
Hemophilia is an inherited bleeding disorder that makes it difficult for the body to form blood clots. This happens because there are not enough clotting factors in the blood.
We also examine the chromosomes of hemophilia to understand its inheritance. Hemophilia is linked to the X chromosome, which is why males—having only one X chromosome—are at higher risk. Without a second X chromosome to balance a defective gene, males are more likely to be affected. This explains why hemophilia predominantly occurs in men.
Key Takeaways
- Hemophilia is an inherited bleeding disorder that impairs blood clot formation.
- The genetic basis of hemophilia is tied to the X chromosome.
- Males are more likely to have hemophilia due to having only one X chromosome.
- A defective gene on the X chromosome causes hemophilia.
- Females can be carriers of hemophilia, but they are less likely to be affected.
The Basics of Hemophilia: A Blood Clotting Disorder
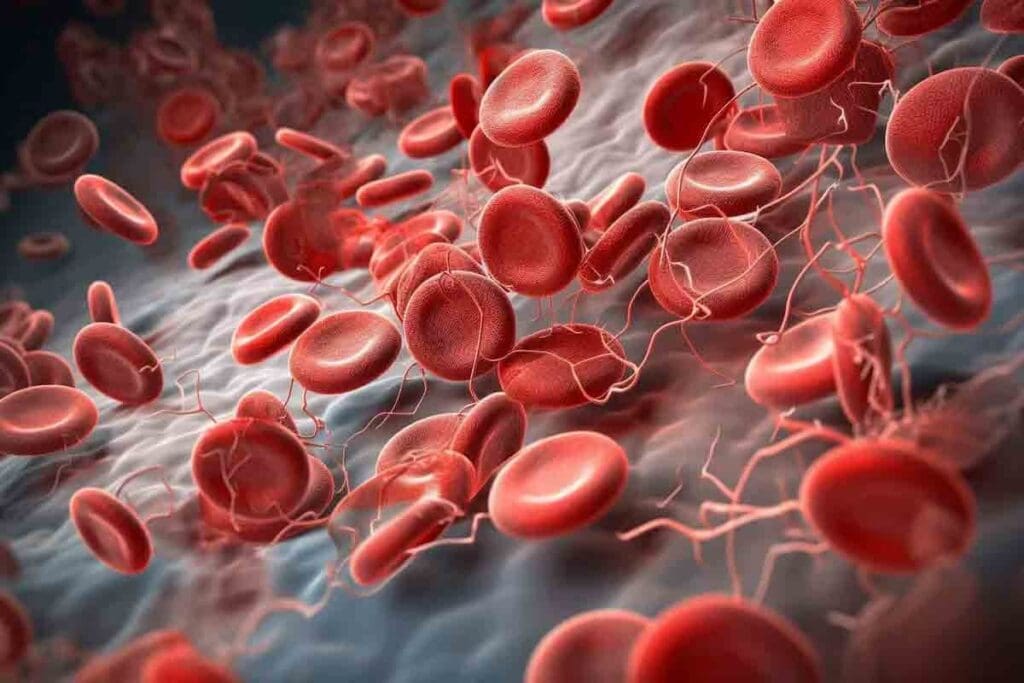
Hemophilia makes it hard for the body to form blood clots. This has big historical and clinical impacts. We’ll look at what it is, how it shows up, and its history. This will help us see why modern treatments are so important.
Definition and Clinical Manifestations
Hemophilia is a genetic disorder that stops the body from making blood clots. These clots are key to stopping bleeding. People with hemophilia often have prolonged bleeding episodes, which can start on their own or after an injury.
The main cause is a lack of clotting factors VIII (8) for Hemophilia A or IX (9) for Hemophilia B. These factors are vital for blood to clot. The genes for these factors are on the X chromosome. This makes hemophilia an X-linked recessive disorder.
| Clotting Factor | Hemophilia Type | Deficiency |
| Factor VIII | Hemophilia A | Low or absent level |
| Factor IX | Hemophilia B | Low or absent level |
Historical Background of Hemophilia
Hemophilia has been around for centuries, with records from the 2nd century. It was called the ‘Royal Disease’ because it was common in European royal families.
“Hemophilia is a bleeding disorder that has been a part of human history for centuries, affecting not just commoners but also royalty.”
In the 20th century, doctors learned more about clotting factors VIII and IX. Knowing its history helps us see how far we’ve come in treating hemophilia.
Types of Hemophilia and Their Prevalence

Hemophilia is not just one condition but a group of bleeding disorders. Each one is caused by a lack of specific clotting factors. The most common types are Hemophilia A and Hemophilia B, with some rare forms also present.
Hemophilia A: Factor VIII Deficiency
Hemophilia A, also known as classic hemophilia, is caused by a lack of factor VIII. It’s the most common type, making up about 80% of cases. Hemophilia A is about three to four times more common than Hemophilia B. It’s caused by mutations in the F8 gene on the X chromosome.
About 1 in every 5,000 male births is affected by hemophilia, with Hemophilia A being the most common.
Hemophilia B: Factor IX Deficiency
Hemophilia B, also known as Christmas disease, is caused by a lack of factor IX. It’s less common than Hemophilia A. It’s caused by mutations in the F9 gene, also on the X chromosome. The symptoms of Hemophilia B are similar to Hemophilia A, making it hard to diagnose just by symptoms.
Rare Forms of Hemophilia
There are other rare types of hemophilia, like Hemophilia C, which is caused by a lack of factor XI. These rare bleeding disorders are less common but important to know about for proper treatment.
It’s key to understand the different types of hemophilia and their genetics. This knowledge helps in making accurate diagnoses and treatment plans. Knowing how these disorders are passed down in families is also important.
The Chromosomes of Hemophilia: Genetic Foundations
Hemophilia’s story starts with the X chromosome, where the F8 and F9 genes live. These genes are key to blood clotting. Knowing how hemophilia is passed down and why it mostly hits males is key.
X Chromosome Structure and Function
The X chromosome is one of two sex chromosomes in humans. Females have two, while males have one X and one Y. It carries many genes, including those for hemophilia A and B.
The X chromosome’s structure includes:
- A large number of genes, including F8 and F9
- Regions critical for gene expression and regulation
- Sequences are vital across species, showing their importance
Location of Hemophilia Genes on the X Chromosome
The genes for hemophilia A (F8) and B (F9) are on the X chromosome’s long arm. F8 is at Xq28, and F9 is at Xq27.1. Knowing where these genes are helps us understand how hemophilia is passed down.
F8 and F9 Genes: Molecular Basis of Hemophilia
The F8 and F9 genes make proteins needed for blood clotting. Mutations in these genes cause hemophilia A and B. Knowing how these genes work is key to finding tests and treatments.
| Gene | Location on X Chromosome | Associated Disorder |
| F8 | Xq28 | Hemophilia A |
| F9 | Xq27.1 | Hemophilia B |
In conclusion, hemophilia’s roots are in the X chromosome, with the F8 and F9 genes. Knowing the X chromosome and these genes is vital for understanding hemophilia’s inheritance and how it shows up.
X-Linked Inheritance Patterns Explained
To understand hemophilia’s genetic role, we must grasp X-linked inheritance patterns. This pattern involves genes on the X chromosome. Hemophilia is a prime example of an X-linked recessive disorder, with the mutated gene on the X chromosome.
How X-Linked Recessive Disorders Are Transmitted
X-linked recessive disorders, like hemophilia, follow a specific pattern. This is because the mutated gene is on the X chromosome. Males, with one X and one Y chromosome, express the disorder if they get an X chromosome with the hemophilia gene.
Carrier Status in Females
Females can carry hemophilia, having one normal X chromosome and one with the mutated gene. They usually don’t show symptoms because the normal X balances out the mutated one. Yet, they can pass the mutated gene to their children.
Punnett Squares and Inheritance Probability
Punnett squares help predict the chance of passing hemophilia. They show the likelihood of a child inheriting the hemophilia gene from their parents. For example, a carrier mother has a 50% chance of each son having hemophilia and each daughter being a carrier.
Consider a scenario where a female carrier has children with a male without hemophilia. Using a Punnett square, we can predict the genotypes and phenotypes of their kids. This shows the risk of hemophilia in sons and carrier status in daughters.
Key Points to Remember:
- Males are more likely to be affected by hemophilia due to having only one X chromosome.
- Females can be carriers of hemophilia, and their carrier status can be passed to their offspring.
- Punnett squares are useful for predicting the probability of hemophilia inheritance.
Understanding X-linked inheritance patterns helps us see why hemophilia mainly affects males. It also shows how the disorder is passed down through generations.
Why Males Are More Susceptible to Hemophilia
Hemophilia mainly affects males because of genetics. It’s caused by mutations in genes for blood clotting proteins, like factor VIII and IX. These genes are on the X chromosome.
We’ll look at why more males get hemophilia. We’ll focus on their chromosomes and what they mean.
The XY Chromosome Disadvantage
Males have an XY chromosome pair, while females have XX. The X chromosome has the genes for hemophilia. If a male gets an X chromosome with a mutation, he gets hemophilia because he only has one X chromosome.
Lack of Compensatory X Chromosome in Males
For males, having only one X chromosome means a mutation in the hemophilia gene causes the condition. Females need both X chromosomes to have the mutation and show symptoms of hemophilia. This makes hemophilia much rarer in females.
This genetic weakness in males is why they get hemophilia more often than females.
Statistical Prevalence in Males vs. Females
The numbers show a big difference in hemophilia cases between males and females. Hemophilia A and B are more common in males.
| Condition | Males | Females |
| Hemophilia A | 1 in 5,000 | 1 in 100,000 |
| Hemophilia B | 1 in 20,000 | 1 in 200,000 |
This table shows how much more common hemophilia is in males. It highlights the genetic reasons for this difference.
Common Misconceptions About Hemophilia Genetics
Hemophilia’s genetics are often misunderstood, leading to many misconceptions. We aim to clear up these misunderstandings and shed light on the genetic basis of hemophilia.
Hemophilia as a Single-Gene Disorder, Not a Chromosomal Abnormality
Many think hemophilia is a chromosomal issue. But it’s actually caused by a mutation in the F8 or F9 gene on the X chromosome. This is different from a chromosomal abnormality.
Knowing that hemophilia is a single-gene disorder is key to genetic counseling. It helps predict the chance of passing it down. It’s not caused by extra or missing chromosomes but by a specific mutation affecting blood clotting.
Myths About Hemophilia Inheritance
One myth is that hemophilia can come from either parent. While both parents can pass on the risk, the pattern is more complex. Males are more likely to be affected because they have only one X chromosome. Females can be carriers and pass the mutated gene to their children.
Another myth is that hemophilia skips generations. While it might seem like it, this isn’t always true. Carrier females can pass the condition to future generations, even if their parents didn’t have it.
Understanding Spontaneous Mutations
About one-third of babies with hemophilia have a new mutation. These mutations happen without a family history of the condition. It’s important to understand these spontaneous mutations for genetic counseling.
Spontaneous mutations show how complex hemophilia genetics are. They highlight the need for genetic testing, even without a known family history.
Female Carriers: Symptoms and Inheritance Patterns
Female carriers are key in passing on hemophilia. Knowing if a female is a carrier is important for family planning. Females can carry the hemophilia gene without showing symptoms because they have a normal gene on the other X chromosome.
Carrier Testing and Identification
Carrier testing checks a female’s blood for the hemophilia gene. This is important for planning families and genetic counseling. Genetic testing can find carriers with great accuracy. This helps families make informed choices about pregnancy and the risk of passing hemophilia.
Symptomatic Female Carriers
Most female carriers don’t show symptoms. But some may be due to X chromosome inactivation. This random process can silence one X chromosome, leading to symptoms if the normal gene is silenced.
X-Chromosome Inactivation and Its Effects
X-chromosome inactivation affects whether a female carrier shows symptoms. The balance of inactivated X chromosomes can change how symptoms appear. This balance can make a big difference in how severe symptoms are.
| X-Chromosome Inactivation Pattern | Effect on Carrier Status | Symptoms in Female Carriers |
| Random Inactivation | Variable expression of the hemophilia gene | Mild to moderate symptoms are possible |
| Skewed Inactivation favoring normal X | Reduced expression of the hemophilia gene | Asymptomatic or mild symptoms |
| Skewed Inactivation favoring hemophilia X | Increased expression of the hemophilia gene | Moderate to severe symptoms are possible |
Knowing about X chromosome inactivation is key to managing female carriers. By identifying carriers and understanding their risk, healthcare providers can offer better support and guidance.
Genetic Mutations and Hemophilia Severity
Hemophilia severity comes from different genetic mutations. These mutations affect how well clotting factors work. The severity depends on how much clotting factor is in the blood. This is tied to the mutation in the F8 or F9 gene.
Types of Mutations in F8 and F9 Genes
The F8 and F9 genes make clotting factors VIII and IX. Mutations in these genes cause hemophilia A and B. There are several types of mutations, including:
- Missense mutations, which result in a non-functional protein
- Nonsense mutations, leading to a truncated protein
- Frameshift mutations, causing a shift in the reading frame and often resulting in a non-functional protein
- Splice site mutations, affecting the splicing of the RNA transcript
These mutations can happen on their own or be passed down from parents. Knowing the type of mutation helps predict how severe hemophilia will be.
Correlation Between Mutation Type and Disease Severity
The type of mutation affects how severe hemophilia is. For example, missense mutations might cause a milder form. But nonsense or frameshift mutations often lead to more severe symptoms.
Studies show that how much clotting factor is left in the blood matters. Little to no clotting factor means more severe hemophilia. But some activity can lead to a milder form.
Recent Advances in Mutation Research
New research has greatly improved our understanding of hemophilia. Technologies like next-generation sequencing help find new mutations. This gives us a better grasp of hemophilia’s genetic roots.
This research changes how we diagnose, treat, and counsel about hemophilia. For instance, knowing specific mutations can predict treatment complications. This is key to avoiding major issues with treatment.
Gene therapy is also being explored. It aims to fix the genetic problem at its source. This could mean no more need for constant treatment, as it could restore normal clotting factor production.
Diagnosis and Genetic Testing
Getting a correct diagnosis of hemophilia is very important. It helps in managing the condition well. Tests check clotting factor levels and find genetic mutations. “Early diagnosis is key to managing hemophilia effectively,” as recent medical guidelines say.
Blood Clotting Factor Assays
Blood clotting factor assays are tests done in labs. They measure clotting factor VIII or IX levels in the blood. These tests help figure out how severe hemophilia is.
Clotting factor assays involve:
- Measuring the activity level of factor VIII or IX
- Checking if the blood can clot rproperlyFinding out how severe hemophilia is based on clotting factor levels
Modern Genetic Testing Methods
Genetic testing for hemophilia looks at genes for clotting factors VIII and IX. It finds mutations. This info is key for genetic counseling and planning families.
Modern genetic testing methods include:
- DNA sequencing to find specific mutations in the F8 or F9 genes
- Gene analysis to see the risk of passing hemophilia to kids
As genetic testing gets better, it’s more important for families with hemophilia history to think about these options.
Prenatal Diagnosis Options
Prenatal diagnosis is for families with hemophilia history. It lets them know early if the fetus has hemophilia. This helps in planning for the pregnancy.
“Prenatal diagnosis gives families important info for making choices about pregnancy,” a leading medical journal says.
Prenatal diagnosis options include:
- Chorionic villus sampling (CVS)
- Amniocentesis
These tests give insights into the fetus’s health. They help families get ready for the future.
Family Planning and Genetic Counseling
Couples with a history of hemophilia can greatly benefit from genetic counseling. This helps them make informed family planning decisions. We understand the complexities of managing hemophilia in families and the importance of support.
Options for Couples with a Family History of Hemophilia
Genetic counseling offers couples with a family history of hemophilia several options. They can understand the risk of passing the mutated gene to their children. They can also discuss the implications of being a carrier and explore reproductive choices.
Risk Assessment: We assess the likelihood of passing the mutated gene to offspring. This helps couples understand their chances of having a child with hemophilia.
Reproductive Options: Couples can consider various reproductive options. These include natural conception, adoption, and assisted reproductive technologies.
Preimplantation Genetic Diagnosis
Preimplantation genetic diagnosis (PGD) is an option for couples undergoing in vitro fertilization (IVF). PGD allows for the screening of embryos for the hemophilia mutation. This enables the selection of unaffected embryos for transfer.
This technology has revolutionized family planning for couples at risk of passing on genetic disorders like hemophilia. By choosing unaffected embryos, couples can significantly reduce the risk of having a child with hemophilia.
| Reproductive Option | Description | Benefit for Hemophilia |
| Natural Conception | Conceiving naturally without medical intervention | Risk of transmitting hemophilia to offspring |
| PGD with IVF | Screening embryos for hemophilia mutation during IVF | Significantly reduces the risk of hemophilia in offspring |
| Adoption | Adopting a child instead of conceiving | Eliminates the risk of genetic transmission |
Ethical Considerations in Genetic Counseling
Genetic counseling for hemophilia involves discussing reproductive options and ethical considerations. We navigate complex decisions with couples, ensuring they are fully informed.
Autonomy: Respecting the couple’s autonomy in making reproductive decisions is key. We provide information and support without directing their choices.
Non-directive Counseling: Our counseling approach is non-directive. We focus on providing complete information to help couples make informed decisions.
By considering these aspects, couples can make decisions that are right for them. They are supported by a thorough understanding of their options and the implications of each choice.
Conclusion: Understanding the X-Factor in Hemophilia
Understanding the role of X chromosomes is key to knowing why more males have hemophilia. Hemophilia is an X-linked disorder. This means it’s more common in males because of how it’s inherited.
The chromosomes of hemophilia are important in passing on the disorder. The X-linked inheritance pattern is the main reason for the difference in how males and females are affected.
We’ve looked at how the X chromosome’s structure and function lead to hemophilia in males. Males, with only one X chromosome, are more likely to get the disorder. This is because they don’t have a second X chromosome to help.
This knowledge is vital for diagnosing, treating, and managing hemophilia.
Knowing about hemophilia’s genetic inheritance helps healthcare providers and families. It helps them make better choices about family planning and genetic counseling. This improves care and support for those with hemophilia.
FAQ
Is hemophilia a chromosomal abnormality?
No, hemophilia is not a chromosomal abnormality. It’s caused by mutations in the F8 or F9 genes on the X chromosome.
Why do males get hemophilia more often than females?
Males get hemophilia more often because they have only one X chromosome. If their X chromosome has the mutated gene, they show the disorder. They don’t have a second X chromosome to balance it out.
What is the genetic basis of hemophilia?
Hemophilia is caused by mutations in the F8 gene (Hemophilia A) or the F9 gene (Hemophilia B). Both genes are on the X chromosome.
Can females be carriers of hemophilia?
Yes, females can carry hemophilia. They have two X chromosomes. Even if one X has the mutated gene, the other can compensate. But they can pass the mutated gene to their sons.
How is hemophilia inherited?
Hemophilia is inherited in an X-linked recessive pattern. The mutated gene is on the X chromosome. Males, with only one X chromosome, are more likely to show the disorder.
What is the role of the X chromosome in hemophilia?
The X chromosome carries the genes (F8 and F9) that cause hemophilia when mutated. Males, with only one X chromosome, are more at risk. They don’t have a second X to balance out the mutated gene.
Are there different types of hemophilia?
Yes, there are two main types. Hemophilia A is caused by a deficiency in factor VIII. Hemophilia B is caused by a deficiency in factor IX.
How does X chromosome inactivation affect female carriers?
X-chromosome inactivation is when one of a female’s X chromosomes is turned off. If the X with the normal gene is turned off more, a female carrier might show symptoms of hemophilia.
What is the significance of genetic counseling for families with hemophilia?
Genetic counseling is key for families with hemophilia. It helps understand the risk of passing on the disorder. It also helps with planning, like preimplantation genetic diagnosis.
Can hemophilia be diagnosed prenatally?
Yes, hemophilia can be diagnosed before birth. Tests check for the mutated gene or clotting factor levels in the fetus.
How do genetic mutations affect the severity of hemophilia?
The severity of hemophilia depends on the mutation in the F8 or F9 gene. Some mutations lead to a bigger deficiency of clotting factor. This makes the disorder more severe.
References:
- National Institutes of Health. (2023). Advances in gene therapy for hemophilia: An update. NIH News. https://www.nih.gov/news-events/nih-research-matters/advances-gene-therapy-hemophilia
- World Health Organization. (2020). Hemophilia fact sheet: Understanding genetic inheritance and treatment. WHO Publications. https://www.who.int/news-room/fact-sheets/detail/hemophilia























