Last Updated on November 20, 2025 by Ugurkan Demir

Medical treatments have greatly improved for kids with leukemia. Thanks to top care from specialized centers, the five-year survival rate is now over 85 percent for many.
It’s key for parents to know the latest survival statistics when dealing with this diagnosis. Different leukemia types have different survival chances. Knowing this helps families make informed choices.
Key Takeaways
- The overall five-year survival rate for childhood leukemia has surpassed 85 percent.
- Different types of leukemia have varying survival rates.
- Advances in medical treatment have improved the outlook for children with leukemia.
- Specialized care centers play a critical role in boosting survival rates.
- Understanding current survival statistics is vital for making informed decisions.
The Remarkable Progress in Childhood Leukemia Survival
Childhood leukemia used to be almost always fatal. But now, thanks to medical research and new treatments, survival rates have greatly improved. This shows how far we’ve come in understanding and treating this disease.
Historical Perspective on Childhood Leukemia Treatment
In the old days, leukemia was a death sentence for kids. Before the 1970s, only about 10% of kids with leukemia lived five years after being diagnosed. Back then, treatments were few, and the disease was a mystery.
Chemotherapy came along in the mid-1900s and changed everything. It was the start of a new chapter in fighting leukemia. Many studies and trials have led to better, safer treatments.
Key Milestones in Improving Survival Rates
There have been a few big moments that have helped kids with leukemia live longer. These include:
- The creation of combo chemotherapy regimens
- Advances in care, like better infection management and blood transfusions
- The start of targeted and immunotherapies
- Better ways to figure out who needs what treatment
Current Overall Survival Statistics
Today, more kids with leukemia are living longer. About 85% of kids in North America and Europe with leukemia survive at least five years after diagnosis. This is thanks to all the hard work of researchers, doctors, and families.
The progress in treating childhood leukemia gives hope to families dealing with this disease. With ongoing research and medical advancements, we can expect even better survival rates and quality of life for survivors.
Understanding Childhood Leukemia: Types and Differences
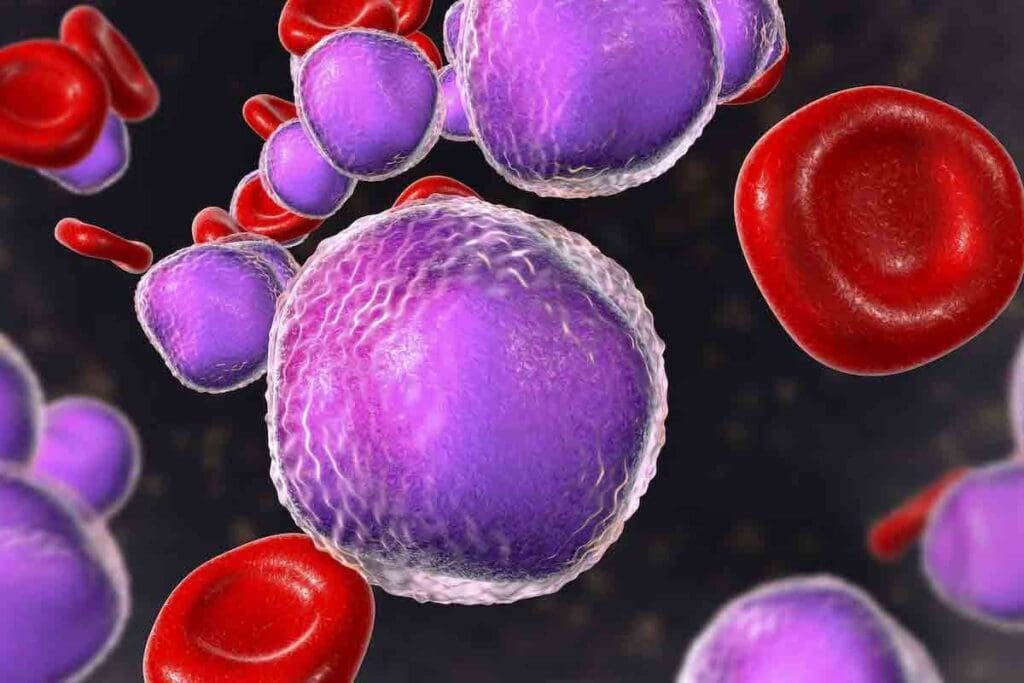
Childhood leukemia is not just one disease. It’s a group of cancers that affect the blood and bone marrow. The two main types are Acute Lymphoblastic Leukemia (ALL) and Acute Myeloid Leukemia (AML). Each has its own characteristics and treatment methods.
Acute Lymphoblastic Leukemia (ALL)
ALL is the most common childhood leukemia, making up 75-80% of cases. It’s caused by the fast growth of immature lymphocytes, a type of white blood cell. Today, the five-year survival rate for ALL is over 90% in many cases. Treatment for ALL includes chemotherapy and sometimes maintenance therapy to prevent relapse.
A leading leukemia researcher says, “Risk-stratified therapy for ALL has been a big step forward. It lets us give high-risk patients more treatment while keeping lower-risk patients safe.” This has helped improve survival rates for children with ALL.
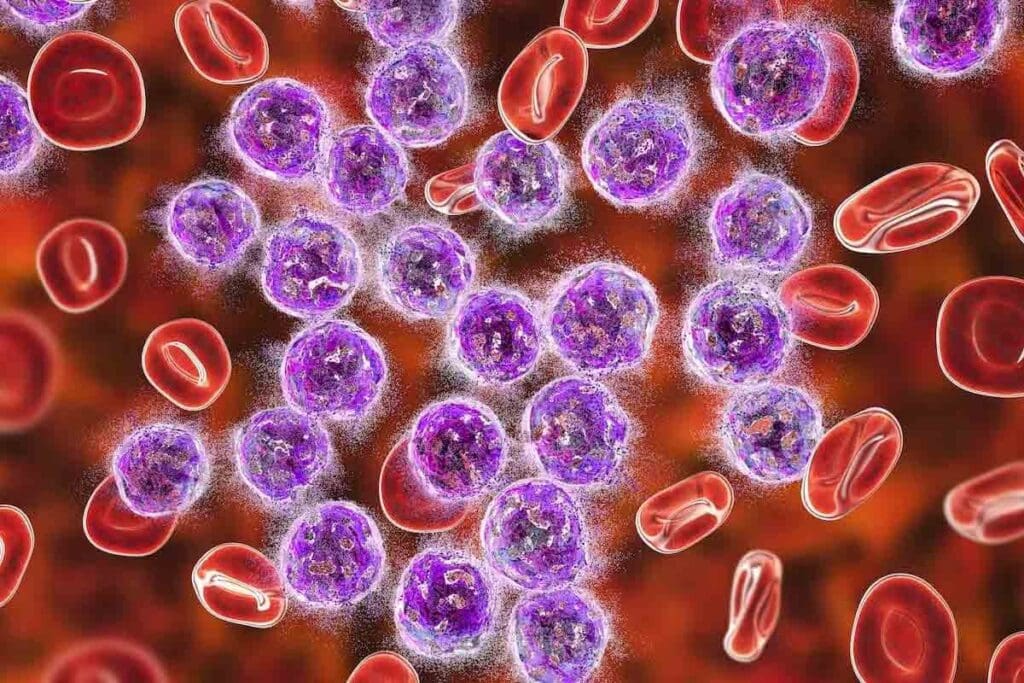
Acute Myeloid Leukemia (AML)
AML is harder to treat and makes up 20-25% of childhood leukemia cases. It’s caused by the fast growth of abnormal myeloid cells in the bone marrow. The prognosis for AML depends on the child’s age, genetic abnormalities, and how well they respond to treatment. Treatment for AML includes intensive chemotherapy and sometimes a stem cell transplant.
A study in the Journal of Clinical Oncology found that “new ways to understand AML have led to finding new treatments and better ways to predict outcomes.” This has helped make treatments more personalized and effective for children with AML.
Other Less Common Types
There are other, less common types of leukemia, like Chronic Lymphocytic Leukemia (CLL) and Chronic Myeloid Leukemia (CML). These are rare in children. They have different characteristics and treatments from ALL and AML. For example, CLL is more common in adults, and when it happens in children, it needs a different treatment plan.
- Chronic Lymphocytic Leukemia (CLL): Rare in children, CLL involves the gradual accumulation of mature lymphocytes.
- Chronic Myeloid Leukemia (CML): CML is characterized by the uncontrolled growth of myeloid cells and is more common in adults.
- Juvenile Myelomonocytic Leukemia (JMML): A rare type of leukemia that occurs in young children, often associated with genetic mutations.
Knowing about these different types of leukemia is key to creating effective treatment plans. As research keeps improving, the outlook for children with leukemia is getting better.
Acute Lymphoblastic Leukemia (ALL): The Most Common and Most Treatable
Childhood Acute Lymphoblastic Leukemia (ALL) is now one of the most treatable cancers. This is thanks to new medical research and better treatment plans. ALL is a cancer that affects the blood and bone marrow, causing too many immature white blood cells.
Thanks to years of research and clinical trials, we now have better ways to treat ALL. This has greatly improved the chances of survival for children with this disease.
Current Five-Year Survival Rates for ALL
The five-year survival rate for children with ALL is about 90 percent. This shows how far we’ve come in treating this cancer. The survival rate means the percentage of kids who live at least five years after being diagnosed.
B-Cell vs. T-Cell ALL Survival Differences
ALL is divided into B-cell and T-cell types, each with different survival chances. B-cell ALL makes up about 85% of cases and has a high cure rate, with survival rates over 90% in many studies. T-cell ALL, once seen as having a poorer prognosis, has also seen survival rates improve with modern treatments.
Knowing whether a child has B-cell or T-cell ALL is important. It helps doctors decide on the best treatment. Children with B-cell ALL usually get less intense chemotherapy than those with T-cell ALL, who need more aggressive treatment.
Treatment Protocols That Have Improved Outcomes
Several treatment plans have helped improve survival rates in childhood ALL. These include:
- Risk stratification: Treatment is tailored based on the risk of relapse.
- Intensification of chemotherapy: Higher doses of chemotherapy for high-risk patients.
- Targeted therapy: Use of drugs that target specific cancer cells.
- Supportive care: Advances in managing side effects and complications.
The following table summarizes the key factors influencing survival rates in childhood ALL:
| Factor | Impact on Survival |
| B-cell ALL | Higher survival rates (>90%) |
| T-cell ALL | Lower survival rates compared to B-cell ALL, but improving |
| Risk Stratification | Tailors treatment to risk, improving outcomes |
| Modern Chemotherapy | More effective and targeted, reducing toxicity |
Thanks to these advancements, ALL is now one of the most curable childhood cancers. Ongoing research and better treatment plans will likely continue to improve survival rates and quality of life for children with ALL.
Acute Myeloid Leukemia (AML): Challenging But Improving Outcomes
Children with AML now have better chances of survival thanks to new treatments. AML is a blood and bone marrow cancer. It grows fast and blocks normal blood cell production.
Current Five-Year Survival Rates for AML
There’s been a big leap in treating childhood AML. Now, over 65 percent of kids survive five years after diagnosis. This gain is thanks to better chemotherapy and care.
Studies show that survival rates for AML in kids have gone up over the years.
| Year | Five-Year Survival Rate |
| 1990s | 40% |
| 2000s | 55% |
| 2020s | 65% |
Recent Advances in AML Treatment
New treatments for AML have been introduced. These include stronger chemotherapy and stem cell transplants. For more info on childhood AML, check out this resource.
Targeted therapies and better care have also helped. These steps have made AML treatment more effective.
Factors That Influence AML Prognosis
Several things affect how well a child with AML will do. These include genetic traits, how well they respond to treatment, and MRD levels. Kids with certain genes may face different challenges.
- Genetic abnormalities
- Response to initial treatment
- Presence of MRD
Childhood Leukemia Survival Rates by Age Group
Childhood leukemia survival rates change with age. Infants, young children, and teens face different challenges. Knowing these differences helps parents and doctors make better treatment choices.
Infants (Under 1 Year)
Infants with leukemia have a tough time. Infant leukemia survival rates are lower than for older kids. This is because the disease is very aggressive in babies, and treating them is hard.
Studies show that babies under 1 with ALL have a lower survival rate. This is often because of certain genetic problems, like the MLL gene rearrangement, which is more common in infant leukemia.
Young Children (Ages 1-9)
Children aged 1 to 9 have seen big improvements in leukemia survival. This age group usually has a better chance of beating the disease, thanks to ALL.
The childhood leukemia survival rates by age show that kids in this age group do better. They can handle chemotherapy better and are less likely to have high-risk genetic features.
Adolescents (Ages 10-19)
Adolescents with leukemia face unique challenges. While treatments have gotten better, they are at higher risk for side effects and may not respond as well to therapy.
Research shows that teens with ALL have a slightly lower survival rate than younger kids. But their overall chances of survival are good. The leukemia in babies survival rate is different from that of teens, showing the need for age-specific treatments.
Understanding the differences in childhood leukemia survival rates by age helps doctors and families make better choices. This way, they can navigate the complexities of leukemia treatment more effectively.
Genetic and Biological Factors Affecting Childhood Leukemia Survival
Genetic and biological factors are key to how well kids with leukemia do. These factors can change how a child reacts to treatment and their chances of getting better.
Chromosomal Abnormalities and Their Impact
Chromosomal abnormalities are a big deal in childhood leukemia. Some, like extra chromosome 21 or certain translocations, can make leukemia cells act differently. For example, kids with Down syndrome might do better in treatment because their cells are more sensitive to drugs.
Translocations, like the ETV6-RUNX1 fusion, are common in B-cell ALL and usually mean a good outlook. But some, like the MLL gene rearrangement, are linked to a worse prognosis.
Minimal Residual Disease (MRD) Status
Minimal Residual Disease (MRD) is when leukemia cells stay in the body after treatment. MRD status is a strong sign of how likely a child is to relapse and survive. Kids with low or undetectable MRD usually have a better chance, while those with high MRD levels face a higher risk.
By checking MRD with flow cytometry or PCR, doctors can see how well treatment is working. This helps tailor treatment to each child, leading to better results.
Other Biological Markers
Other biological markers also play a role in survival rates for kids with leukemia. These include genetic mutations, like those in the TP53 or IKZF1 genes, and certain proteins in leukemia cells.
For instance, some surface antigens help doctors classify leukemia types and decide on treatments. Knowing these markers is key to creating targeted therapies and better patient care.
Special Considerations for Infant Leukemia
Infants with leukemia face unique challenges that need special treatments. Leukemia in babies, like Acute Lymphoblastic Leukemia (ALL) and Acute Myeloid Leukemia (AML), is different from leukemia in older kids.
Why Infant Leukemia Has Lower Survival Rates
Infant leukemia often has lower survival rates than in older kids. This is due to several reasons, including mixed lineage leukemia (MLL) gene rearrangements. These are more common in infants and often mean a worse prognosis.
Infants’ young immune systems and fast disease progression make treatment harder. Their developing organs are also more at risk from chemotherapy’s side effects. This makes it tough to treat without harming them long-term.
Specialized Treatment Protocols for Infants
Researchers and doctors are working on special treatments for infant leukemia. These aim to boost survival rates while reducing harm from treatment.
Treatment for infant leukemia might include chemotherapy, targeted therapy, and sometimes stem cell transplants. The treatment plan is made just for the infant, based on their risk level. This is decided by things like MLL gene rearrangements and how well they respond to treatment.
| Treatment Component | Description | Benefit |
| Chemotherapy | Intensive multi-agent chemotherapy regimens | Effective in achieving remission |
| Targeted Therapy | Drugs targeting specific molecular abnormalities | Reduces toxicity and improves efficacy |
| Stem Cell Transplantation | Replaces the infant’s bone marrow with healthy cells | Offers a potentially curative option for high-risk cases |
Recent Improvements in Infant Leukemia Outcomes
In recent years, there have been big steps forward in treating infant leukemia. New, less harmful treatments have helped increase survival rates.
Studies are ongoing to make treatments even better. They focus on tailoring therapy for each infant’s risk level. New drugs and targeted therapies are being tested to improve outcomes for babies with leukemia.
Long-Term Survival and Quality of Life After Childhood Leukemia
Medical treatments for childhood leukemia have gotten better. Now, we focus on long-term survival and quality of life. Survivors face many challenges after treatment, making ongoing care key.
Late Effects of Treatment
Childhood leukemia survivors may face late effects of treatment. These can include organ damage, growth issues, and a higher risk of secondary cancers. For example, some chemotherapy and radiation can harm the heart later in life. Regular follow-up care is essential to monitor and manage these effects.
Follow-Up Care and Monitoring
Follow-up care for survivors includes regular check-ups and monitoring for late effects. A detailed care plan helps survivors deal with long-term challenges. This may include screenings for secondary cancers, heart checks, and overall health assessments.
Psychosocial Outcomes for Survivors
The psychosocial outcomes for childhood leukemia survivors vary. While many lead healthy, fulfilling lives, others face anxiety, depression, or social and emotional challenges. Access to psychosocial support services, like counseling and support groups, is vital for coping.
What Parents Should Know About Relapse and Second-Line Treatments
Childhood leukemia relapse is a complex issue that parents need to understand. It happens when leukemia comes back after treatment ends. Knowing the risks, signs, and treatment options is key for parents.
Relapse Rates and Survival After Relapse
Relapse rates depend on the leukemia type and initial treatment response. For example, kids with Acute Lymphoblastic Leukemia (ALL) face different outcomes based on when and where the relapse happens.
- Early Relapse: Relapse within a year of diagnosis usually has a poorer prognosis.
- Late Relapse: Relapse after a longer time may have better outcomes.
Thanks to new treatments, survival after relapse has improved. This includes new chemotherapy and targeted therapies.
New and Emerging Therapies for Relapsed Leukemia
The treatment for relapsed leukemia is changing. New and emerging therapies are showing promise.
- Targeted Therapies: Drugs that target specific genetic mutations or proteins in leukemia cells.
- Immunotherapies: Treatments that use the immune system to fight leukemia, like CAR-T cell therapy.
- Clinical Trials: Ongoing studies looking into new drugs and treatment combinations.
These therapies offer hope for better outcomes in children with relapsed leukemia.
Stem Cell Transplantation Outcomes
Stem cell transplantation is a treatment for some children with relapsed leukemia. It replaces the diseased bone marrow with healthy stem cells.
“Stem cell transplantation can be a curative option for patients with high-risk or relapsed leukemia, giving them a chance for long-term survival.”
-Hematology experts highlight.
Outcomes after stem cell transplantation have gotten better. This is thanks to better donor matching, reduced-intensity conditioning regimens, and advances in post-transplant care.
Conclusion: Hope and Perspective for Parents Facing Childhood Leukemia
Getting a diagnosis of childhood leukemia is tough for families. But thanks to new treatments, many kids are now surviving. This gives hope to parents of kids with leukemia.
The path to recovery is long and hard. But knowing about leukemia types, treatments, and survival chances helps parents. Thanks to ongoing research, the outlook for families with leukemia is getting better.
As treatments get better, it’s key for parents to stay updated. Working with doctors helps ensure their child gets the best care. This way, families can face leukemia’s challenges with hope and confidence for a brighter future.
FAQ
What is the overall survival rate for childhood leukemia?
The five-year survival rate for childhood leukemia is over 85 percent. This shows a big improvement in treatment.
How do survival rates differ between acute lymphoblastic leukemia (ALL) and acute myeloid leukemia (AML)?
ALL has a better five-year survival rate than AML. This is because of new treatments for ALL.
What are the survival rates for B-cell and T-cell ALL?
B-cell ALL usually has a higher survival rate than T-cell ALL. But, both have seen better outcomes thanks to new treatments.
How does age affect childhood leukemia survival rates?
Infants under one year have lower survival rates. Young children aged 1-9 have the highest rates. Adolescents face challenges that can affect their survival.
What genetic and biological factors influence childhood leukemia survival?
Chromosomal abnormalities and minimal residual disease (MRD) status are key. They help predict prognosis and guide treatment.
Why does infant leukemia have a lower survival rate?
Infant leukemia often has high-risk genetic features. It needs special treatments, leading to lower survival rates.
What are the late effects of childhood leukemia treatment?
Survivors might face organ damage, secondary cancers, and psychosocial challenges. This shows the need for ongoing care.
What are the chances of survival after a leukemia relapse?
Survival after relapse depends on leukemia type, timing, and treatment response. New therapies are helping.
How effective is stem cell transplantation in treating childhood leukemia?
Stem cell transplantation is effective for some relapsed or high-risk leukemia cases. It offers a chance of a cure for some patients.
Is childhood leukemia curable?
Yes, many children with leukemia are cured. Advances in treatment are improving cure rates.
What is the cure rate for childhood acute lymphoblastic leukemia (ALL)?
The cure rate for childhood ALL is about 90 percent or higher for some subtypes. It’s one of the most treatable cancers in kids.
What is the prognosis for childhood acute myeloid leukemia (AML)?
AML’s prognosis depends on genetic characteristics and treatment response. But, survival rates are improving with new therapies.
How do childhood leukemia survival rates compare across different studies?
Survival rates might vary slightly between studies. This is due to different populations, treatments, and follow-up periods. But, overall, outcomes are getting better.
References
- Buechner, J., Zwaan, C. M., Pabst, T., & Creutzig, U. (2023). Pediatric Acute Myeloid Leukemia — Past, Present, and Future. Frontiers in Pediatrics, 11, Article 8837075. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8837075/
- National Cancer Institute. (2025, January). Childhood Acute Myeloid Leukemia Treatment (PDQ®). https://www.cancer.gov/types/leukemia/hp/child-aml-treatment-pdq