon in angioplasty to widen the artery
- The deployment of a stent in stent placement to maintain arterial patency
When Angioplasty Alone is Sufficient
In some cases, just using balloon angioplasty is enough to fix the problem. This is true for patients with less severe blockages. But, the choice depends on the patient’s health and the blockage’s details.
|
Characteristics |
Balloon Angioplasty |
Stent Placement |
|---|---|---|
|
Complexity of Lesion |
Suitable for simpler lesions |
Preferred for complex lesions |
|
Risk of Restenosis |
Higher risk without stent |
Lower risk with stent |
|
Procedure Time |
Generally shorter |
May be longer due to stent deployment |
Benefits of Adding a Stent
Using a stent during angioplasty has many advantages. It lowers the chance of the artery narrowing again and improves long-term results. Stents are very helpful for patients with complex blockages or those at high risk of narrowing.
The benefits of stent placement include:
- Reduced risk of restenosis
- Improved arterial patency
- Better long-term outcomes
Impact on Plaque Management
Both methods affect how plaque is managed. But, stent placement offers more support to the artery walls. This might help prevent plaque from building up again.
Understanding the differences between balloon angioplasty and stent placement helps doctors choose the best treatment. This improves patient outcomes.
Types of Stents and Their Effect on Plaque
There are different stents for treating artery plaque, each with its own benefits. The right stent can greatly affect treatment success and recovery.
Bare-Metal Stents
Bare-metal stents are made of metal mesh. They keep arteries open after angioplasty. They’ve been used for years.
Advantages: Simple design, less expensive than drug-eluting stents.
Disadvantages: Higher risk of in-stent restenosis compared to drug-eluting stents.
Drug-Eluting Stents
Drug-eluting stents have a coating that slowly releases medication. This helps prevent cell growth and reduces restenosis risk.
Advantages: Lower risk of in-stent restenosis, reduced need for repeat procedures.
Disadvantages: Requires longer antiplatelet therapy, higher cost.
Bioabsorbable Stents
Bioabsorbable stents are made from materials that dissolve over time. They might reduce long-term complications of permanent stents.
Advantages: Could reduce long-term complications, restore natural vessel function.
Disadvantages: Limited long-term data, potentially higher risk of certain complications.
Choosing the Right Stent Type
Choosing a stent depends on many factors. These include the patient’s medical history, blockage location and severity, and overall health.
|
Stent Type |
Key Benefits |
Potential Drawbacks |
|---|---|---|
|
Bare-Metal Stents |
Simple, less expensive |
Higher risk of restenosis |
|
Drug-Eluting Stents |
Lower restenosis risk |
Longer antiplatelet therapy, higher cost |
|
Bioabsorbable Stents |
Potential for fewer long-term complications |
Limited long-term data |
We carefully consider these factors to choose the best stent for each patient. This ensures the best possible outcome.
Immediate Post-Procedure Effects
After a stent placement, patients face many immediate effects. These can greatly affect their recovery and health. We’ll help you understand what to expect.
Restored Blood Flow
Stent placement brings back blood flow to the affected area. This can lessen symptoms like chest pain and shortness of breath. Restored blood flow is key for oxygen and nutrients to the heart muscle, boosting heart function.
Recovery in the Hospital
Patients usually stay in the hospital for a while after the procedure. This lets doctors watch for any immediate problems. It’s vital to keep a close eye during this time to fix any issues quickly.
Initial Medication Regimen
Patients are given medications after the stent placement. These help prevent clots and aid in healing. Following this medication is very important to avoid stent thrombosis. We’ll talk about these medications and their role in recovery.
Monitoring for Complications
Watching for complications is a big part of post-procedure care. Doctors look for signs of bleeding, infection, or stent problems. Finding complications early can greatly improve results. It’s important for patients to know the warning signs and tell their doctor right away.
Long-Term Changes to Arterial Plaque After Stenting
Stenting not only opens up blocked arteries but also starts a healing process. This process is key to keeping the artery open long-term. It’s important for doctors to know about these changes to care for patients better.
Healing Process Around the Stent
After a stent is placed, the body starts to heal around it. New tissue grows over the stent, which helps prevent blood clots. This is a critical step in avoiding serious problems.
How fast this healing happens can vary. It depends on the type of stent, the patient’s health, and if they follow their medication plan.
Endothelialization
Another important change is endothelialization. This is when the artery’s inner lining grows over the stent. It’s essential because it lowers the chance of blood clots forming on the stent.
When the endothelium grows well over the stent, it means the stent is working right. This is good news for avoiding future problems.
Potential for Restenosis
Even with stenting, there’s a chance for restenosis, or the artery to narrow again. This can happen when new tissue grows inside the stent.
|
Factors Influencing Restenosis |
Description |
Impact on Restenosis Risk |
|---|---|---|
|
Stent Type |
Drug-eluting stents release medication to prevent cell proliferation. |
Reduced risk |
|
Patient Health |
Diabetes and other conditions can affect healing and tissue growth. |
Increased risk |
|
Medication Adherence |
Adhering to antiplatelet therapy reduces clot formation risk. |
Reduced risk |
Long-term Arterial Remodeling
After stenting, the artery goes through changes. This includes adapting to the stent and adjusting blood flow. These changes are complex and depend on many factors.
Understanding these changes helps doctors take better care of patients after stenting. It can lead to better health outcomes.
By knowing about these long-term changes, doctors can improve patient care. This leads to better health outcomes after stenting.
Potential Complications and Risks
Stent placement is a common medical procedure. But, like any invasive treatment, it comes with risks. It’s important for patients to know these risks to make smart choices about their health.
In-Stent Restenosis
In-stent restenosis happens when the artery narrows again after a stent is placed. This can cause symptoms to come back or even lead to a heart attack. Drug-eluting stents help by releasing medicine that stops cells from growing too much.
Stent Thrombosis
Stent thrombosis is a serious issue where a blood clot forms inside the stent. It’s a life-threatening problem that needs quick medical help. Dual antiplatelet therapy is used to prevent this by stopping platelets from sticking together.
Arterial Injury
There’s a chance of damaging the artery wall during stent placement. This can cause bleeding, hematoma, or even a tear in the artery. Thanks to better technology and skills, these risks are getting lower.
Allergic Reactions
Some people might have an allergic reaction to the stent materials or the drugs used during the procedure. Pre-procedure assessment helps find these allergies. This way, doctors can take the right steps to avoid problems.
Knowing about these risks helps doctors take better care of patients. It also lets patients play a big part in their recovery and health in the long run.
Life After Stent Placement: Managing Plaque Buildup
The journey doesn’t end with stent placement. It’s key to manage plaque buildup proactively. After a stent procedure, patients must keep their heart health up. This involves sticking to medication, making lifestyle changes, and regular check-ups.
Medication Adherence
Following your medication plan is vital after a stent. Antiplatelet therapy helps prevent clots around the stent. Taking these meds as directed by your doctor keeps the stent open and working right.
It’s important to know the side effects of these meds. If you have concerns, talk to your doctor. Consistency is key in keeping your arteries healthy.
Lifestyle Modifications
Big lifestyle changes can help manage plaque buildup. Dietary adjustments to a heart-healthy diet are key. Eating more fruits, veggies, and whole grains is important. Regular physical activity also helps keep your heart healthy.
Also, quitting smoking is a must for smokers. Smoking speeds up plaque buildup. We’re here to help you make these changes.
Follow-up Care and Monitoring
Regular visits to your healthcare provider are essential. These visits help monitor your arteries and stent. They catch any problems early, like in-stent restenosis.
Also, don’t forget about cardiac check-ups and tests as your doctor suggests. These check-ups help keep an eye on your heart’s health and spot any issues that need attention.
Preventing New Plaque Formation
Stopping new plaque from forming is an ongoing effort. It involves sticking to your lifestyle changes and medication. Managing risk factors like high blood pressure, diabetes, and high cholesterol is also key.
By working with your healthcare team and sticking to your treatment plan, you can lower the risk of new plaque. This helps keep your stent healthy.
Conclusion
It’s key to know what happens to plaque when a stent is used. Stents help manage coronary artery disease well. They improve blood flow and lower the risk of problems from plaque buildup.
Stent placement, made possible by catheterization, is a mainstay in treating blocked arteries. Stents push plaque against the artery walls, helping blood flow normally. But, knowing the risks like in-stent restenosis and stent thrombosis is important.
After a stent is placed, proper care is critical for long-term success. This means following medication, making lifestyle changes, and going to follow-up visits. Stent placement is very effective, but we must also think about overall heart health. This includes understanding the benefits and drawbacks of treatments like pacemakers.
Using stents with other plaque management strategies can help patients with coronary artery disease. As medical technology and treatments get better, our aim is to give the best care to those with this condition.
FAQ
What is a stent and how does it work?
A stent is a small, mesh-like device. It’s put into a blocked or narrowed artery to restore blood flow. It expands to keep the artery open, allowing blood to flow freely.
What happens to the plaque when a stent is put in?
When a stent is placed, the plaque is compressed against the arterial walls. The stent helps to keep the artery open, improving blood flow.
What are the different types of stents available?
There are several types of stents, including bare-metal stents, drug-eluting stents, and bioabsorbable stents. Each type has its own benefits and is chosen based on individual patient needs.
How is a stent placed in the body?
Stent placement involves using a catheter to deliver the stent to the blocked artery. The stent is then expanded using balloon angioplasty to keep the artery open.
What is the role of catheters in stent delivery?
Catheters are used to navigate through blood vessels to deliver the stent to the blocked artery. They play a critical role in the stent placement procedure.
What are the risks associated with stent placement?
Potential risks include in-stent restenosis, stent thrombosis, arterial injury, and allergic reactions. But these risks are relatively low, and the procedure is generally safe.
How can plaque buildup be managed after stent placement?
Managing plaque buildup after stent placement involves medication adherence, lifestyle modifications, follow-up care, and strategies to prevent new plaque formation.
What is the difference between balloon angioplasty and stent placement?
Balloon angioplasty involves using a balloon to expand the artery. Stent placement involves placing a stent to keep the artery open. Stent placement is often used in conjunction with balloon angioplasty.
How long does it take to recover from a stent procedure?
Recovery time varies, but most patients can return to normal activities within a few days to a week after the procedure.
Can a pacemaker be used in conjunction with a stent?
Yes, a pacemaker can be used in conjunction with a stent. But the presence of a pacemaker may require special consideration during the stent placement procedure.
Are there any restrictions on activities after stent placement?
Patients may be advised to avoid heavy lifting, bending, or strenuous activities for a period after the procedure. But most normal activities can be resumed shortly after.
How often should I follow up with my doctor after stent placement?
Follow-up care is key after stent placement. Patients should follow their doctor’s instructions for follow-up appointments and monitoring.
Can a urinary catheter be used in patients with certain medical conditions?
Urinary catheters, such as Foley catheters, are used to manage urinary retention or incontinence. Their use depends on individual patient needs and medical conditions.
What are the possible complications of using a catheter?
Possible complications of catheter use include infection, injury to the urinary tract, and blockage of the catheter. Proper care and maintenance can minimize these risks.
How is a catheter inserted and removed?
Catheter insertion and removal should be performed by a healthcare professional. Proper technique is essential to minimize discomfort and prevent complications.
Reference
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK507788/








