Last Updated on November 26, 2025 by Bilal Hasdemir
For those looking to ease neck and arm pain, knowing about cervical epidural steroid injection is key. At Liv Hospital, we offer trusted, patient-focused care. We make sure you get the safest, latest treatments for cervical spine injections.
Cervical epidural steroid injections are a non-surgical way to treat neck pain. They inject corticosteroid medication into the epidural space of the cervical spine. This helps manage chronic pain from nerve root irritation and inflammation in the neck.
Patients need to understand the procedure and needle size before treatment. These injections aim to cut down inflammation and ease pain by delivering corticosteroid medication directly to the epidural space.
Key Takeaways
- Understanding the procedure and needle size is key for patients considering cervical epidural steroid injections.
- Cervical epidural steroid injections are a non-surgical way to manage chronic neck pain.
- The procedure involves injecting corticosteroid medication into the epidural space.
- Liv Hospital offers patient-centered care for cervical spine injections.
- Corticosteroid medication helps reduce inflammation and ease pain.
What Are Cervical Epidural Steroid Injections?
Cervical epidural steroid injections put medicine right next to the spinal cord in the neck. They help treat neck pain and swelling.
Definition and Therapeutic Purpose
These injections put corticosteroid medicine into the epidural space. This space is around the spinal cord in the neck. The goal is to lessen swelling and pain.
The medicine used is strong against inflammation. It’s meant to calm down the spinal nerves. This helps ease long-term neck pain and other symptoms.
Anatomy of the Cervical Epidural Space
The cervical epidural space is between the vertebrae and the dural sac. It has fatty tissue, blood vessels, and nerves. Knowing this area well is key to safe and effective injections.
| Anatomical Structure | Description | Relevance to CESI |
| Cervical Epidural Space | Potential space between the vertebrae and the dural sac | Target area for corticosteroid injection |
| Spinal Nerves | Nerves emerging from the spinal cord | Compression or irritation can cause pain |
| Fatty Tissue | Adipose tissue within the epidural space | Cushions the nerves and spinal cord |
Historical Development of the Procedure
Epidural steroid injections started in the early 20th century. Over the years, they’ve improved with better imaging and understanding of the spine. Now, they’re done with fluoroscopy for better accuracy and safety.
With ongoing tech advancements, the procedure is getting even better. It’s now a more reliable way to treat chronic neck pain.
Common Conditions Treated with Cervical ESI
Cervical epidural steroid injections (CESI) are key for treating many cervical spine issues. They help with conditions like cervical spondylosis, herniated discs, and radiculopathy. These injections ease pain and swelling.
Cervical Radiculopathy and Nerve Root Compression
Cervical radiculopathy causes neck and arm pain, numbness, or weakness. It’s often due to nerve root compression or swelling. CESI delivers corticosteroids to the affected area. This reduces swelling and eases nerve root pressure.
Studies show CESI is effective for cervical radiculopathy. It targets the pain source, giving patients much-needed relief and improving their quality of life.
Cervical Spondylosis and Degenerative Changes
Cervical spondylosis is when the cervical spine wears down over time. It can cause neck pain, stiffness, and less mobility. CESI helps manage these symptoms by reducing swelling and easing pain.
| Condition | Symptoms | Treatment with CESI |
| Cervical Radiculopathy | Pain, numbness, and weakness in the neck and arm | Reduces inflammation, relieves nerve compression |
| Cervical Spondylosis | Pain, stiffness, reduced mobility | Reduces inflammation, relieves pain |
| Herniated Discs | Pain, numbness, tingling in the neck and arm | Reduces inflammation, relieves pressure on discs |
Herniated Discs in the Cervical Region
Herniated discs in the cervical spine can cause a lot of pain and discomfort. This pain often spreads to the arms. CESI treats herniated discs by reducing swelling and easing nerve pressure.
Using CESI for herniated discs is great because it’s a less invasive option. It offers patients a faster recovery and lowers the risk of complications compared to surgery.
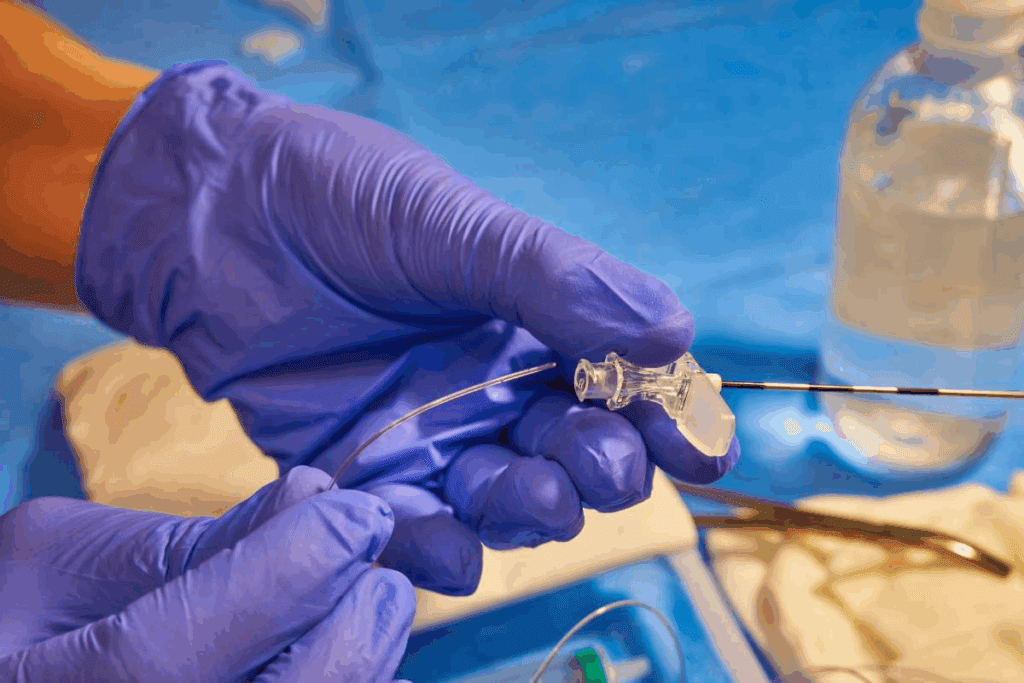
Cervical Epidural Steroid Injection Needle Size: What You Need to Know
The size of the needle used in cervical epidural steroid injections is key. It affects how well the procedure works and how safe it is. Finding the right needle size is important for both the success of the treatment and the comfort of the patient.
Standard Needle Gauge Ranges
Needles for these injections usually range from 22 to 25 gauge. This size is chosen to ensure the medication is delivered accurately while keeping the patient comfortable.
The gauge of the needle is the opposite of its diameter. A higher gauge means a thinner needle. A thinner needle is better because it causes less damage to tissues. This can help reduce pain for the patient after the procedure.
Balancing Precision and Patient Comfort
Finding the right balance between precision and comfort is essential. A needle that’s too big can be uncomfortable and cause more damage. On the other hand, a needle that’s too small might not be stable enough for precise delivery.
When picking a needle size, we look at several things. These include the patient’s body, the condition being treated, and the injection technique.
How Needle Size Affects Medication Delivery and Tissue Trauma
The needle size used in these injections affects how well the medication is delivered and how much tissue damage occurs. The right size needle ensures the medication reaches the right spot with minimal damage to nearby tissues.
| Needle Gauge | Precision Level | Patient Comfort Level |
| 22 Gauge | High | Moderate |
| 23 Gauge | High | High |
| 24 Gauge | Very High | High |
| 25 Gauge | Very High | Very High |
Understanding how needle size affects both the delivery of medication and patient comfort helps healthcare providers make better choices. This can lead to better results from cervical epidural steroid injections.
Advanced Techniques in Cervical Epidural Steroid Injection
Modern techniques have made cervical epidural steroid injections more precise. This has led to better treatment for various cervical spine issues. We’ll look at the advanced methods used, focusing on the interlaminar and transforaminal approaches.
Interlaminar Approach: Technique and Applications
The interlaminar approach injects steroids into the epidural space. It’s done through the space between the C7 and T1 vertebrae. This method is great for treating conditions that affect many nerve roots or need to cover a wide area of the cervical spine.
Key aspects of the interlaminar approach include:
- Precise needle placement under fluoroscopic guidance
- Use of a loss-of-resistance technique to confirm epidural space entry
- Injection of corticosteroids to reduce inflammation and relieve pain
Transforaminal Approach: Targeted Delivery Method
The transforaminal approach injects steroids directly into the neural foramen. It targets the specific nerve root affected. This method is very effective for treating cervical radiculopathy caused by nerve root compression.
The benefits of the transforaminal approach include:
- Targeted delivery of medication to the affected nerve root
- Potential for faster and more effective pain relief
- Reduced risk of complications compared to other approaches in some cases
Comparing Efficacy and Safety Profiles of Different Approaches
Both the interlaminar and transforaminal approaches have their own strengths and weaknesses. We compare them to find the best technique for each patient.
| Approach | Efficacy | Safety Profile |
| Interlaminar | Effective for the broad coverage of the cervical spine | Generally safe, but risk of dural puncture |
| Transforaminal | Highly effective for targeted nerve root treatment | The risk of intravascular injection requires a precise technique |
Understanding the benefits and risks of each approach helps healthcare providers choose the best treatment for patients. This ensures the most effective and safe treatment for cervical epidural steroid injections.
The Critical Role of Fluoroscopic Guidance
Fluoroscopic guidance is key in making cervical epidural steroid injections safer and more effective. It helps place the needle exactly right. This is vital for the medicine to work well and to avoid risks.
Benefits of Real-time Imaging During Injection
Fluoroscopic guidance gives us real-time imaging during injections. This lets doctors see where the needle is and how the contrast spreads. It’s important to make sure the medicine goes to the right spot for the best results.
With real-time imaging, doctors can adjust the needle as they go. This is very important in the neck area because it’s complex and there’s little room for mistakes.
Reducing Procedural Risks Through Precise Visualization
Fluoroscopic guidance is great at lowering the risks of the procedure. It gives a clear view of where the needle is going and what’s around it. This helps doctors avoid problems like hitting a blood vessel or irritating a nerve.
Also, using contrast material lets doctors see if the medicine is going into a blood vessel or not. This means they can fix any issues right away. This level of detail makes cervical epidural steroid injections much safer.
Alternative Imaging Modalities in Cervical ESI
Even though fluoroscopy is the top choice for cervical epidural steroid injections, other methods like ultrasound and MRI are being looked at, too. Ultrasound guidance is good because it shows what’s happening in real-time without using X-rays. But it depends a lot on the skill of the person using it.
MRI guidance is great for seeing soft tissue,s but it’s more complicated and expensive. The choice of imaging method depends on the situation, what’s available, and what the doctor prefers.
Medication Formulations Used in Cervical ESI
The success of cervical ESI procedures depends on the medications used. Corticosteroids and local anesthetics are key. They help provide both quick and lasting pain relief for patients.
Types and Properties of Corticosteroids
Corticosteroids are vital in cervical ESI. They fight inflammation, easing pain and swelling in the cervical spine. The most used corticosteroids are:
- Triamcinolone: It has strong anti-inflammatory effects.
- Methylprednisolone: It’s effective in reducing inflammation.
- Dexamethasone: It works fast and is very potent.
These steroids differ in strength, how long they last, and side effects. The right one depends on the patient’s and the doctor’s choice.
Local Anesthetics: Immediate Pain Relief Agents
Local anesthetics are used with corticosteroids for quick pain relief. They include:
- Lidocaine: It works fast and numbs the area well.
- Bupivacaine: It lasts longer, providing more pain relief.
Local anesthetics help reduce pain during and after the procedure. They make the treatment more effective.
Combination Therapy: Balancing Short and Long-term Effects
Using both corticosteroids and local anesthetics in cervical ESI is beneficial. Corticosteroids fight inflammation for long-term relief. Local anesthetics provide quick pain relief during and after the procedure. This mix:
- Improves pain management
- Reduces discomfort during the procedure
- Enhances both short and long-term results
Healthcare providers choose and mix these medications carefully. They tailor the treatment to each patient’s needs, making cervical epidural steroid injections more effective.
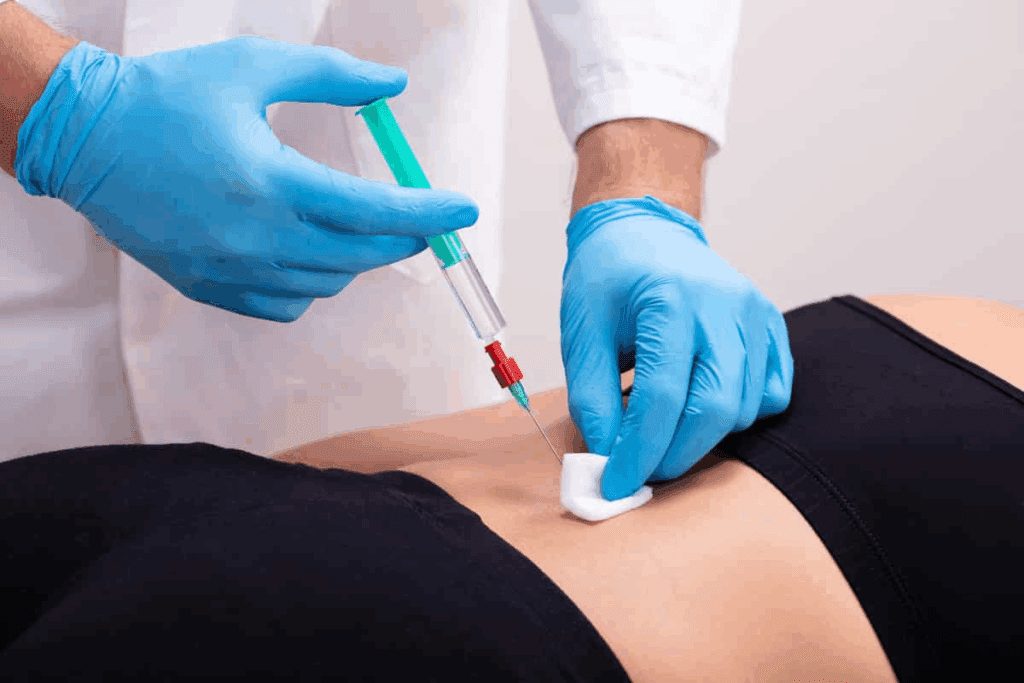
The Complete Cervical Epidural Steroid Injection Procedure
Getting a cervical epidural steroid injection is a detailed process. It’s done under fluoroscopic guidance to place the steroid correctly. This ensures the treatment is safe and effective.
Pre-procedure Assessment and Patient Preparation
We start by checking the patient’s medical history and current health. We look at imaging studies and talk about any allergies or sensitivities to medications.
- Review of medical history and current medications
- Discussion of possible risks and benefits
- Getting informed consent
- Preparing the injection site
Positioning, Sterilization, and Local Anesthesia
Getting the patient in the right position is key to success. We make sure they’re comfortable and the cervical spine is easy to reach.
Sterilization and local anesthesia are important:
- The skin is cleaned with an antiseptic solution.
- A local anesthetic is given to reduce pain.
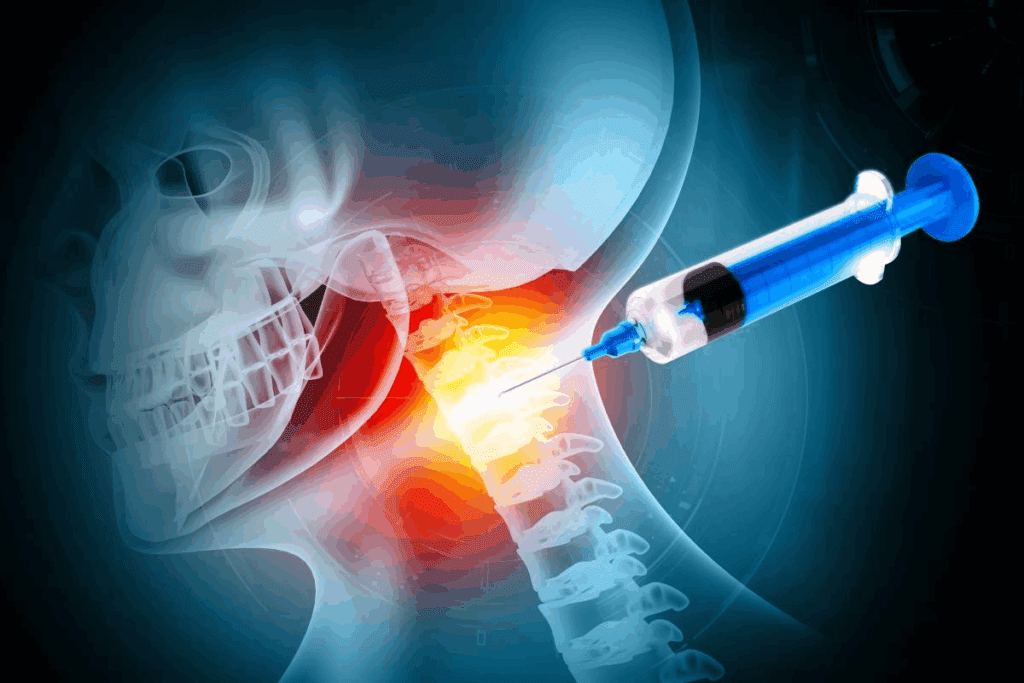
Needle Insertion Technique and Medication Delivery
The needle insertion needs precision and skill. We use fluoroscopic guidance to place the needle correctly in the epidural space.
Then, the medication is delivered to the right area:
- Corticosteroids help reduce inflammation and swelling.
- Local anesthetics give immediate pain relief.
Post-procedure Monitoring and Care Instructions
After the procedure, we watch for any immediate reactions or problems. We give patients care instructions to help them recover smoothly.
Important post-procedure instructions are:
- Avoiding hard activities for a while.
- Watching for signs of infection or other issues.
- Going to follow-up appointments to check how the treatment is working.
Safety Profile: Risks and Complications
Cervical epidural steroid injections are generally safe but can have risks and complications. Both doctors and patients need to know about these to ensure safe treatment and good results.
Common Side Effects and Their Management
Side effects of these injections include pain or discomfort at the site, facial flushing, and trouble sleeping. These usually go away on their own. But some people might see bigger issues like higher blood sugar or mood swings. Teaching patients well and taking care of them after the procedure can help lessen these problems.
To deal with common side effects well, we suggest:
- Keeping a close eye on blood sugar in diabetic patients
- Helping with insomnia and mood changes
- Teaching ways to manage pain at the injection site
Serious Complications: Recognition and Prevention
Though rare, serious issues like infection, nerve damage, and allergic reactions can happen. It’s key to spot and handle these problems quickly. For example, if you have a fever, more pain, or redness at the site, get it checked right away.
To lower the chance of serious problems, we follow strict cleaning techniques and check patients for any reasons they shouldn’t get the injection. Using X-ray guidance helps us aim better, which cuts down the risk of nerve damage.
Patient Selection: Contraindications and Special Considerations
Picking the right patients is key to avoiding risks with cervical epidural steroid injections. You shouldn’t get it if you have an active infection, bleeding problems, or allergies to the drugs. People with diabetes or past mental health issues need extra care because steroids can affect blood sugar and mood.
We also look at the patient’s health overall, including past surgeries or spine problems. Doing a detailed check before the procedure helps us make it safer and more effective for each person.
Conclusion: Efficacy and Future Directions in Cervical Spine Interventions
Cervical epidural steroid injections are a key treatment for chronic neck pain. They work by putting corticosteroids into the epidural space. This can greatly reduce pain and enhance a patient’s quality of life.
Research supports the effectiveness of these injections for conditions like cervical radiculopathy and herniated discs. The use of fluoroscopic guidance makes the procedure safer. It ensures the needle is placed accurately, reducing risks.
As we learn more, we’ll see new techniques and medications for cervical spine treatments. Adding cervical epidural injections to treatment plans is a promising step. It helps meet the complex needs of patients with chronic neck pain. This approach can lead to better outcomes and improved lives for those affected.
FAQ
What is a cervical epidural steroid injection?
This procedure involves putting corticosteroid medication into the space around the spinal nerves in the neck. It helps reduce inflammation and eases pain.
What conditions are treated with cervical epidural steroid injections?
It treats conditions like cervical radiculopathy, herniated discs, and degenerative disc disease. These cause chronic neck pain.
What is the typical needle size used for cervical epidural steroid injections?
The needles used are usually between 22-25 gauge. This size is precise yet comfortable for the patient.
How does needle size affect the delivery of medication in cervical epidural steroid injections?
Smaller needles might cause less trauma but need more skill. Larger needles are easier to use but might be more uncomfortable.
What are the different approaches used in cervical epidural steroid injections?
There are two main approaches: interlaminar and transforaminal. Each has its own method, use, and safety level.
Why is fluoroscopic guidance important in cervical epidural steroid injections?
It uses real-time imaging to guide the needle. This reduces risks by ensuring accurate placement and delivery.
What medications are used in cervical epidural steroid injections?
Corticosteroids and local anesthetics are used together. They help with both short-term and long-term pain relief.
What are the common side effects of cervical epidural steroid injections?
Side effects include temporary pain or discomfort at the site. Serious complications are rare but should be discussed with a doctor.
Are there any contraindications for cervical epidural steroid injections?
Yes, some conditions or situations may not be suitable. A doctor will assess each case to determine if it’s safe.
What can I expect during a cervical epidural steroid injection procedure?
The procedure includes preparation, positioning, and sterilization. It also involves local anesthesia, needle insertion, and medication delivery. Afterward, you’ll be monitored and given care instructions.
How do cervical epidural steroid injections fit into the management of chronic neck pain?
They are a valuable treatment for chronic neck pain. They offer a potentially effective way to relieve pain caused by various conditions.
References
- Benzon, H. T., Huntoon, M. A., Rathmell, J. P., & American Academy of Neurology (AAN) Panel. (2023, December). Epidural Steroids for Cervical and Lumbar Radicular Pain: A Systematic Review and Meta-Analysis. Neurology. https://pubmed.ncbi.nlm.nih.gov/39938000/
- Epstein, N. E. (2018). Major risks and complications of cervical epidural steroid injections. Surgical Neurology International, 9, 86. https://surgicalneurologyint.com/wp-content/uploads/2018/04/8843/SNI-9-86.pdf
- Narayanaswami, P. (2024, March 29). A new systematic review summarizes the efficacy of epidural spinal injections for chronic back pain. Practical Neurology. https://practicalneurology.com/news/a-new-systematic-review-summarizes-the-efficacy-of-epidural-spinal-injections-for-chronic-back-pain/2473789/
- Benyamin, R., Singh, V., Parr, A. T., Conn, A., Diwan, S., & Abdi, S. (2009). Systematic review of the effectiveness of cervical epidurals in the management of chronic neck pain. Pain Physician, 12(1), 137-157. https://painphysicianjournal.com/current/pdf?article=MTE3NQ%3D%3D&journal=47