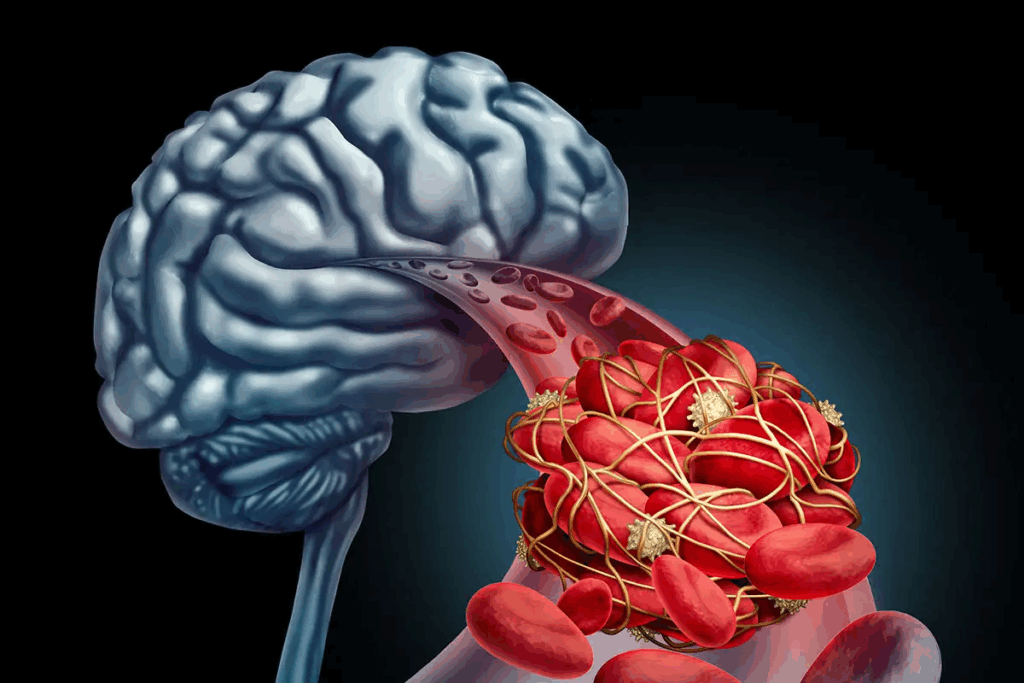
When a brain aneurysm is diagnosed, patients look for safe and advanced treatments. At Liv Hospital, we use a minimally invasive approach called brain aneurysm endovascular coiling. This method uses platinum embolism coils to stop blood flow to the aneurysm, preventing it from rupturing.
Our team of experts uses a small catheter to reach the aneurysm. They thread it into an artery and place coils or stents to hold the aneurysm in place. This endovascular coiling procedure is a groundbreaking option for treating aneurysms. It’s a less invasive choice compared to traditional surgery.
Understand the cerebral coiling procedure, its steps, and how it helps restore blood flow and prevent rupture.
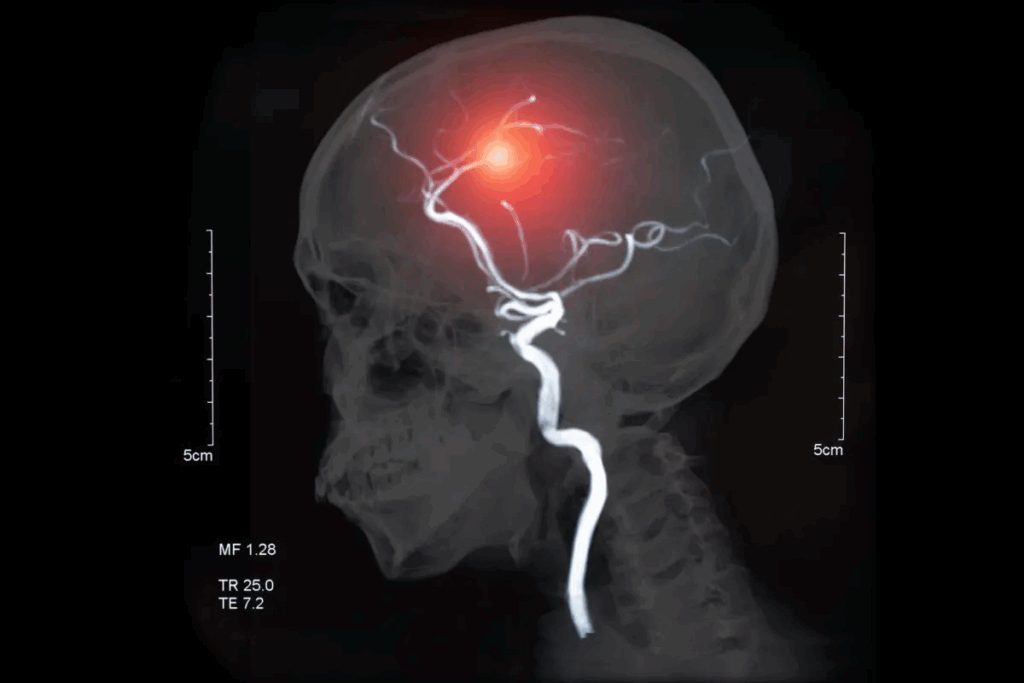
A brain aneurysm is a weak spot on an artery wall in the brain. It can cause serious health problems if not treated. Knowing about brain aneurysms helps us spot risks and avoid serious issues.
Brain aneurysms are abnormal blood vessel dilations in the brain. They can burst, causing bleeding in the brain. Most people don’t show symptoms until they burst, making early detection hard.
Several things can make an aneurysm more likely to burst. These include its size, where it is, and the person’s health. Smoking, high blood pressure, and a family history of aneurysms are big risk factors.
| Risk Factor | Description | Impact on Aneurysm Rupture |
| Size of Aneurysm | Larger aneurysms are more prone to rupture. | High |
| Location of Aneurysm | Aneurysms at certain locations are more likely to rupture. | Variable |
| Smoking | Smoking significantly increases the risk of rupture. | High |
| High Blood Pressure | Uncontrolled hypertension can increase rupture risk. | High |
| Family History | Having a family history of aneurysms may increase risk. | Moderate |
Finding and treating brain aneurysms early is key to avoiding rupture. This can greatly improve a patient’s chances of recovery.
We’ve covered the basics of brain aneurysms, their risks, and why early treatment is vital. People with risk factors should see a doctor for a check-up and treatment plan.
Endovascular coiling is a new way to treat brain aneurysms. It’s less invasive than old surgery methods. Doctors use it to fill the aneurysm with coils to stop it from bursting.
Coil embolization, or endovascular coiling, uses platinum coils to stop blood flow in aneurysms. It aims to prevent the aneurysm from bursting by blocking it and causing it to clot.
The idea of endovascular coiling started in the 1990s. It was seen as a safer option than traditional surgery. Over time, new coil designs and materials have made it even better. Now, it’s a common treatment for some brain aneurysms.
Endovascular coiling has big advantages over old surgery methods. It means less recovery time, less damage, and no open brain surgery. Unlike clipping, which opens the skull, coiling uses a small tube to reach the aneurysm.
Choosing between these treatments depends on the aneurysm and the patient’s health. The main benefits of endovascular coiling are:
We carefully check patients for coiling procedures. We look at their aneurysm and health. This helps us decide if coiling is right for them.
Some patients are perfect for coiling. They have small to moderate aneurysms. Their aneurysms also have a narrow neck and are easy to reach in the brain.
Also, those at high risk for surgery or who have had surgery before might choose coiling.
Coiling isn’t for everyone. Big or giant aneurysms, wide necks, and complex blood vessels are no-go’s. We check for risks and plan to avoid problems.
Imaging is key before coiling. We use digital subtraction angiography (DSA) and 3D rotational angiography. These help us understand the aneurysm’s shape, size, and where it is.
By carefully checking patients and their aneurysms, we find the best treatment. This leads to the best results.
The cerebral coiling procedure needs special equipment and materials. This ensures the best treatment for brain aneurysms. We use the latest technology and top-quality materials for the best results.
The angiography suite is key for cerebral coiling. It has a high-resolution imaging system for real-time views. This setup is clean and staffed by experts.
Catheterization tools help reach the aneurysm. We use guidewires, microcatheters, and guiding catheters. Choosing the right tools is vital for success.
Embolism coils are used to block the aneurysm. We have bare platinum and coated coils to help healing. The right coil depends on the aneurysm and patient.
Stents or balloon devices might be used too. They help keep the coil in place and block the aneurysm. Using these devices needs careful planning.
With advanced tools and the right materials, we can treat brain aneurysms well through cerebral coiling.
Getting ready for a cerebral coiling procedure is key. It includes several important steps. These steps make sure the patient knows what to expect and is ready for the treatment.
We start by teaching the patient about the cerebral coiling procedure. We cover its benefits, risks, and other options. This is important for getting informed consent, which is both legal and ethical.
We talk about possible problems like stroke or aneurysm rupture. We also explain how we’ll try to avoid these issues. And we discuss what happens after the procedure and follow-up care.
Anesthesia is vital for the success of the procedure. We look at the patient’s health and past medical history. This helps us choose the right anesthesia, like general or conscious sedation.
Our team works with anesthesiologists to keep the patient comfortable and safe. This teamwork is key for handling any anesthesia-related issues.
We use anticoagulation and antiplatelet therapy to prevent blood clots. The treatment plan depends on the patient’s risk factors and the aneurysm’s details.
| Medication | Dose | Purpose |
| Aspirin | 81 mg daily | Antiplatelet therapy |
| Clopidogrel | 75 mg daily | Antiplatelet therapy |
| Heparin | Bolus followed by infusion | Anticoagulation during procedure |
We manage the anticoagulation and antiplatelet therapy carefully. This balance helps avoid blood clots and bleeding problems.
The cerebral coiling procedure is a complex endovascular intervention. It needs precision and expertise. We will guide you through the critical steps involved in performing a cerebral coiling procedure.
Proper patient positioning is key for the success of the cerebral coiling procedure. We make sure the patient is comfortably positioned on the angiography table. Their head is secured in a neutral position.
A sterile field is then prepared around the femoral access site. We clean the area with antiseptic solutions and cover it with sterile drapes. This minimizes the risk of infection.
Access to the femoral artery is obtained using a percutaneous technique. We use ultrasound guidance to locate the femoral artery. This ensures accurate placement of the needle.
Once access is secured, a sheath is introduced. This allows for the passage of catheters and other devices necessary for the procedure.
Under fluoroscopic guidance, we navigate the catheter to the aneurysm site. This requires careful manipulation and precise control to avoid complications.
We use a combination of guidewires and catheters to reach the aneurysm. Techniques like roadmapping help in navigation.
Once the catheter is in place, we perform an angiographic assessment. We evaluate the aneurysm’s morphology and size. This involves injecting contrast material and capturing images using digital subtraction angiography.
We take precise measurements of the aneurysm’s dimensions. This includes its neck and dome. We determine the appropriate size and type of coils to be used.
The key steps outlined above are critical for the successful completion of a cerebral coiling procedure. By following these steps and using the right techniques and equipment, we can effectively treat brain aneurysms. This improves patient outcomes.
Complex aneurysms are tricky to treat. They need special strategies because of their unique shapes. We use advanced techniques to handle these cases.
Wide-necked aneurysms are hard to treat because they can’t be fully blocked without harming the main artery. We use stent-assisted coiling and balloon-assisted coiling to fix them. Stent-assisted coiling uses a stent to hold the coils in place. Balloon-assisted coiling uses a balloon to keep the coils from going into the main artery.
Choosing between these methods depends on the aneurysm’s size, neck width, and if there are branch vessels. We carefully look at these factors to pick the best treatment for each patient.
| Technique | Description | Advantages |
| Stent-Assisted Coiling | Deployment of a stent across the aneurysm neck to facilitate coil placement. | Provides a scaffold for coils, improving aneurysm occlusion. |
| Balloon-Assisted Coiling | Temporary balloon inflation to prevent coil protrusion into the parent vessel. | Enhances coil stability and promotes complete aneurysm occlusion. |
Large and giant aneurysms are big challenges. They are big and can have complex blood flow. We use flow diversion and parent artery occlusion to treat them.
Flow diversion uses a stent to change blood flow and help the aneurysm clot. Parent artery occlusion blocks the main artery to stop blood flow to the aneurysm. Sometimes, we also use bypass surgery.
Ruptured aneurysms need quick action to stop bleeding. We often use emergency coiling or clipping. Unruptured aneurysms can be treated more carefully, allowing for better planning.
When deciding how to treat an aneurysm, we consider its shape, the patient’s health, and the risk of rupture. For ruptured aneurysms, our main goal is to stop the bleeding fast.
During cerebral coiling, several challenges can pop up. These need quick and effective solutions. It’s key for operators to be ready to tackle them.
Coil migration is a big problem during cerebral coiling. It can block blood flow or cause blood clots. To fix this, we use different retrieval methods.
The right method depends on where the coil moved and the patient’s body. We might use a snare, a balloon, or a stent retriever.
Acting fast is vital to avoid more issues. We must carefully pick the best way to get the coil back.
Thromboembolic complications are another big challenge. They can happen because of the coil or blood stasis. We tackle these with medicine and mechanical tools.
Key strategies include:
Quickly spotting and treating these issues is key.
Aneurysm perforation is a serious issue during cerebral coiling. It needs immediate action to stop bleeding and prevent more harm. Our emergency plan includes:
Being ready and acting fast is essential to handle aneurysm perforation well.
Vasospasm can happen during or after cerebral coiling, often in those with subarachnoid hemorrhage. We watch the patient’s brain function and use imaging to spot vasospasm.
To treat vasospasm, we use:
Spotting and treating vasospasm early is vital to avoid brain damage.
The time after a procedure is very important. We need to take good care and watch closely to avoid problems. When the patient leaves the procedure room, we focus on helping them recover safely and smoothly.
Right after the procedure, we keep a close eye on the patient’s health. We check their blood pressure and how their brain is working. We also watch for any signs of trouble like blood clots or swelling in the blood vessels.
Good care right away helps the patient recover well. We make sure they are comfortable and manage any pain they might have.
Checking the brain’s health is key after a procedure. Our plan includes:
These checks help us spot any brain changes or problems early. This way, we can act fast if needed.
We use special medicine to stop blood clots from forming. The exact plan depends on the patient and the procedure. Our steps include:
Following the medicine plan is very important. It helps lower the risk of serious problems.
Before the patient goes home, we give them lots of information. This includes:
We think it’s important to teach patients about their care. This way, they can take good care of themselves at home.
After a cerebral coiling procedure, patients need careful follow-up and long-term management. This ensures the best results. It’s important to watch the treated aneurysm and handle any complications that might come up.
Having a set imaging follow-up schedule is key. We suggest the first check-up within 6 to 12 months after the procedure. Then, we recommend regular follow-ups. The choice of imaging, like digital subtraction angiography (DSA) or magnetic resonance angiography (MRA), depends on the aneurysm and the patient’s health.
We watch for coil compaction or recanalization during follow-up. Coil compaction means the coils get too close together, which can cause the aneurysm to grow back. Recanalization is when blood flow starts again in the aneurysm. Catching these problems early is key to avoiding serious issues.
If imaging shows coil compaction or recanalization, we might need to treat again. We look at many things when planning the next step, like the aneurysm’s shape and the patient’s health. Retreatment options could be more coiling, stent-assisted coiling, or even flow diversion.
Managing patients long-term after cerebral coiling needs a team effort. Neurosurgeons, neuroradiologists, and other experts all play a part. By keeping a close eye on patients and acting fast, we can make sure they do well and avoid problems.
Endovascular coiling has changed how we treat brain aneurysms. It’s a less invasive method with big benefits. It’s more popular than old surgery methods because it works well.
Many studies show endovascular coiling works great for brain aneurysms. It has high success rates, with many patients seeing their aneurysms fully closed. It’s very effective for certain types of aneurysms, like small-necked ones.
Table: Success Rates of Endovascular Coiling
| Aneurysm Type | Success Rate (%) | Complication Rate (%) |
| Small-necked | 85 | 5 |
| Wide-necked | 75 | 10 |
| Ruptured | 80 | 15 |
Endovascular coiling is less invasive, leading to a quicker recovery. Patients feel less pain and can get back to their lives faster. This is a big plus for those wanting a quick recovery.
The endovascular method has many advantages. It’s safer, causes less brain damage, and can treat hard-to-reach aneurysms. These benefits make it a good choice for many patients.
Long-term studies show endovascular coiling can keep aneurysms closed for a long time. While results vary, they’re mostly good. We keep watching patients to see how well it works over time.
In summary, endovascular coiling is a top choice for treating brain aneurysms. It has many benefits and a strong success rate. As we get better at it, we expect even better results for patients.
We’ve looked into the cerebral coiling procedure for treating brain aneurysms. It’s safe and effective, with benefits like a small incision and quick recovery. This method has changed how we handle brain aneurysms, giving patients a new option instead of old surgeries.
The procedure uses a catheter to reach the aneurysm. There, coils block the aneurysm to stop bleeding. Knowing how it works helps doctors understand brain aneurysm treatment better.
In summary, the cerebral coiling procedure is key in treating brain aneurysms. It offers patients a good chance of success with little risk. As we keep improving this method, we’ll make patient care even better for brain aneurysm treatment.
Cerebral coiling, also known as endovascular coiling, is a minimally invasive procedure. It uses platinum embolism coils to block blood flow to a brain aneurysm. This prevents rupture and promotes clotting within the aneurysm.
Endovascular coiling has many benefits. It’s less invasive than open surgery, which means less risk of complications. It also has a shorter recovery time. Plus, it can treat aneurysms that are hard to access surgically.
Cerebral coiling carries some risks. These include coil migration, thromboembolic complications, aneurysm perforation, and vasospasm. But, these risks are low with experienced practitioners.
Patient selection is based on several factors. The size, shape, and location of the aneurysm are evaluated. So is the patient’s overall health and medical history. This helps determine if they’re a good candidate for endovascular coiling.
Imaging is key in pre-procedure evaluation. It helps characterize the aneurysm and assess its morphology. It also helps plan the best treatment strategy.
After cerebral coiling, follow-up care is important. It involves regular imaging studies. These studies monitor the aneurysm’s occlusion status and check for coil compaction or recanalization. They also determine if retreatment is needed.
Endovascular coiling is very effective in treating brain aneurysms. It has high success rates and low complication rates. But, long-term results can vary based on individual factors.
The recovery timeline for cerebral coiling is shorter than for open surgery. Most patients can resume normal activities within a few days to weeks after the procedure.
Yes, cerebral coiling can treat complex or ruptured aneurysms. These cases may need specialized techniques and adjunctive devices for the best results.
Long-term outcomes for patients treated with cerebral coiling are generally good. There are high rates of aneurysm occlusion and low rates of recurrence. But, ongoing monitoring is necessary to ensure the best results.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us