Diagnosing heart failure needs a deep look at breath and heart CHF lung sounds. At Liv Hospital, we focus on care that checks every detail of these important signs.
Learn about CHF lung sounds and what they reveal about heart failure conditions.
Heart failure happens when the heart can’t pump enough blood. Congestive heart failure lung sounds show this problem, with fine crackles being a key sign.
We will look at the 7 key heart failure lung sounds that give us important clues about heart failure. Knowing these sounds helps us diagnose and treat congestive heart failure better.
Heart failure affects lung function, leading to specific breath sounds doctors can recognize. Congestive Heart Failure (CHF) means the heart can’t pump enough blood. This leads to changes in lung function and distinct lung sounds.
When the heart can’t pump well, blood backs up in the lungs. This high pressure pushes fluid into the alveoli, causing pulmonary edema. Pulmonary edema is a key sign of CHF and changes breath sounds.
Fluid in the lungs causes inflammation and irritation. This leads to symptoms like shortness of breath and coughing. These symptoms are linked to the lung sound changes doctors listen for.
The link between heart function and lung sounds is complex. As CHF worsens, the heart’s pumping gets worse. This increases lung pressure, causing fluid to leak into the alveoli.
This fluid buildup changes breath sounds, often causing crackles or rales. Doctors listen to these sounds to understand CHF’s severity and treatment success. For example, fine crackles at the lung bases might show early congestion.
Changes in respiratory sounds over time offer insights into disease progression or improvement. This shows why regular monitoring is key in managing CHF.
Diagnosing heart failure well depends on learning auscultation techniques. These skills help detect small changes in breath and heart sounds. Healthcare professionals need to master these skills to manage heart failure well.
Getting the best sound is key. When checking for heart failure, focus on areas where sounds are loudest.
How the patient sits affects sound detection. Changing their position can reveal hidden sounds.
Key positioning techniques include:
Using the right stethoscope placement and patient positioning helps doctors detect heart failure sounds better. This leads to more accurate diagnoses and timely treatments.
When checking patients with heart failure, fine crackles are key. They show up as high-pitched sounds during late inspiration, mainly at the lung bases. These sounds happen when small airways open up because of fluid or inflammation.
Fine crackles sound high-pitched and come during late inspiration. They’re like Velcro being pulled apart. Finding them means the lungs are full of fluid, a sign of heart failure. The timing and how they sound can tell us a lot about the problem.
These sounds happen when small airways open up because of fluid or inflammation. This usually happens in lung problems like pulmonary edema, linked to heart failure.
In early heart failure, fine crackles are heard at both lung bases. This is called bibasilar. It’s because fluid settles at the bases due to gravity. The bibasilar pattern is a key sign of early heart failure.
As heart failure gets worse, fine crackles spread to more areas. They can move up to the mid and upper lung zones. Watching how and where fine crackles appear helps track heart failure’s progress and treatment success.
Advanced CHF is marked by coarse crackles, which are louder and deeper than fine crackles. These sounds are key indicators of the disease’s worsening. As CHF gets worse, lung sounds change a lot, showing the disease’s effects.
Coarse crackles are different from fine crackles in several ways. They are louder, deeper, and last longer. Unlike fine crackles, which are heard late in breathing, coarse crackles can be heard all through breathing. This difference is key for doctors to know how severe CHF is.
Coarse crackles often mean more severe lung fluid buildup in CHF patients. Their presence shows the disease has moved past the early stages, where fine crackles are more common.
Widespread crackles, including both fine and coarse, show extensive lung involvement. When crackles are heard on both sides and are widespread, it means a lot of fluid in the lungs. This is a sign of advanced disease and a higher risk of serious problems.
The move from fine to coarse crackles, or having both, means the patient’s condition is getting worse. It’s vital for healthcare providers to watch these changes closely. They have big implications for managing the disease and planning treatment.
Understanding the difference between coarse and fine crackles helps doctors better judge CHF’s stage and severity. This knowledge helps in making the right treatment choices and tailoring care to each patient’s needs.
Cardiac wheeze is a unique sound caused by fluid buildup in the bronchial walls due to heart failure. It can be hard to tell apart from other breathing problems. We’ll look into why wheezing happens in heart failure and how to tell it apart from other wheezing sounds.
Wheezing in heart failure comes from bronchial edema. This is when fluid gathers in the bronchial walls. It makes the airways narrow, leading to the wheezing sound we hear.
The heart’s problem in pumping blood causes this fluid buildup. It leads to congestion in the lungs.
Telling cardiac wheeze apart from asthma or COPD is key for the right treatment. Cardiac wheeze often shows signs of heart failure like orthopnea and paroxysmal nocturnal dyspnea. Asthma and COPD usually have a history of breathing issues and different lung scans.
We use a mix of medical history, physical checks, and tests like echocardiography and spirometry. This helps us figure out the cause of wheezing.
Rhonchi and gurgling sounds are important signs of fluid overload in CHF patients. These sounds show how severe the congestion is. They give valuable insights into the patient’s health.
Rhonchi are low-pitched, snoring sounds caused by airway blockage. In CHF patients, these sounds happen during breathing in and out. They show a lot of fluid in the airways.
Rhonchi and gurgling sounds in CHF patients mean fluid overload. This might need changes in treatment. Diuretic therapy might need to be stronger to reduce fluid and ease symptoms.
These sounds also mean the patient needs closer watch. Healthcare providers should check lung sounds, fluid levels, and overall health often. Paying attention to these sounds helps improve patient care.
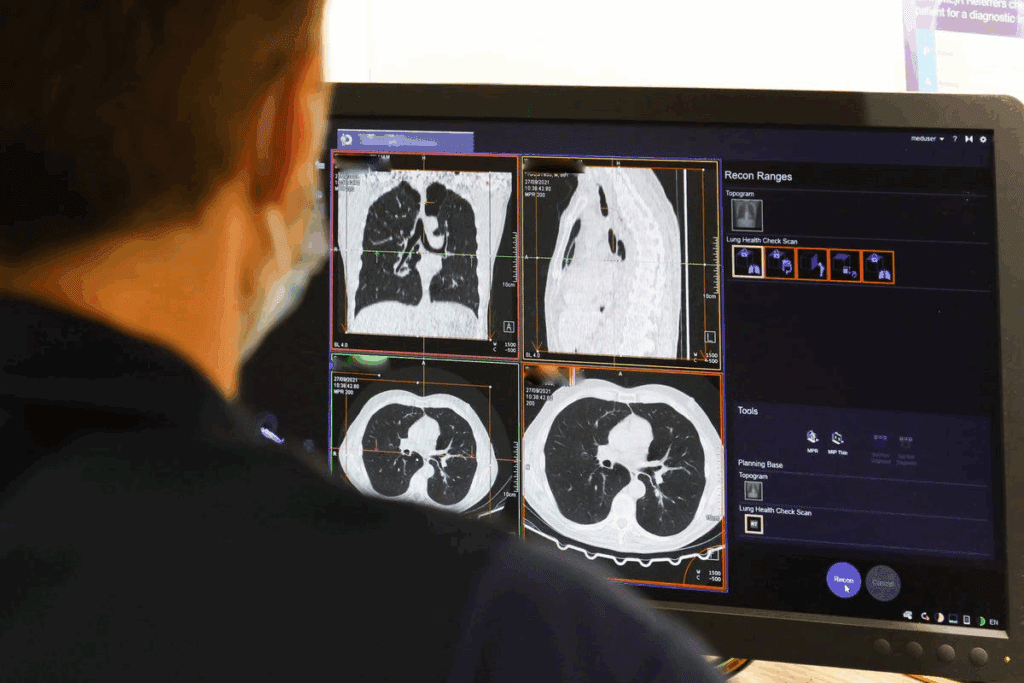
Pleural effusion, a common complication of CHF, often shows as diminished breath sounds during auscultation. This finding is important and needs careful checking. It can mean there’s fluid in the pleural space.
When checking patients with CHF, we must watch for changes in breath sounds. These changes can show how the patient’s condition is changing. Diminished breath sounds are key, as they might mean there’s fluid in the pleural space.
Finding pleural fluid buildup is key for diagnosing and treating CHF. We use clinical checks and imaging to spot pleural effusion. Listening with a stethoscope is important, as it often shows the first sign of fluid.
To find pleural fluid buildup, we should:
As pleural effusion grows, we notice different sounds when listening with a stethoscope. These changes help us understand how the condition is getting worse and guide treatment.
| Clinical Finding | Acoustic Change | Clinical Significance |
| Diminished Breath Sounds | Reduced intensity of breath sounds | Indicates pleural fluid accumulation |
| Pleural Rub | Grating or rubbing sound | May indicate pleurisy or inflammation |
| Auscultatory Percussion | Dullness on percussion | Confirms presence of pleural fluid |
Knowing these sound changes is vital for treating CHF well. By spotting signs like diminished breath sounds, we can act quickly to help patients.
In patients with CHF, the S3 gallop is a key sign of ventricular dysfunction. This sound happens early in diastole, right after the second heart sound. It’s a key finding in diagnosing heart failure.
The S3 gallop, or third heart sound, is a low sound. It’s best heard with the bell of the stethoscope at the heart’s apex. It sounds like “lub-dub-ta,” with the “ta” being the S3 sound.
To hear it well, patients should lie on their left side. This brings the heart closer to the chest.
Clinical Tip: The S3 gallop is louder during breathing in. It’s also more noticeable when you squat or raise your legs.
An S3 gallop means the ventricle is filling too fast. It shows the ventricle is under too much pressure and volume. This leads to rapid filling in early diastole.
| Clinical Feature | Description | Implication |
| S3 Gallop Presence | Indicates rapid ventricular filling | Ventricular dysfunction |
| Timing | Early diastole, after S2 | Increased filling pressures |
| Best Heard | Apex, with bell of stethoscope | Optimal auscultation technique |
The S3 gallop is a key tool in diagnosing CHF. It helps doctors spot patients with serious ventricular problems. This guides treatment and management plans.
Lung sounds in CHF patients change a lot as the disease gets worse. These changes are key for doctors to watch, as they show how the disease is moving and if treatments are working. Knowing how CHF lung sounds change helps doctors adjust treatment plans.
In the early stages of CHF, lung sounds might seem normal or show small changes. Fine crackles, or rales, are often the first sign of fluid in the lungs. These high-pitched sounds are heard during late inspiration and are usually found at the lung bases.
Fine crackles mean fluid is starting to build up in the lungs, a sign of CHF. As the disease gets worse, these sounds get louder and spread out more.
When CHF gets to a moderate stage, lung sounds get louder and spread out more. Coarse crackles may show up, meaning more fluid is building up. These sounds are louder and more musical, lasting through inspiration.
Patients might also start to hear cardiac wheezing, a sign of swelling in the bronchial tubes. This wheezing is different from asthma or COPD because it comes with other CHF symptoms and gets better with diuretics.
In the final stages of heart failure, lung sounds can be very dramatic. Rhonchi and gurgling sounds may appear because of a lot of fluid in the airways. These sounds are scary and often mean the patient is having a hard time breathing.
Pleural effusion, a common problem in advanced CHF, can cause diminished breath sounds in certain areas. Doctors need to watch for these changes, as they show the disease is getting much worse.
By keeping an eye on lung sound changes in CHF, doctors can manage the disease better and help patients get better.
Understanding congestive heart failure lung and heart sounds is key for top-notch patient care. Recognizing these sounds helps us see how severe and how fast the condition is getting worse.
Using these sounds well lets doctors and nurses spot and handle CHF better. We can tell when a patient needs a change in treatment to feel better and slow the disease down.
Being able to tell apart different sounds like fine crackles, coarse crackles, and cardiac wheeze helps us treat each patient uniquely. This way, we can make their lives better and their health outcomes better too.
As we learn more about heart failure sounds, we can give patients with CHF even better care. This leads to better health and happiness for our patients.
Congestive heart failure can cause many lung sounds. These include fine crackles, coarse crackles, and cardiac wheeze. You might also hear rhonchi and gurgling sounds. Diminished breath sounds can also occur due to fluid buildup.
Fine crackles are a key sign of pulmonary edema in heart failure. They are high-pitched and heard during late inspiration. They often appear bibasilar, showing fluid in the lungs.
Fine crackles are high-pitched and early signs of heart failure. Coarse crackles are louder and more widespread. They show more severe disease and edema.
Cardiac wheeze is caused by bronchial edema in heart failure. It’s different from asthma or COPD wheezing. It often comes with other heart failure signs.
Rhonchi and gurgling sounds in CHF patients show fluid overload. Rhonchi is a low-pitched wheezing sound. Gurgling sounds suggest a lot of fluid in the airways.
Diminished breath sounds in CHF often mean pleural effusion. This is fluid between the lung and chest wall. It affects lung expansion and breathing.
An S3 gallop is a heart sound in CHF. It happens shortly after the second heart sound. It shows rapid ventricular filling and ventricular dysfunction.
As CHF gets worse, lung sounds change. They might go from fine crackles to coarse crackles. Other sounds like rhonchi and gurgling may also appear. This shows worsening edema and fluid overload.
Knowing CHF lung and heart sounds is key for diagnosing and managing heart failure. It helps healthcare professionals see how severe the disease is. They can then adjust treatment plans.
Using the right stethoscope placement and patient position is vital. It helps healthcare professionals accurately diagnose and assess CHF.
Cardiac function and respiratory sounds in CHF are closely linked. Poor cardiac function leads to pulmonary congestion. This affects respiratory sounds and gives important diagnostic clues.
National Center for Biotechnology Information. (2025). 7 Key CHF Lung Sounds What Breath and. Retrieved from https://pubmed.ncbi.nlm.nih.gov/30344929/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us