Sudden vision loss is alarming. Central Retinal Vein Occlusion (CRVO) is a serious condition that needs immediate care. It happens when a blood clot or less blood flow blocks the central retinal vein. This mostly affects adults over 50.
CRVO is the second most common retinal vascular disorder after diabetic retinopathy. Knowing the signs, causes, and treatments is key for early action and saving vision. We will look at the main signs of CRVO and what causes it. This helps patients and doctors spot this serious vision problem early.
Key Takeaways
- CRVO is a serious retinal vascular disorder that can cause sudden vision loss.
- It mainly affects adults aged 50 and older.
- Understanding CRVO signs and causes is vital for timely medical help.
- CRVO treatment options are available to save vision.
- Quick medical care is needed to avoid permanent vision loss.
Understanding Central Retinal Vein Occlusion
CRVO is a serious eye condition where the central retinal vein gets blocked. This blockage causes changes in the retina that can hurt your vision. To fully understand CRVO, we need to look at its definition, how common it is, the anatomy of retinal veins, and how it affects vision.
Definition and Epidemiology
Central Retinal Vein Occlusion happens when the central retinal vein gets blocked. This vein is key for draining blood from the retina. It’s more common in older adults and those with hypertension and diabetes.
Studies show CRVO is a big cause of vision loss worldwide. The rate of CRVO varies among different groups.
CRVO is linked to other health issues like heart disease and diabetes. Knowing this helps in preventing and treating CRVO.
Anatomy of Retinal Venous Drainage
The retina’s veins drain through the central retinal vein, which goes out through the optic nerve. The anatomy of these veins is complex. The central retinal vein can be compressed at the lamina cribrosa.
The retinal venous drainage system is key to the retina’s health. Any blockage can cause serious problems like hemorrhages and edema.
Impact on Visual Function
CRVO can severely affect your vision. Symptoms include blurred vision, floaters, and sudden vision loss. How much your vision is affected depends on the blockage’s severity and any other health issues.
CRVO’s effects aren’t just short-term. It can also cause long-term vision problems like macular edema and new blood vessel growth. Knowing these possible effects helps in managing patient hopes and making treatment plans.
Types of CRVO: Clinical Significance and Prognosis
Knowing the types of CRVO is key to understanding the disease’s impact and future outlook. CRVO can be divided into three main types: non-ischemic, ischemic, and impending. Each type shows different symptoms and outcomes.
Non-Ischemic CRVO (70% of Cases)
Non-ischemic CRVO makes up about 70% of cases and often has a better outlook for vision. People with this type usually have dilated and tortuous retinal veins and retinal hemorrhages mainly in the back of the eye. Their vision can vary, but many start with relatively good sight.
A leading ophthalmologist notes, “Non-ischemic CRVO has a better chance of recovery, but it’s important to keep an eye on it for signs of change.” Early detection and management are vital to avoid serious issues.
Ischemic CRVO (30% of Cases)
Ischemic CRVO, making up about 30% of cases, has a much worse outlook for vision. The retina shows widespread hemorrhages, cotton-wool spots, and areas where blood flow is blocked. This type is more severe and carries a higher risk of serious complications.
A clinical study found, “Ischemic CRVO is at high risk for neovascular glaucoma, leading to severe vision loss if not treated quickly.” Managing ischemic CRVO requires close monitoring and timely action to avoid serious problems.
Impending CRVO: The Early Warning Stage
Impending CRVO is an early stage where symptoms like transient visual obscurations or retinal venous dilation may appear. Spotting impending CRVO early is critical for early intervention to possibly prevent full CRVO.
A medical expert says, “Identifying those at risk of CRVO and managing their conditions can prevent CRVO.” Risk factor modification and regular eye exams are essential for managing risk.
In summary, knowing the different types of CRVO is vital for understanding its impact and future. Non-ischemic CRVO has a better outlook, while ischemic CRVO is riskier. Impending CRVO is an early sign where quick action can change the disease’s course.
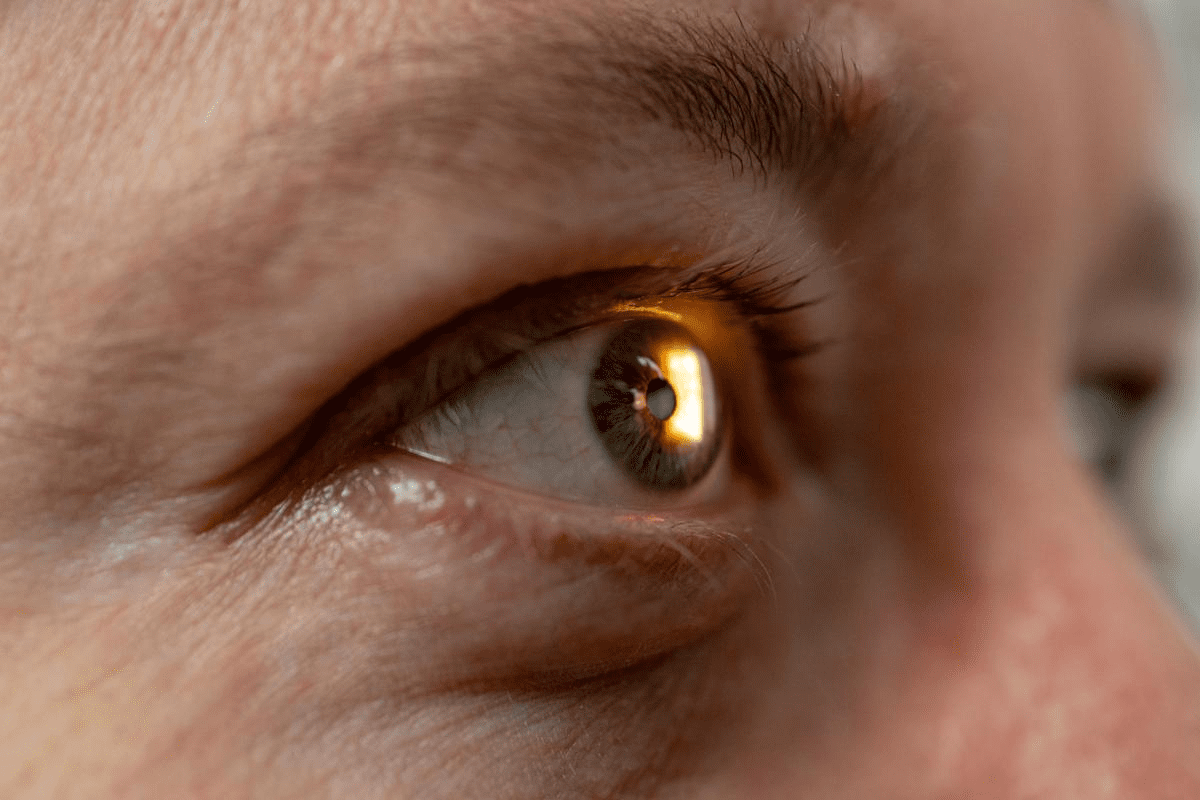
5 Key Signs of Central Retinal Vein Occlusion Fundoscopy
Fundoscopy is key in spotting Central Retinal Vein Occlusion (CRVO). It lets doctors see the retina and find signs of CRVO.
Dilated and Tortuous Retinal Veins
During fundoscopy, doctors see veins that are big and twisted. These veins are full and bent, showing they can’t drain well. This is a big sign of CRVO.
The “Blood and Thunder” Retinal Hemorrhages
CRVO also shows up with big retinal hemorrhages. They look like “blood and thunder.” These happen when veins and capillaries burst, spilling blood into the retina.
Cotton-Wool Spots: Indicators of Retinal Ischemia
Cotton-wool spots are another sign of CRVO. They show where the retina isn’t getting enough blood. Seeing these spots means the retina is badly damaged.
Retinal Edema and Macular Involvement
CRVO can also cause the retina to swell, affecting the macula. This can hurt vision a lot. Fundoscopy helps see how bad the swelling is and how it affects the macula.
These five signs together show how CRVO affects the retina. Spotting them in fundoscopy helps doctors diagnose CRVO and choose the right treatment.
Pathophysiology: How CRVO Develops
To understand CRVO, we must look at vascular compression at the lamina cribrosa. The lamina cribrosa is key because the central retinal vein goes through it. This makes it prone to compression.
Vascular Compression at the Lamina Cribrosa
The central retinal vein gets compressed at the lamina cribrosa. This happens due to intrinsic factors like the vein’s narrow shape. It also happens because of extrinsic factors like high eye pressure or artery changes.
This compression causes blood flow problems, damage to the inner lining of the vein, and clot formation.
Thrombus Formation Mechanisms
Thrombus formation in CRVO comes from several factors. These include slow blood flow, a tendency to clot easily, and damage to the vein’s lining. The process starts with the activation of clotting factors and platelets.
This leads to a clot that blocks the vein. Understanding these mechanisms is key to finding effective treatments.
Cascade of Retinal Damage
When the vein is blocked, the retina starts to suffer. The blockage raises pressure, causes bleeding, and swelling. The retina then doesn’t get enough blood, leading to ischemia.
This triggers the release of VEGF, which makes swelling worse and encourages new blood vessel growth. This chain of events can severely harm vision if not treated.
We know CRVO’s pathophysiology is complex and involves many factors. By grasping these mechanisms, we can improve how we manage the condition and help patients better.
Common Causes and Risk Factors
CRVO is caused by many factors, including vascular, systemic, and eye-related risks. Knowing these risks helps us spot who’s at high risk and how to prevent it.
Age-Related Vascular Changes
Getting older increases the risk of CRVO due to changes in blood vessels. Vascular stiffness and atherosclerosis grow with age. This makes retinal veins more likely to get blocked.
Systemic Conditions: Hypertension, Diabetes, and Hyperlipidemia
Conditions like hypertension, diabetes mellitus, and hyperlipidemia are key in CRVO development. They damage blood vessels and raise the chance of blood clots. It’s important to manage these conditions to lower CRVO risk.
Hypertension can cause vascular endothelial dysfunction, making blood clots more likely. Diabetes can lead to retinal microvascular changes, raising CRVO risk even more.
Ocular Risk Factors
Ocular factors, like glaucoma and ocular hypertension, also play a part in CRVO. High eye pressure can squeeze retinal veins, raising the risk of blockage.
Hematologic Disorders and Hypercoagulable States
Hematologic disorders that cause hypercoagulable states, such as factor V Leiden mutation and antiphospholipid syndrome, increase CRVO risk. These conditions make blood clotting more likely, which can block retinal veins.
It’s vital to understand these risk factors for early CRVO detection and management. By tackling these conditions, we can lower CRVO risk and its complications.
Comprehensive Diagnostic Approach
Diagnosing CRVO requires a mix of clinical checks, advanced imaging, and lab tests. We use these tools to spot CRVO and gauge its severity.
Clinical Examination Techniques
Starting with a detailed medical history is key in diagnosing CRVO. We look for risk factors like high blood pressure, diabetes, and heart disease. Checking your vision is also important.
Fundoscopy lets us see signs of CRVO, like swollen veins and bleeding in the retina. These signs help us understand how severe the CRVO is.
Advanced Imaging: Fluorescein Angiography and OCT
Advanced imaging is vital for CRVO diagnosis. Fluorescein angiography shows how blood flows in the retina. It helps us see if there’s blockage or leakage.
Optical Coherence Tomography (OCT) gives us detailed images of the retina. It helps us measure thickness and spot swelling. OCT is key for tracking the disease and treatment success.
Laboratory Investigations
We run lab tests to find out if other health issues are causing CRVO. These include tests for diabetes, high blood pressure, and high cholesterol. Sometimes, we check for blood clotting disorders, too.
Laboratory Test | Purpose |
Fasting glucose | To diagnose diabetes |
Lipid profile | To assess for hyperlipidemia |
Blood pressure monitoring | To diagnose hypertension |
Thrombophilia screen | To identify thrombophilic disorders |
Differential Diagnosis Considerations
When we diagnose CRVO, we also think about other conditions that might look similar. These include diabetic retinopathy and other eye problems. A thorough check helps us make the right diagnosis and treatment plan.
Evidence-Based Treatment Options
Central Retinal Vein Occlusion (CRVO) treatment is complex. It uses many proven methods. Knowing the condition well is key to choosing the right treatment.
Medical Management of Underlying Conditions
It’s important to manage health issues like high blood pressure, diabetes, and high cholesterol. These can cause CRVO. Fixing these problems can help avoid more serious issues and improve vision.
A study in the Journal of Ophthalmology showed managing these conditions is vital. Patients with controlled blood pressure and diabetes saw better vision than those who didn’t.
Anti-VEGF Intravitreal Injections
Anti-Vascular Endothelial Growth Factor (anti-VEGF) injections are a big help in treating CRVO. They cut down swelling in the macula and help eyes see better by stopping new blood vessels from growing.
Benefits of anti-VEGF injections include:
- Reduced macular edema
- Improved visual acuity
- Inhibition of neovascularization
Doctors often use drugs like ranibizumab and aflibercept. How often you get these shots depends on how well you respond to treatment.
Corticosteroid Therapy
Corticosteroids are another option for CRVO, mainly for those who don’t get better with anti-VEGF shots. They help reduce swelling and inflammation, which can improve vision.
These drugs can be given as shots or implants. But, they can also cause side effects like cataracts and high eye pressure. These need to be watched closely.
Laser Photocoagulation Techniques
Laser treatment is used for CRVO, mostly for those with ischemic CRVO or at risk of new blood vessel growth. It helps by reducing ischemia and stopping new blood vessels from forming.
Treatment Modality | Indications | Benefits |
Anti-VEGF Injections | Macular edema, neovascularization | Improved visual acuity, reduced macular edema |
Corticosteroid Therapy | Inflammation, macular edema | Reduced inflammation, improved visual outcomes |
Laser Photocoagulation | Ischemic CRVO, neovascular complications | Reduced retinal ischemia, prevention of neovascularization |
In summary, treating CRVO requires a variety of proven methods. This includes managing health issues and using advanced treatments like anti-VEGF shots, corticosteroids, and laser therapy. Knowing the benefits and when to use each can help doctors give better care and improve patient results.
Complications and Long-Term Management
Managing CRVO well means knowing its possible problems. We must watch out for risks and deal with them to help our patients the most.
Neovascular Glaucoma: A Sight-Threatening Complication
Neovascular glaucoma is a big problem from CRVO. It happens when new, weak blood vessels grow in the iris and angle. This can cause high eye pressure and serious vision loss if not treated fast.
We need to keep an eye on patients for signs of new blood vessels. This includes iris neovascularization and angle neovascularization. Finding it early is key to managing it well.
Persistent Macular Edema
Persistent macular edema is another big issue from CRVO. It can cause long-term vision problems. We use optical coherence tomography (OCT) to check the macula’s thickness and edema.
Condition | Characteristics | Management |
Neovascular Glaucoma | New blood vessel formation in iris and angle, increased IOP | Anti-VEGF injections, pan-retinal photocoagulation |
Persistent Macular Edema | Chronic fluid accumulation in the macula | Anti-VEGF injections, corticosteroids, macular grid laser |
Monitoring Protocols and Follow-up Care
Regular check-ups are key for managing CRVO problems. We suggest a follow-up plan that includes:
- Monthly visits for the first 3-6 months
- OCT imaging at each visit
- Fluorescein angiography as needed
Visual Rehabilitation Strategies
Helping patients use what vision they have is important. We help them through:
- Low vision aids
- Vision therapy
- Counseling on adaptive techniques
By knowing about CRVO’s problems and using good long-term care, we can make patients’ lives better.
Prevention Strategies and Risk Reduction
To prevent Central Retinal Vein Occlusion (CRVO), we need to manage risk factors and make lifestyle changes. Early detection is also key. By tackling these areas, we can lower the risk of CRVO or lessen its effects if it happens.
Managing Systemic Conditions
It’s important to control risk factors like high blood pressure, diabetes, and high cholesterol to prevent CRVO. Working with your doctor to manage these conditions is essential.
Key strategies include:
- Managing blood pressure through medication, diet, and exercise
- Maintaining good glycemic control for diabetic patients
- Lowering cholesterol levels through diet, exercise, and medication if necessary
Lifestyle Adjustments
Changing your lifestyle can help prevent CRVO. A healthy lifestyle can manage risk factors and improve eye health.
Recommended lifestyle changes include:
- Quitting smoking to reduce vascular risk
- Engaging in regular physical activity to improve circulation and overall health
- Maintaining a balanced diet rich in fruits, vegetables, and omega-3 fatty acids
Early Detection of Impending CRVO
Spotting CRVO early is critical to avoid vision loss. Regular eye exams can catch risk factors and early signs of CRVO.
Key components of early detection include:
- Regular eye exams, more so for those with risk factors
- Watching for sudden vision loss or distortion
- Knowing your family history and genetic risk
Management of Fellow Eye Risk
If you’ve had CRVO in one eye, you’re at higher risk in the other. Close monitoring and preventive steps are needed.
Strategies for managing fellow eye risk include:
- Regular follow-up appointments with an eye care specialist
- Continued management of systemic risk factors
- Prompt reporting of any new symptoms or vision changes
By using these prevention strategies and risk reduction methods, we can greatly reduce CRVO’s impact. This helps preserve vision and improves patient outcomes.
Conclusion
Central Retinal Vein Occlusion (CRVO) is a serious cause of vision loss. It’s important to know its signs, causes, and treatments. We’ve talked about the main signs and how to diagnose and treat it.
Managing CRVO well means a team effort. This includes treating underlying conditions and using special eye injections. We also use laser treatments to help. Knowing how to treat CRVO helps us give patients the best care.
CRVO needs a detailed plan for diagnosis and treatment. It’s key to manage risk factors and make lifestyle changes early. Our goal is to offer top-notch healthcare to international patients. We’re dedicated to helping those with CRVO see their best.
FAQ
What is Central Retinal Vein Occlusion (CRVO)?
CRVO is when the main vein draining blood from the retina gets blocked. This leads to vision problems and can cause severe vision loss.
What are the symptoms of CRVO?
Symptoms include sudden vision loss, blurred vision, and vision that looks distorted. You might also see retinal hemorrhages and edema.
What are the different types of CRVO?
There are two main types: non-ischemic CRVO and ischemic CRVO. Ischemic CRVO is more severe and can lead to neovascular glaucoma.
What causes CRVO?
CRVO is caused by several factors. These include age-related changes, high blood pressure, diabetes, and high cholesterol. Ocular and hematologic conditions also play a role.
How is CRVO diagnosed?
Diagnosing CRVO involves a detailed eye exam. This includes fundoscopy, fluorescein angiography, and OCT. Lab tests are also used to check for underlying conditions.
What are the treatment options for CRVO?
Treatment includes managing underlying conditions and using anti-VEGF injections. Corticosteroids and laser photocoagulation are also used to manage complications and improve vision.
Can CRVO be prevented?
While CRVO can’t be completely prevented, controlling risk factors helps. Making lifestyle changes and early detection can reduce the risk or lessen its impact.
What are the possible complications of CRVO?
Complications include neovascular glaucoma, persistent macular edema, and vision loss. This highlights the need for prompt treatment and ongoing management.
How is ischemic central retinal vein occlusion different from non-ischemic CRVO?
Ischemic CRVO has a more severe blockage, causing significant retinal ischemia. Non-ischemic CRVO has a better prognosis with less severe ischemia.
What is impending CRVO?
Impending CRVO is the early stage before a full CRVO. It’s when symptoms or signs of retinal venous congestion appear. This allows for early intervention.
References
National Health Service (NHS). Central Retinal Vein Occlusion: Signs, Causes, and Treatment. Retrieved from https://www.nhs.uk/conditions/retinal-vein-occlusion/