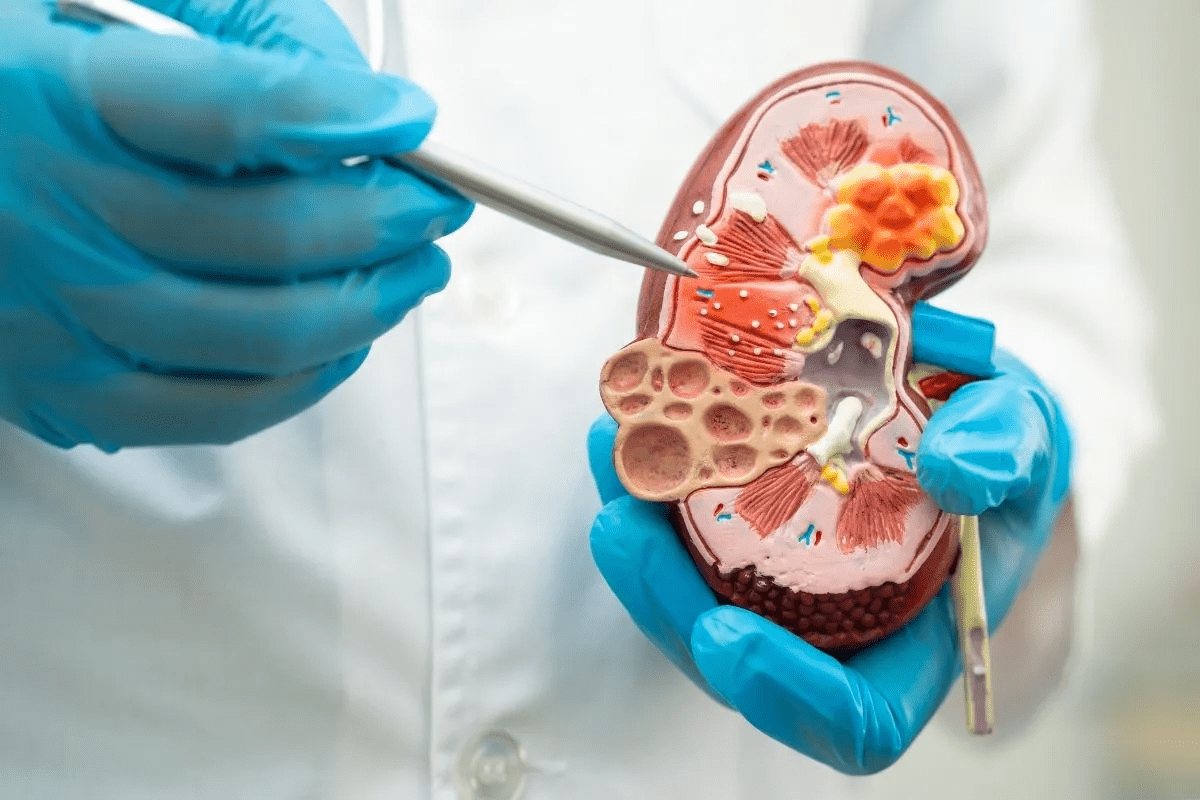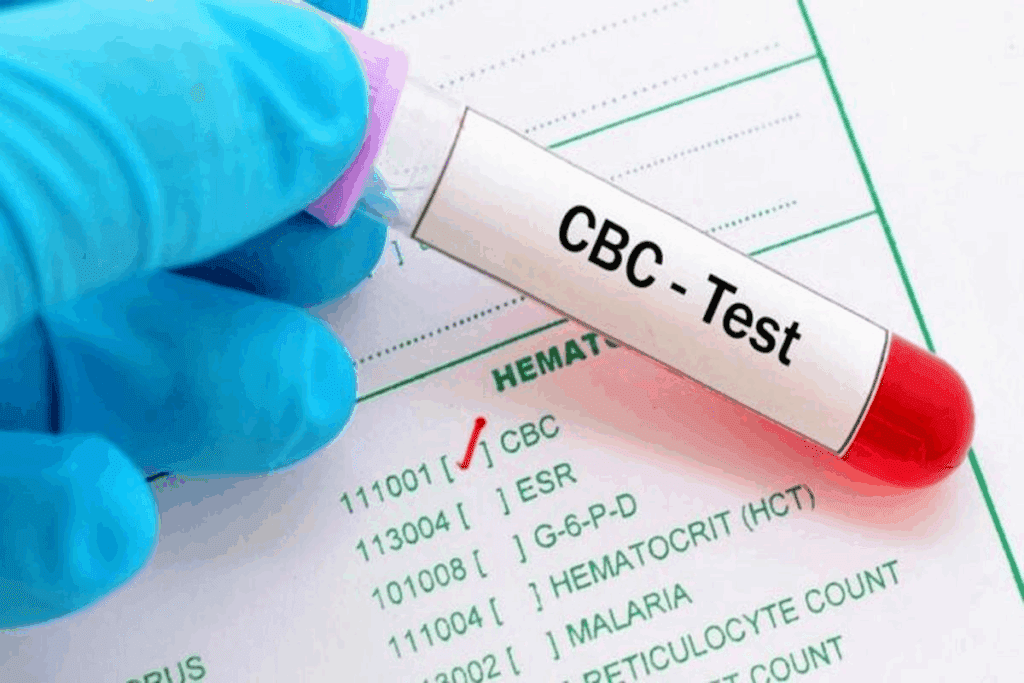
A Complete Blood Count (CBC) is a key tool in healthcare. It helps doctors find many health issues, including infections. In fact, CBC infection detection plays an important role in identifying early signs of illness. Did you know that over 100 million CBC tests are done every year in the United States?
This blood test looks at different parts of the blood. It checks white blood cells, red blood cells, and platelets — all vital for CBC infection detection and overall health evaluation. This gives doctors important clues about how the body fights infections.
By looking at these parts, doctors can spot and keep track of many conditions with greater accuracy.
Key Takeaways
- A CBC test is used to diagnose various health conditions, including infections.
- The test measures different blood components, such as white and red blood cells.
- Understanding CBC results is key for both healthcare professionals and patients.
- CBC helps in monitoring the body’s response to infections.
- It is one of the most commonly performed blood tests in the United States.
Understanding the Complete Blood Count (CBC) Test
The CBC test is a detailed blood analysis that checks your overall health. It looks at white blood cells, red blood cells, and platelets. This helps doctors see how your body fights off infections.
Components of a Standard CBC Test
A standard CBC test checks several important things:
- White Blood Cell (WBC) Count: This counts the white blood cells, which fight infections.
- Red Blood Cell (RBC) Count: It looks at the red blood cells, which carry oxygen.
- Platelet Count: This checks the platelets, which help blood clot.
- Hemoglobin (Hb) and Hematocrit (Hct): They measure hemoglobin and the red blood cell ratio in the blood.
Together, these parts give a full picture of your health.
The Role of CBC in Diagnosing Infections
The CBC test is key in finding infections. For example, a high white blood cell count means you might have an infection. It can also tell if it’s a bacterial or viral infection by looking at the white blood cells.
Doctors use CBC test results to understand what’s wrong and how to treat it.
How White Blood Cell Count Indicates Infection
Knowing about white blood cell count is key to diagnosing and treating infections. White blood cells, or WBCs, are vital for our immune system. They help fight off infections. The number of these cells in our blood tells us a lot about infections.
Normal White Blood Cell Ranges
A normal white blood cell count is between 4,500 and 11,000 cells per microliter of blood. This number can change based on the lab, age, sex, and other factors. It’s important to know these ranges to understand test results.
Leukocytosis: Elevated White Blood Cell Count
Leukocytosis means having more than 11,000 white blood cells per microliter. It often shows an infection, inflammation, or immune response. Many things can cause it, like bacterial infections, stress, and some medicines.
The table below shows common reasons for leukocytosis:
| Cause | Description |
| Bacterial Infections | Infections caused by bacteria, such as pneumonia or urinary tract infections. |
| Viral Infections | Some viral infections can cause an increase in white blood cell count. |
| Inflammatory Conditions | Conditions like rheumatoid arthritis can lead to leukocytosis. |
Leukopenia: Decreased White Blood Cell Count
Leukopenia means having fewer than 4,500 white blood cells per microliter. It makes us more likely to get infections because our bodies can’t fight off germs well. It can be caused by viral infections, bone marrow problems, and some medicines.
It’s important to know about leukocytosis and leukopenia to diagnose and treat infections correctly.
The Significance of CBC Differential in Infection Detection

The CBC differential test is key in finding infections by looking at blood cells. It helps understand how the body fights infections and what kind it is.
This test counts different white blood cells: neutrophils, lymphocytes, monocytes, eosinophils, and basophils. Changes in these counts show different infections.
Neutrophil Elevation and Bacterial Infections
Neutrophils fight bacterial infections. When their count goes up, it means a bacterial infection is likely.
Lymphocyte Count Changes in Viral Infections
Lymphocytes are important for fighting viruses. Changes in their count help diagnose viral infections.
Monocyte Levels in Chronic Infections
Monocytes turn into macrophages, key in chronic infections. High monocyte levels suggest a chronic infection.
Eosinophil and Basophil Counts in Parasitic and Allergic Reactions
Eosinophils and basophils deal with parasites and allergies. Changes in their counts help diagnose these issues.
Healthcare providers use the CBC differential to understand infections and how the body reacts. This helps them make the right treatment choices.
Bacterial Infections Detected Through CBC
A CBC test is key in finding bacterial infections. It shows how severe an infection is. It looks at blood’s parts, like red and white blood cells, and platelets.
Healthcare providers use this info to spot signs of bacterial infections.
Common Bacterial Infection Patterns in CBC Results
Bacterial infections make white blood cells go up, called leukocytosis. The CBC differential count shows which white blood cells are higher. For example, more neutrophils mean a bacterial infection.
Case Examples: Pneumonia, UTIs, and Sepsis
Pneumonia, UTIs, and sepsis show unique signs in CBC results. Pneumonia raises white blood cells, mostly neutrophils. UTIs also increase white blood cells, with signs of immature cells.
Sepsis, a serious infection, changes CBC results a lot. It can make white blood cells go up or down.
Doctors use CBC results with symptoms and other tests to diagnose and treat infections. Knowing these patterns helps doctors care for patients better.
Viral Infections and Their CBC Signatures
It’s key to know how viral infections affect CBC results for correct diagnosis and treatment. Viral infections can change CBC parameters in specific ways. These changes help doctors tell them apart from bacterial infections.
Characteristic CBC Changes in Viral Infections
Viral infections often show certain changes in CBC results. A big change is lymphocytosis, or an increase in lymphocytes. This is common in infections like infectious mononucleosis from the Epstein-Barr virus (EBV).
Another key change is leukopenia, or a drop in white blood cells. This can happen in many viral infections, like the flu and HIV. The CBC differential count also shows changes in other white blood cells, like neutropenia. This is often seen in viral infections.
Distinguishing Viral from Bacterial Infections
Differentiating between viral from bacterial infections is very important for the right treatment. CBC results can give important clues. For example, bacterial infections usually cause neutrophilia, or more neutrophils. But viral infections often lead to lymphocytosis or leukopenia.
The CBC differential count helps figure out the infection type. A high lymphocyte count might mean a viral infection. But an elevated neutrophil count could point to a bacterial infection. Knowing these patterns helps doctors make better decisions about testing and treatment.
Parasitic Infections Revealed by CBC Parameters
Diagnosing parasitic infections often uses CBC parameters. These tests show how the body reacts to infections. They check the blood’s white, red cells, and platelets.
Some CBC parameters are key to finding parasitic infections. Eosinophilia, for example, is important. It’s when eosinophils, a type of white blood cell, are too high.
Eosinophilia in Parasitic Infections
Eosinophilia is linked to parasitic infections, like those from worms. Seeing high eosinophils means there might be an infection. This calls for more tests.
Eosinophils fight parasites by releasing special granules. A high eosinophil count can hint at an infection. But, it’s not the only sign.
Blood Smear Analysis for Parasitic Detection
Blood smear analysis is also vital for finding parasites. It looks at a blood sample under a microscope. This way, doctors can see parasites directly.
This method is great for spotting Plasmodium (malaria) and Trypanosoma (African trypanosomiasis or sleeping sickness). Seeing the parasites lets doctors confirm the diagnosis.
Using CBC parameters and blood smear analysis together helps diagnose parasitic infections better. It gives a clearer picture of how the infection affects the body.
Fungal Infections and CBC Abnormalities
Fungal infections can change CBC parameters in specific ways. These changes help doctors understand the infection’s severity and type. Knowing these changes is key to diagnosing and treating fungal infections.
Common CBC Patterns in Fungal Infections
In fungal infections, CBC results often show certain patterns. For example, an elevated white blood cell count is common. It shows the body’s fight against the infection. The differential count might show neutrophilia, which is important in fighting off fungal pathogens.
Eosinophilia is another pattern seen in some fungal infections. This includes infections from Aspergillus or Coccidioides. Eosinophilia can hint at a parasitic or allergic reaction, but in fungal infections, it points to a specific disease.
Limitations of CBC in Fungal Infection Diagnosis
Even though CBC gives insights into the body’s response to fungal infections, it has limitations in diagnosing them. It can’t pinpoint the specific fungal pathogen or tell different fungal infections apart. For a clear diagnosis, tests like fungal cultures, serological tests, or molecular diagnostics are needed.
Also, CBC findings can be similar in bacterial or viral infections. So, it’s important to look at CBC results along with other diagnostic findings. This helps in making an accurate diagnosis and treatment plan.
CBC Infection Detection: Capabilities and Limitations
It’s important to know what a CBC can and can’t do in detecting infections. The CBC test is a key tool in healthcare. It helps doctors understand if you have an infection and what kind it might be.
What a CBC Can Reliably Indicate About Infections
A CBC can show if you have an infection by looking at your white blood cells and other blood markers. For example, a high white blood cell count usually means you have a bacterial infection. The pattern of your white blood cells can also hint at viral or parasitic infections.
Key indicators of infection in CBC results include:
- Leukocytosis (elevated WBC count)
- Neutrophilia (increased neutrophils) for bacterial infections
- Lymphocytosis (increased lymphocytes) for viral infections
- Eosinophilia (increased eosinophils) for parasitic infections
When Additional Diagnostic Tests Are Necessary
Even though a CBC is very helpful, it’s not always enough to know for sure what’s going on. Sometimes, you need more tests to figure out the exact infection.
Examples of additional diagnostic tests that may be required include:
- Blood cultures to identify specific bacterial pathogens
- Serological tests to detect antibodies against specific viruses or parasites
- Molecular diagnostic tests, such as PCR, are used to detect microbial DNA
In summary, while a CBC is a great tool for finding infections, knowing its limits is key. By using CBC results along with more tests and the doctor’s judgment, doctors can give better diagnoses and treatments.
The Role of Red Blood Cell Parameters in Infection Assessment
Red blood cell parameters play a key role in assessing infections. They include indicators like hemoglobin and hematocrit levels. These can give insights into how severe and long-lasting an infection is.
Hemoglobin and Hematocrit Changes During Infections
Infections can cause changes in hemoglobin and hematocrit levels. This happens due to inflammation and poor nutrition. Hemoglobin levels might drop in chronic infections because of the body’s fight against the infection. Hematocrit, which shows the red blood cell count, can also change based on the infection’s severity and length.
Some important changes include:
- Lower hemoglobin levels due to anemia of chronic disease
- Changes in hematocrit levels show red blood cell mass changes
- More erythropoietin production in response to inflammation
Anemia of Chronic Disease and Infection
Anemia of chronic disease often happens in patients with long-term infections. It’s caused by the body’s ongoing fight against the infection, leading to less red blood cell production. This condition can make managing the infection harder, affecting patient recovery and hospital stays.
Key points about anemia of chronic disease are:
- Less erythropoietin production or effectiveness
- Higher hepcidin levels cause iron to be locked away
- Long-term inflammation makes it hard for iron to be used for red blood cells
It’s important to understand these changes to better manage patients with chronic infections. Treating anemia can help improve their overall health.
Platelet Count Abnormalities in Various Infections
Platelet count changes are common in infections. They offer important clues for diagnosis. A CBC test can show these changes in platelet count.
The CBC test checks platelet count, among other things. Changes in this count can signal an infection. Knowing these changes helps doctors diagnose and treat.
Thrombocytopenia in Severe Infections
Thrombocytopenia, or low platelet count, is seen in severe infections. It can happen due to bone marrow issues, increased platelet destruction, or the spleen holding onto platelets.
Severe infections like sepsis can cause thrombocytopenia. This is because of the body’s inflammatory response and possible DIC.
Reactive Thrombocytosis Following Infection
Some infections lead to reactive thrombocytosis, or a high platelet count. This happens as the body fights off the infection. It’s seen during the recovery phase.
The body’s fight against infection boosts thrombopoiesis. This leads to more platelets being made. While usually harmless, reactive thrombocytosis can sometimes cause problems.
Acute-Phase Reactants and Their Relationship to CBC
Diagnosing infections often involves clinical checks and lab tests like CBC and acute-phase reactants. These proteins change in the blood when inflammation happens. They help see how the body reacts to infection.
Using CBC and acute-phase reactants together gives more info. This is helpful when a CBC alone isn’t enough. It helps in understanding the infection’s severity and the body’s response.
C-Reactive Protein and Erythrocyte Sedimentation Rate
CRP and ESR are key acute-phase reactants. CRP is made by the liver when there’s inflammation. ESR shows how fast red blood cells settle, hinting at inflammation.
CRP and ESR show inflammation, but not just from infections. They help doctors understand the infection’s severity when used with CBC results.
Combining CBC with Acute-Phase Reactants for Better Diagnosis
Using CBC with CRP and ESR improves diagnosis. For example, a patient with a bacterial infection might have high white blood cells and CRP. This shows a big inflammatory response.
This method helps doctors see if treatment is working. If CRP goes down and CBC improves, treatment is likely effective. But if CRP stays high, treatment might need changing.
In summary, using CBC and acute-phase reactants together is a strong way to diagnose. It gives doctors a clearer view of a patient’s health. This helps manage infections better.
Special CBC Findings in Specific Infections
Understanding special CBC findings is key to diagnosing infections. Certain infections cause unique changes in CBC results. These changes are vital for accurate diagnosis and effective treatment.
Malaria and Other Blood Parasites
Malaria, caused by Plasmodium parasites, can be detected through CBC findings. Anemia, thrombocytopenia, and sometimes leukopenia are hallmark signs. The CBC may also show an elevated monocyte count and a normal or low white blood cell count.
A notable feature of malaria is the presence of parasites within red blood cells. This can be identified on a blood smear examination. It’s a critical diagnostic tool, essential in regions where malaria is common.
| CBC Parameter | Typical Findings in Malaria |
| Hemoglobin | Decreased |
| Platelet Count | Thrombocytopenia |
| White Blood Cell Count | Normal or Low |
Infectious Mononucleosis and Atypical Lymphocytes
Infectious mononucleosis, caused by the Epstein-Barr virus (EBV), is marked by atypical lymphocytes in the CBC. These cells are larger than normal lymphocytes and have distinctive features.
The CBC typically shows lymphocytosis, with a significant proportion of atypical lymphocytes. This finding is a key diagnostic criterion for infectious mononucleosis.
“The presence of atypical lymphocytes is a hallmark of infectious mononucleosis, aiding in its diagnosis.”
Source: Clinical Hematology
Sepsis and Left Shift in Neutrophils
Sepsis, a life-threatening condition caused by an overwhelming immune response to infection, can be indicated by specific CBC findings. One of the critical signs is the presence of a left shift in neutrophils, also known as bandemia.
A left shift refers to an increase in immature neutrophils (bands) in the blood, indicating a severe bacterial infection. The CBC may also show leukocytosis, with an elevated total white blood cell count.
The presence of a left shift in neutrophils is a critical indicator of sepsis. It guides prompt and appropriate treatment.
Interpreting CBC Results in Immunocompromised Patients
Understanding CBC results for immunocompromised patients is complex. These patients, like those on chemotherapy, have immune systems that don’t work as well. This makes it hard to tell if they have an infection just by looking at their CBC results.
How Immunosuppression Affects CBC Infection Markers
Immunosuppression changes how infections show up on CBC tests. For example, someone on chemotherapy might not get the usual increase in white blood cells when they have a bacterial infection. It’s important to know this to make the right diagnosis.
Key changes in CBC results for immunocompromised patients include:
- Lower white blood cell counts (leukopenia) make it hard to spot infections.
- Changes in the types of white blood cells, like fewer neutrophils, affect fighting infections.
- Atypical lymphocyte counts might mean a viral infection or other immune system issues.
Special Considerations for Cancer Patients Receiving Chemotherapy
Cancer patients on chemotherapy face special challenges. Their treatments can suppress the bone marrow, hiding signs of infection in their CBC results.
“The challenge in diagnosing infections in immunocompromised patients lies in the subtlety of their CBC results, requiring a high index of suspicion and often additional diagnostic testing.” – A Hematologist
It’s vital to closely examine each part of the CBC. This includes:
| CBC Parameter | Typical Change in Infection | Change in Immunocompromised |
| White Blood Cell Count | Increased (leukocytosis) | Decreased (leukopenia) or blunted response |
| Neutrophil Count | Increased | Decreased (neutropenia) |
| Lymphocyte Count | Variable | Altered, potentially decreased |
By carefully looking at CBC results and knowing the patient’s immune status, doctors can better understand infections. This helps them choose the right treatment.
When to Order a CBC for Suspected Infections
Healthcare providers need to know when to order a CBC for suspected infections. This ensures they act quickly. A CBC test gives important information about a patient’s health. It helps find out if there’s an infection and what kind it is.
Clinical Scenarios Warranting CBC Testing
There are several times when a CBC test is needed for suspected infections. These include:
- Patients with a fever that doesn’t have a clear cause
- People showing signs of sepsis, like a fast heart rate, fast breathing, and confusion
- Patients who often get infections or have weakened immune systems
- Those with infections in one area that might spread, like pneumonia or UTIs
In these cases, a CBC can spot changes in blood cell counts. This might mean there’s an infection. For example, too many white blood cells could mean a bacterial infection. Too few might point to a viral infection or problems with the bone marrow.
Frequency of CBC Monitoring During Infection Treatment
How often to check a CBC during treatment depends on the infection’s severity and the patient’s response. It also depends on any extra health issues. Usually, CBCs are checked more often in very sick patients or those with serious infections.
For example, in sepsis, CBCs might be checked daily or more often. This helps see how well the patient is doing with antibiotics and catches any new problems early. For simpler infections, CBCs might be checked every few days or weekly.
Effective use of CBC testing in managing infections depends on understanding the situation and the patient’s needs. Knowing when to order a CBC and how to read the results helps doctors make better choices for their patients.
Conclusion: The Value of CBC in Infection Management
A Complete Blood Count (CBC) is key in fighting infections. It tells us a lot about the infection’s presence, how bad it is, and what type it is.
When we check for infections, we look at different parts of the blood. This includes white blood cells, how they’re different, and red blood cells.
Doctors use this info to find infections, see how they’re growing, and check if treatments are working.
Using CBC helps doctors tell infections apart. They can spot bacterial, viral, and parasitic infections. It also helps them find any serious problems.
In short, CBC is a main tool in diagnosing and managing infections. It gives doctors important clues to help patients get better.
FAQ
What is a Complete Blood Count (CBC) test, and how is it used in diagnosing infections?
A CBC test checks different parts of your blood. It looks at white blood cells, red blood cells, and platelets. It helps find health problems, like infections, by spotting odd changes in these parts.
How does white blood cell count indicate infection?
White blood cells fight off infections. If there are too many or too few, it might mean you have an infection. Knowing what’s normal and what’s not helps doctors diagnose better.
What is the significance of CBC differential in infection detection?
A CBC differential test looks at different types of white blood cells. It shows if you have a bacterial, viral, or parasitic infection. This helps doctors figure out what’s causing your illness.
Can CBC detect bacterial infections, and if so, how?
Yes, CBC can spot bacterial infections. It looks at white blood cell counts and types. For example, it can find pneumonia, UTIs, and sepsis.
How do viral infections affect CBC results?
Viral infections change CBC results in specific ways. This helps doctors tell them apart from bacterial infections. Knowing these changes is key to correct diagnosis and treatment.
What CBC parameters can indicate parasitic infections?
Elevated eosinophil counts can point to parasitic infections. Blood smears also help find parasites. CBC gives important clues about parasitic infections.
Can CBC diagnose fungal infections, and what are its limitations?
Fungal infections can change CBC results, but CBC isn’t perfect for diagnosing them. Knowing its limits helps doctors make accurate diagnoses and treatments.
What are the capabilities and limitations of CBC in infection detection?
CBC is useful for infection detection, but has its limits. Sometimes, more tests are needed. Knowing when to use CBC and when to add more tests is important for accurate diagnosis.
How do red blood cell parameters relate to infection assessment?
Changes in hemoglobin and hematocrit levels can indicate infections. Anemia of chronic disease is common in long-term infections. These changes offer insights into infection severity and duration.
What is the significance of platelet count abnormalities in various infections?
Thrombocytopenia (low platelet count) can happen in severe infections. Reactive thrombocytosis (high platelet count) can follow infections. These changes help understand infection severity and progression.
How do acute-phase reactants relate to CBC, and what is their significance in infection diagnosis?
C-reactive protein and erythrocyte sedimentation rate are markers of infection. Used with CBC, they improve diagnosis accuracy. Combining these tests is beneficial.
How should CBC results be interpreted in immunocompromised patients?
Immunocompromised patients, like those on chemotherapy, have unique CBC results. Understanding how these changes relate to infections is critical for accurate diagnosis.
When should a CBC be ordered for suspected infections?
CBC testing is needed in many situations. The frequency of testing depends on the infection and treatment. Knowing when to use CBC helps improve diagnosis and care.
References
- Seo, I. H., & Lee, Y. J. (2022). Usefulness of Complete Blood Count (CBC) to assess cardiovascular and metabolic diseases in clinical settings: A comprehensive literature review. International Journal of Molecular Sciences, 23(23), 14827. https://pmc.ncbi.nlm.nih.gov/articles/PMC9687310/