We know that childhood obesity is a big problem in the U.S. It affects almost 1 in 5 kids and teens. Get a simple ‘childhood obesity definition.’ Our best guide explains the BMI criteria, causes, and shocking 2024 statistics in the US.
It’s when a child’s body mass index (BMI) is at or above the 95th percentile for their age and sex. This is a serious issue that can affect their health for years to come.
By 2024, the number of kids and teens with obesity in the U.S. is very high. This shows we need to keep working hard to solve this problem.
Key Takeaways
- Childhood obesity is defined as having a BMI at or above the 95th percentile for age and sex.
- Approximately 1 in 5 U.S. children and adolescents have obesity.
- The prevalence of childhood obesity has increased significantly.
- Childhood obesity is a critical public health concern with long-term implications.
- Understanding the current statistics is essential for addressing this issue.
The State of Childhood Obesity in America

Approximately 14.7 million children in the U.S. are affected by obesity as of 2024. This is a huge public health challenge. The World Health Organization says over 390 million kids and teens aged 5–19 were overweight in 2022. This includes 160 million with obesity.
The Scale of the Public Health Challenge
Childhood obesity in the United States is a big worry. It affects kids’ health and wellbeing. It also puts a big strain on the healthcare system and society.
Some key statistics show how big the problem is:
- About 1 in 5 children in the U.S. has obesity.
- Obesity hits some racial and ethnic groups harder.
- It leads to many health problems now and later in life.
Key Trends in 2024
Looking at childhood obesity trends in 2024, we see a few important points:
- Increased Prevalence: Obesity in kids is getting worse. Some age groups are more affected than others.
- Age-Specific Trends: Obesity rates change with age. Teens (ages 12-19) have a high rate.
- Racial and Ethnic Disparities: Obesity rates vary by race and ethnicity. This shows we need to focus on specific groups.
Knowing these trends helps us find ways to fight childhood obesity. We can work to make American kids healthier.
Childhood Obesity Definition: Medical and Clinical Criteria
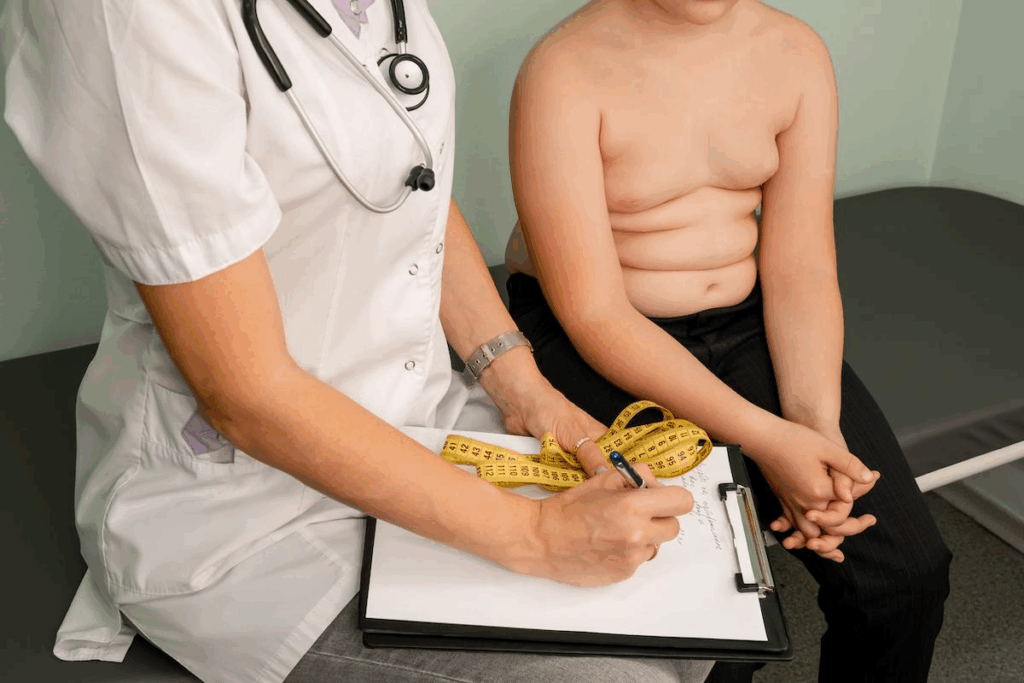
The medical world has its own way of defining childhood obesity. It’s different from how they define it in adults. The Centers for Disease Control and Prevention (CDC) says a child is obese if their Body Mass Index (BMI) is at or above the 95th percentile. This percentile is based on the child’s age and sex.
BMI Percentiles and Classification System
The CDC uses a special BMI percentile system for kids. It compares a child’s BMI to a growth chart. This chart shows how BMI is spread out among kids of the same age and sex.
- Underweight: BMI less than the 5th percentile
- Normal weight: BMI between the 5th and 84th percentiles
- Overweight: BMI between the 85th and 94th percentiles
- Obese: BMI at or above the 95th percentile
Differences Between Adult and Childhood Obesity Definitions
Adult obesity is defined by a specific BMI (BMI ≥ 30 kg/m²). But, childhood obesity is different. It’s based on age- and sex-specific BMI percentiles. This is because kids’ bodies change a lot with age and sex.
For example, a BMI percentile chart for kids considers the natural changes in body fat during growth. This gives a more detailed look at obesity in children.
Clinical Assessment Methods and Tools
Doctors use many ways to diagnose and classify obesity in kids. These include:
- Anthropometric measurements (height, weight, BMI)
- Growth charts and BMI percentiles
- Waist circumference measurements
- Medical history and physical examination
- Laboratory tests (e.g., lipid profiles, glucose levels)
By using these methods, doctors can accurately find out if a child is obese. Then, they can make a good treatment plan.
2024 Childhood Obesity Statistics in the United States
Recent data on childhood obesity rates in the United States shows a big challenge for our health. About 19.7% of kids aged 2-19 have obesity. This is a big problem that needs many solutions.
Current National Prevalence Data
The CDC’s latest numbers show that obesity in kids and teens is a big issue. It’s even bigger in some racial and ethnic groups. The CDC’s National Health and Nutrition Examination Survey (NHANES) shows how big this problem is.
The obesity prevalence changes a lot depending on who you are. This shows we need to focus on different groups. Keeping track of these numbers is key to understanding the problem.
Changes from Previous Years (2020-2023)
Looking at childhood obesity statistics from 2020 to 2023, we see some ups and downs. The CDC’s data shows how different efforts and challenges affect our health.
- From 2020 to 2023, some age groups saw a small drop in obesity rates. This might be because of more awareness and prevention.
- But, the overall trend is worrying, with some groups facing higher rates.
CDC Surveillance and Reporting Methods
The CDC uses strong methods to watch childhood obesity rates. The NHANES data is a big part of this, giving us a clear picture of the U.S. population’s health.
The CDC’s methods include:
- Doing regular surveys and exams to get data on obesity.
- Looking at the data to find trends and patterns in different groups.
- Sharing the findings to help shape public health policies and strategies.
Understanding the CDC’s role in monitoring childhood obesity helps us see how complex this issue is. It shows why we need to rely on data to tackle it.
Age-Specific Obesity Rates Among American Youth
As kids get older, their chances of being overweight change. We look at how obesity rates vary by age among American youth. This includes preschool, school-age, and teenagers.
Preschool Children (Ages 2-5): 12.7% Prevalence
Preschoolers aged 2-5 have a 12.7% obesity rate. This age is key because early obesity can lead to health problems later. Early intervention is vital to avoid long-term health issues.
School-Age Children (Ages 6-11): 20.7% Prevalence
School-age kids, 6 to 11, have a 20.7% obesity rate. This shows why school-based health initiatives and parental support are so important for a healthy lifestyle.
Adolescents (Ages 12-19): 22.2% Prevalence
Adolescents, 12 to 19, have a 22.2% obesity rate. This age group faces challenges like peer influence and increased independence in food choices. Targeted efforts are needed to help them.
The CDC says obesity rates differ by age among kids. This shows the need for strategies that fit each age group to fight childhood obesity.
Obesity rates go up as kids get older. This highlights the need for early and ongoing efforts to help them. By understanding these trends, we can create better prevention and treatment plans for each age group.
Teenage Obesity in America: A Closer Look
Teenage obesity is a complex issue with many factors involved. It affects not just personal health but also the healthcare system and society. Understanding this is key to tackling the problem.
Current Teenage Obesity Rate Statistics
About 22.2% of teens aged 12-19 have obesity, recent stats show. This highlights the need for effective solutions.
Obesity rates vary among different groups. Some groups face higher risks. Knowing these differences helps in creating better prevention and treatment plans.
Key Statistics:
- 22.2% of adolescents aged 12-19 have obesity
- Obesity rates are higher among certain ethnic and socioeconomic groups
- The prevalence of severe obesity is also on the rise among teenagers
Unique Factors Affecting Adolescent Weight
Adolescence is a time of growth and change. Many factors can impact weight during this period. These include:
- Dietary habits and nutritional knowledge
- Physical activity levels and sedentary behaviors
- Socioeconomic status and access to healthy food options
- Psychological factors, such as stress and body image concerns
The World Health Organization (WHO) notes that childhood and adolescent obesity can harm health. It increases the risk of noncommunicable diseases later in life.
“The risk factors for noncommunicable diseases start early in life, and the risk of developing these diseases is significantly increased by being overweight or obese during adolescence.”
World Health Organization
Long-term Implications for Young Adults
Teenage obesity has long-term health effects. Young adults who were obese as teens face higher risks of chronic diseases. These include:
- Diabetes
- Cardiovascular disease
- Certain types of cancer
Early action and prevention are vital. They help reduce these risks and improve health outcomes for young adults.
We need a broad approach to tackle teenage obesity. This includes education, policy changes, and community efforts. Together, we can lower obesity rates and enhance health and wellbeing among teens.
Racial and Ethnic Disparities in US Childhood Obesity
Childhood obesity rates vary a lot in the United States. Different racial and ethnic groups face different challenges. This shows how complex the issue is.
Non-Hispanic Black Children: 23.5% Obesity Rate
Non-Hispanic Black children have a high obesity rate of 23.5%. This is much higher than some other groups. It shows we need special help for them.
Hispanic Children: 22.2% Obesity Rate
Hispanic children also have a high obesity rate of 22.2%. Their diet, exercise, and money situation might play a part.
Social Determinants Behind Racial Disparities
Many things cause these racial differences. Socioeconomic status, access to healthy food, and safe places to be active are key. For example, not having stores with fresh food can lead to more obesity.
We need a big plan to fix these problems. This includes changing laws, starting community programs, and teaching people. Knowing why these differences exist helps us find ways to help all kids, no matter their race or ethnicity.
Socioeconomic Factors and Childhood Obesity Rates
Lower-income families face a higher risk of childhood obesity. This is due to several socioeconomic factors. We will look into how income, food access, and housing conditions affect obesity rates in children from lower-income backgrounds.
Income-Related Patterns: 24.1% in Lowest vs. 10.4% in Highest Income Groups
Research shows that kids from poorer families are more likely to be obese. The gap in obesity rates between the poorest and richest families is huge. While 24.1% of low-income kids are obese, only 10.4% of those from wealthier families are.
Here’s a table showing this difference:
Income Group | Childhood Obesity Rate (%) |
Lowest Income | 24.1 |
Middle Income | 18.5 |
Highest Income | 10.4 |
Food Environment and Nutrition Access
The food environment is key in the fight against childhood obesity. Lower-income families often struggle to find healthy food. They tend to eat more high-calorie, high-fat foods because they’re cheaper but not good for health.
Food deserts and the lack of supermarkets in poor areas make things worse. It’s vital to increase access to healthy food to fight childhood obesity.
Housing and Neighborhood Influences
Housing and neighborhood conditions also play a big role in childhood obesity. Low-income areas often lack safe places for kids to play. This limits their chances to be active.
Living in tough neighborhoods can also stress kids out. This stress can harm their health and increase obesity rates.
By understanding these factors, we can create better plans to lower childhood obesity rates. This is important for lower-income families.
Economic Impact of Childhood Obesity in the US
The US is facing a big economic challenge because of childhood obesity. This issue affects not just health, but also the economy and healthcare system.
Annual Healthcare Costs
The annual healthcare costs for childhood obesity are huge, at $1.3 billion. This shows we need to find ways to prevent and treat it.
Children with obesity spend a lot more on healthcare than others. This is because they often need more hospital visits and treatments.
Individual Cost Burden
For each child, the cost of obesity is much higher. Studies say it’s $116 to $310 more each year than for non-obese kids.
This shows how important it is to start treating obesity early. It helps families and the healthcare system save money in the long run.
Projected Lifetime Economic Consequences
The future costs of childhood obesity are scary. Kids who are obese as adults will likely face more health problems and costs.
We need to think about these long-term costs when we plan to fight childhood obesity. By investing in prevention and treatment, we can save money for both individuals and society.
In summary, childhood obesity in the US has big economic costs. It affects healthcare and families. We need a strong plan to prevent and treat it to save money and improve health.
Geographic Variations in Childhood Obesity Across America
Childhood obesity in America varies by region. Some states and areas face bigger challenges than others. This is shown in recent data.
States with Highest Childhood Obesity Prevalence
Some U.S. states have much higher childhood obesity rates. Mississippi leads with over 25% of kids affected. Other high rates are seen in Alabama, Arkansas, and Louisiana.
These states often have lower incomes, less access to healthy food, and fewer chances for kids to be active.
States with Lowest Childhood Obesity Prevalence
States like Colorado, Utah, and Minnesota have lower rates. They have higher incomes, better food access, and more chances for kids to be active.
Colorado, for example, has a big outdoor culture. This helps keep obesity rates low.
Urban vs. Rural Obesity Patterns
Urban and rural areas show different obesity patterns. Rural areas often have higher rates. This is due to less access to healthy food, fewer places to play, and longer distances to school.
In contrast, urban areas have more chances for a healthy life. They have parks and centers for fun. But, they also face high living costs and food deserts.
It’s key to understand these differences to fight childhood obesity. By knowing the challenges of each area, we can make better plans to help kids stay healthy across America.
Health Consequences of Childhood Obesity
Childhood obesity affects many areas of a child’s life. It impacts their physical, mental, and social health. The effects can last a long time.
Immediate Physical Health Complications
Childhood obesity leads to several serious health problems. One major issue is type 2 diabetes, which is becoming more common in kids. Other problems include:
- Respiratory problems: Kids with obesity are more likely to have asthma and sleep apnea.
- Joint problems: Excess weight can cause issues like Blount’s disease, affecting the legs and hips.
- Cardiovascular risk factors: High blood pressure, high cholesterol, and other factors increase the risk of heart disease.
Psychological and Social Impacts
Childhood obesity also has serious mental and social effects. Kids with obesity often face:
- Low self-esteem: Weight-related bullying and social stigma can hurt a child’s self-image.
- Depression and anxiety: The emotional toll of obesity can lead to mental health issues.
- Social isolation: Children may feel embarrassed or ashamed and withdraw from social activities.
Long-term Health Risks into Adulthood
Childhood obesity can lead to serious health problems that last into adulthood. These include:
Health Risk | Description | Potential Long-term Impact |
Cardiovascular disease | Increased risk due to high blood pressure and cholesterol | Heart attacks, strokes, and other cardiovascular events |
Type 2 diabetes | Continued risk into adulthood if obesity persists | Diabetes-related complications, including kidney damage and vision loss |
Cancer | Some cancers are associated with obesity | Increased risk of various types of cancer |
It’s important to understand these health consequences to fight childhood obesity. By tackling this issue, we can protect children’s health now and in the future.
Conclusion: Addressing the Childhood Obesity Epidemic
To tackle the childhood obesity crisis, we need a wide-ranging plan. This includes pushing for healthy eating, more exercise, and policies that back up these efforts. The World Health Organization (WHO) and Centers for Disease Control and Prevention (CDC) suggest a mix of actions to fight and manage childhood obesity.
Childhood obesity isn’t just a personal issue; it affects society too. It brings big costs and health problems down the line. So, stopping childhood obesity is key, and we must use all the right strategies to do it.
Healthcare experts, lawmakers, and local groups can join forces to fight childhood obesity. Together, they can make places that encourage healthy living. This teamwork is critical in making our communities better for everyone’s health.
FAQ
What is childhood obesity, and how is it defined?
Childhood obesity is when a child’s BMI is at or above the 95th percentile for their age and sex. We use the BMI percentile system to check if a child’s weight is healthy.
What are the current statistics on childhood obesity in the US?
In the US, about 19.7% of kids aged 2-19 have obesity. This rate varies by age. For example, 12.7% of preschoolers, 20.7% of school-age kids, and 22.2% of teens have obesity.
How does childhood obesity differ from adult obesity?
Children’s bodies are growing and changing, so we define obesity differently for them. We consider their age and sex. The health problems caused by obesity can also differ between kids and adults.
What are the health consequences of childhood obesity?
Obesity in kids can cause health problems like insulin resistance and type 2 diabetes. It can also affect their mental health, leading to low self-esteem and feeling left out. Kids with obesity are at higher risk for heart disease and some cancers later in life.
What socioeconomic factors contribute to childhood obesity?
Kids from lower-income families are more likely to be obese. The rate is 24.1% in the lowest income group and 10.4% in the highest. Food environment, nutrition access, and housing conditions also play a role.
Are there racial and ethnic disparities in childhood obesity rates?
Yes, there are big differences in obesity rates among racial and ethnic groups. Non-Hispanic Black kids have a rate of 23.5%, and Hispanic kids have a rate of 22.2%. These disparities are linked to socioeconomic status and access to healthy food and activities.
What is the economic impact of childhood obesity in the US?
Childhood obesity costs the US healthcare system about $1.3 billion a year. Each child with obesity costs $116-310 more annually. The long-term economic effects of obesity are huge, showing the need for early action.
How does childhood obesity vary across different regions in the US?
Obesity rates vary across the US, with some states having higher rates than others. Urban and rural areas also have different patterns. This shows the need for specific solutions in each area.
What can be done to address the childhood obesity epidemic?
To fight childhood obesity, we need a team effort from healthcare, policymakers, and communities. We should focus on prevention and management. This includes promoting healthy eating and activity, improving access to healthy food and safe places to be active, and supporting families and kids with obesity.
References
Government Health Resource. Evidence-Based Medical Guidance. Retrieved from https://www.nutritioned.org/certified-nutrition-specialist/