Last Updated on October 31, 2025 by
Chronic kidney disease (CKD) is a big health issue. It affects 1 in 7 adults in the United States. Sadly, 90% of those with CKD don’t know they have it until it’s too late.
We will look at the 5 stages of chronic kidney disease. We’ll cover everything from normal function to kidney failure. We’ll talk about GFR levels, symptoms, and how to classify each stage. Knowing these stages is key to catching the disease early and managing it well.
Healthcare experts use five stages to classify CKD. They look at the estimated glomerular filtration rate (eGFR) and markers of kidney damage. This helps them spot the disease getting worse and act fast to help.
Key Takeaways
- CKD affects 1 in 7 ad ults in the United States.
- 90% of individuals with CKD are unaware of their condition until it progresses.
- Classification into five stages helps in early detection and management.
- eGFR and kidney damage markers are key for CKD staging.
- Understanding CKD stages is vital for timely medical interventions.
Understanding Chronic Kidney Disease (CKD)
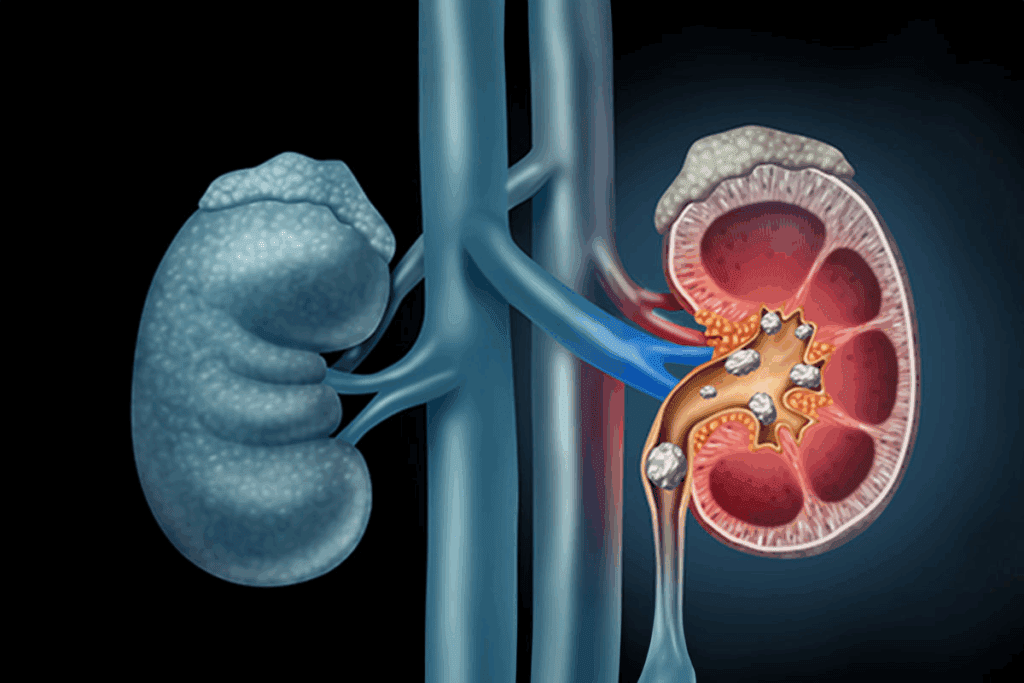
The kidneys are key to our health. CKD happens when they get damaged. It’s when the kidneys can’t filter blood well, causing toxins to build up in the body.
What Causes Kidney Damage
CKD can start from different reasons. Diabetes and high blood pressure are the main causes. They put a lot of strain on the kidneys, slowly damaging them.
Other things can also harm the kidneys, such as:
- Family history of kidney disease
- Obesity and smoking
- Certain genetic conditions
How CKD Progresses Over Time
CKD can progress differently for everyone. But, it usually gets worse over time. As it does, the kidneys work less well, causing more severe symptoms.
Understanding how CKD gets worse is key. It helps manage the disease and slow it down. Regular check-ups and the right treatments can greatly improve life for those with CKD.
The Importance of Glomerular Filtration Rate (GFR)

The glomerular filtration rate (GFR) shows how well the kidneys clean waste from the blood. It’s key for checking kidney health and finding out the stage of chronic kidney disease (CKD).
How GFR Measures Kidney Function
GFR is figured out by the serum creatinine level, age, sex, and race. Serum creatinine is a waste from muscle breakdown.
The GFR test looks at blood creatinine levels to guess how fast the kidneys filter waste. A lower GFR means more advanced CKD. For example, a GFR of 32 is stage 3 CKD, while 44 is also stage 3 but closer to stage 2.
- GFR helps diagnose and track CKD.
- It shows the CKD stage.
- GFR is key for choosing the right treatment.
The Difference Between GFR and eGFR
GFR and eGFR (estimated GFR) are often mixed up, but they’re not the same. GFR is the real filtration rate, and eGFR is an estimate based on serum creatinine, age, sex, and race.
Most labs now give eGFR with creatinine tests. This makes it easier for doctors to check kidney function without hard math. Knowing the difference is important, as eGFR might not always be right for everyone, like the elderly or those with muscle diseases.
- eGFR is calculated with serum creatinine and demographic factors.
- It’s a simple way to check kidney function.
- eGFR values help in staging CKD and planning treatment.
Understanding GFR and eGFR helps doctors manage CKD better. This slows down the disease and lowers the risk of problems. Regular GFR checks are vital for CKD patients to catch issues early.
CKD Staging: The Complete Classification System
Knowing the stages of chronic kidney disease (CKD) is key for good care. CKD staging shows how much kidney damage and function there is. This helps doctors create a treatment plan just for you.
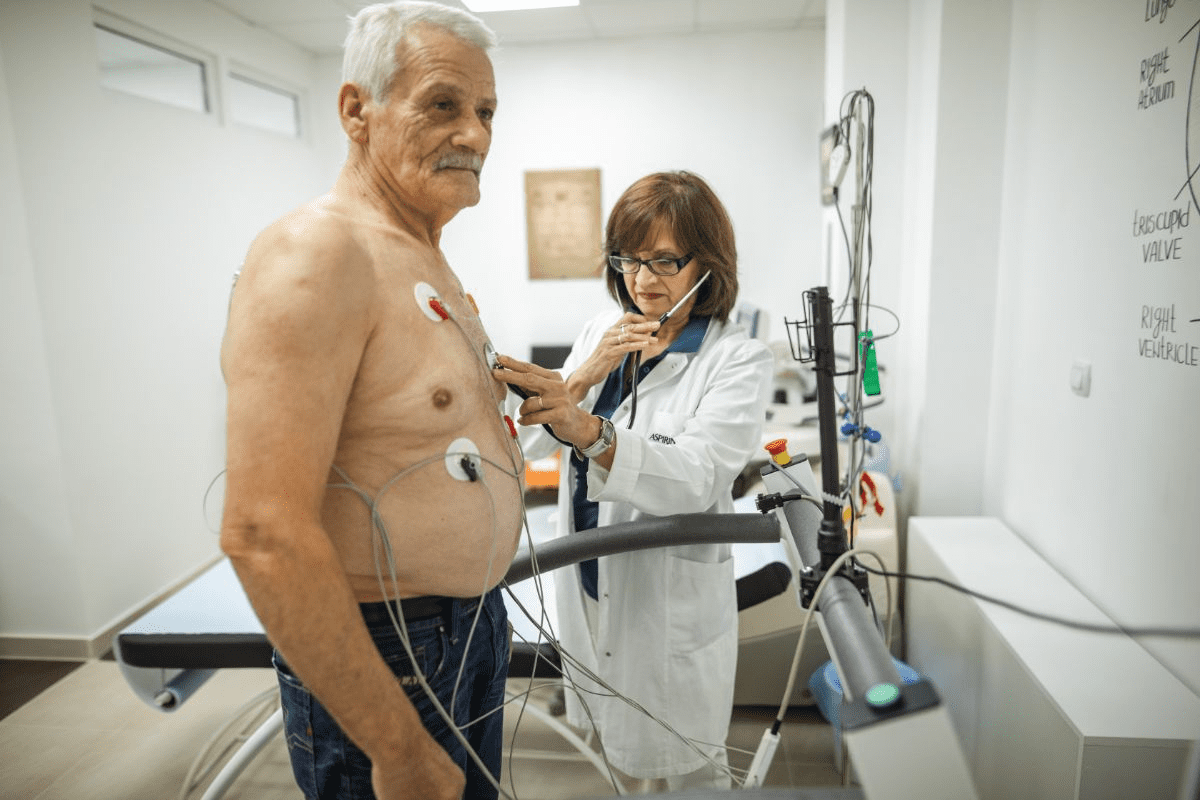
How Doctors Determine Your CKD Stage
Doctors figure out your CKD stage by looking at two things: your glomerular filtration rate (GFR) and kidney damage markers like albuminuria. GFR shows how well your kidneys filter waste. Albuminuria means your kidneys are damaged because it finds albumin in your urine.
To find your CKD stage, doctors use:
- GFR tests to check kidney function
- Urine tests for albuminuria and other kidney damage signs
- Imaging tests to see the kidneys and find any problems
The Role of Albuminuria in Classification
Albuminuria, or albumin in your urine, is a big sign of kidney damage. It’s very important in figuring out your CKD stage. The amount of albuminuria helps show how bad the kidney damage is, along with your GFR.
The table below shows how CKD stages are based on GFR and albuminuria levels:
| CKD Stage | GFR Level (mL/min/1.73m2) | Albuminuria Level |
| 1 | >90 | Present |
| 2 | 60-89 | Present |
| 3a | 45-59 | Varies |
| 3b | 30-44 | Varies |
| 4 | 15-29 | Varies |
| 5 | Varies |
Understanding your CKD stage and what affects it, like GFR and albuminuria, helps doctors make better treatment plans. This can slow down the disease and improve your health.
Stage 1 CKD: Normal Kidney Function with Damage
Stage 1 CKD means your kidneys work fine but show signs of damage. Even though they’re okay, tests can spot problems.
Finding kidney damage early is key to managing CKD well. We use different tools to catch it early.
Identifying Early Kidney Damage
Spotting early kidney damage needs urine tests, imaging, and more. Urine tests can find protein or blood, signs of kidney trouble.
Diagnostic Tests for Early Kidney Damage:
- Urine albumin-to-creatinine ratio test
- Serum creatinine test to estimate GFR
- Imaging tests like ultrasound or CT scans
- Kidney biopsy in some cases
Management Strategies for Stage 1
Managing Stage 1 CKD means slowing it down and fixing the root causes. Changing your lifestyle and getting medical help are key.
Key Management Strategies:
| Strategy | Description |
| Control Blood Pressure | High blood pressure can make CKD worse. Keeping it in check helps slow it down. |
| Manage Diabetes | For those with diabetes, keeping blood sugar levels right is vital to protect the kidneys. |
| Lifestyle Changes | Eating well, exercising, and not smoking can greatly help manage CKD. |
By using these strategies, we can manage Stage 1 CKD well. This might even stop it from getting worse.
Stage 2 CKD: Mild Kidney Damage (GFR 60-89)
In Stage 2 CKD, the GFR is between 60 and 89. This shows mild kidney damage. At this point, kidney issues are more serious than in Stage 1. Yet, symptoms might be small or not there at all. We will look at early signs, symptoms, and how to treat Stage 2 CKD.
Early Signs and Symptoms
At Stage 2 CKD, people might not feel any symptoms. This makes regular doctor visits key for catching problems early. Some signs include:
- Swelling in the feet, ankles, or face due to fluid retention
- Changes in urination patterns, such as frequency or color
- Fatigue or weakness
These signs can be hard to spot. It’s important to see a doctor if you notice anything off.
Treatment Approaches for Stage 2
Dealing with Stage 2 CKD needs a few steps. We aim to slow the disease and handle related health problems. Here’s what we suggest:
- Keep an eye on kidney function with regular GFR tests
- Manage conditions like diabetes and high blood pressure
- Live a healthy life with a balanced diet and exercise
Medications might be needed for related issues. And lifestyle changes are key in fighting CKD.
Knowing about Stage 2 CKD and using the right treatments can help manage the condition. It also lowers the chance of more kidney damage.
Stage 3 CKD: Moderate Kidney Damage
Understanding Stage 3 CKD is key for patients to manage their condition well. At this stage, kidney function is greatly reduced. But, there’s a lot that can be done to slow the disease’s progress.
Stage 3 CKD is split into two parts: 3a and 3b, based on the eGFR. This split helps in creating management plans based on the kidney damage’s severity.
Stage 3a (GFR 45-59): What to Expect
In Stage 3a CKD, patients may notice symptoms due to reduced kidney function. Common symptoms include fatigue, weakness, and swelling in the legs and feet. “The kidneys play a vital role in maintaining overall health,” says a nephrology expert. “At Stage 3a, it’s vital to monitor kidney function closely and adjust lifestyle habits.”
Management strategies include controlling blood pressure, managing diabetes, and dietary changes. Patients are advised to follow a kidney-friendly diet, limiting sodium, potassium, and phosphorus.
Stage 3b (GFR 30-44): Critical Differences
Stage 3b CKD shows more advanced kidney damage than Stage 3a. Symptoms can become more severe, and the risk of complications like anemia and bone disease increases.
Patients with Stage 3b CKD need more intense management. This includes regular checks of eGFR, electrolyte levels, and hemoglobin. “It’s critical for patients to work closely with their healthcare provider to manage symptoms and slow disease progression,” emphasizes a healthcare professional.
Treatment may include medications to manage symptoms and slow CKD progression. Lifestyle changes are also key, focusing on a healthy diet, regular exercise, and avoiding smoking.
In conclusion, Stage 3 CKD, whether 3a or 3b, needs careful management to prevent further kidney damage. By understanding each substage and working with healthcare providers, patients can manage their condition and improve their quality of life.
Stage 4 CKD: Severe Kidney Damage (GFR 15-29)
Stage 4 CKD means severe kidney damage, with a GFR of 15-29. Patients at this stage are at high risk of kidney failure. It’s vital to manage symptoms and slow disease progression.
Recognizing Advancing Symptoms
As CKD reaches Stage 4, symptoms worsen and affect daily life. Common signs include:
- Nausea and vomiting
- Loss of appetite
- Fatigue and weakness
- Swelling in the legs and feet
- Difficulty breathing
These symptoms show the kidneys can’t filter waste and fluids well. It’s key for patients to work with their healthcare team to manage these symptoms.
Preparing for Possible Renal Replacement Therapy
At Stage 4 CKD, preparing for renal replacement therapy (RRT) is essential. RRT includes dialysis or a kidney transplant. Preparing involves:
- Learning about different dialysis types and their effects
- Checking if a kidney transplant is right for you
- Making lifestyle changes for future RRT
Talking about financial and social support with healthcare providers
Early preparation can greatly improve outcomes and quality of life. We suggest patients and their families talk openly with their healthcare team about the best steps.
Understanding Stage 4 CKD’s severity and taking proactive steps helps patients navigate this critical phase. Our healthcare team is dedicated to providing full support and guidance on this journey.
Stage 5 CKD: Kidney Failure (GFR Below 15)
When you reach Stage 5 CKD, your kidneys are failing badly. You’ll need to make big changes in your life and get medical help. Your kidneys can’t remove waste and balance fluids like they should.
Life with End-Stage Renal Disease
At Stage 5 CKD, also known as end-stage renal disease (ESRD), you might feel very tired, weak, and confused. These feelings can make everyday tasks hard to do.
You might also get swelling in your legs, shortness of breath, and nausea. To manage these symptoms, you’ll need a treatment plan that covers both your body and mind.
Treatment Options: Dialysis and Transplantation
For Stage 5 CKD, you’ll need a treatment to keep you alive. The main choices are dialysis and kidney transplantation.
- Dialysis uses a machine to filter your blood outside your body, like healthy kidneys do.
- Kidney transplantation means getting a healthy kidney from someone else, which can make your life more normal.
Dialysis can be done at home or in a center, but it’s a big time commitment. Kidney transplantation offers more freedom but requires surgery and lifelong medicine to stop your body from rejecting the new kidney.
Choosing the right treatment depends on many things, like your health, lifestyle, and what you prefer. It’s important to talk to your doctor to figure out the best option for you.
The Role of Creatinine in Diagnosing CKD Stages
Creatinine in the blood is key for checking kidney health and CKD stages. It’s a waste from muscle breakdown. Healthy kidneys remove it, but impaired kidneys let it build up.
How Serum Creatinine Relates to GFR
Serum creatinine helps calculate the eGFR, a key for CKD stages. The eGFR shows how well kidneys filter waste. A higher creatinine means worse kidney function and a lower eGFR.
The eGFR is better than serum creatinine alone for CKD staging. But, remember, eGFR is an estimate. It can be affected by age, sex, and race.
| CKD Stage | GFR Level (mL/min/1.73m2) | Serum Creatinine Level |
| 1 | >90 | Normal |
| 2 | 60-89 | Normal or slightly elevated |
| 3a | 45-59 | Elevated |
| 3b | 30-44 | заметно elevated |
| 4 | 15-29 | High |
| 5 | Very High |
Interpreting Your Creatinine Test Results
Understanding your creatinine test results is important. High levels mean your kidneys are not working well. But, how fast they rise matters too. A quick jump might mean acute kidney injury, while a slow rise suggests CKD getting worse.
“Knowing your creatinine levels and how they affect your kidneys is vital for managing CKD. By working with your healthcare provider, you can slow the disease and keep your health in check.”
Talk to your healthcare provider about your creatinine test results. They can explain what they mean and help you manage your CKD.
Common Symptoms Across All CKD Stages
It’s important to know the symptoms of CKD at all stages for early treatment. CKD is a condition where the kidneys slowly lose function. As it gets worse, symptoms can really affect a person’s life.
Early Warning Signs Often Overlooked
In the early stages, symptoms are often mild and easy to miss. Common signs include fatigue, swelling in the legs and feet, and changes in urine output. These signs can be hard to spot without a doctor’s help.
People with risk factors like diabetes or high blood pressure should watch for these signs. Regular doctor visits can catch kidney problems early.
Late-Stage Symptoms Requiring Immediate Attention
In later stages, symptoms get worse and can include shortness of breath, chest pain, and severe fatigue. Stage 5 CKD, or ESRD, means the kidneys almost stop working. Symptoms can be very serious.
If you have severe swelling, confusion, or persistent nausea, get help right away. These signs mean your kidneys are failing fast. You might need dialysis or a transplant.
Knowing the symptoms of CKD is key to managing it well. Being aware of early and late signs helps patients work with doctors. This can slow the disease and improve health.
Slowing CKD Progression: Evidence-Based Strategies
Slowing Chronic Kidney Disease (CKD) needs a mix of lifestyle changes and medical treatments. These strategies can greatly improve life quality and may delay kidney failure.
Lifestyle Modifications That Make a Difference
Lifestyle changes are key in managing CKD. Dietary changes are very important. Eating less protein, less sodium, and avoiding high phosphorus foods can slow disease progress. Also, keeping a healthy weight through diet and exercise is good.
Exercise is also vital. It helps manage weight, lowers blood pressure, and boosts heart health. Aim for 30 minutes of moderate exercise daily.
“Lifestyle changes are fundamental in slowing CKD progression. By making informed choices about diet and exercise, patients can take an active role in managing their condition.”
| Lifestyle Modification | Benefit |
| Dietary Changes | Reduces strain on kidneys |
| Regular Exercise | Improves cardiovascular health |
| Weight Management | Reduces risk of complications |
Medical Interventions by Stage
Medical treatments vary by CKD stage. For stages 1-2, controlling high blood pressure and diabetes is key. Stages 3-4 might involve medications like ACE inhibitors or ARBs to slow disease.
In stage 4, preparing for dialysis or a kidney transplant is important. This includes creating a vascular access for dialysis.
It’s vital for patients to work with their doctors to find the right treatment. This depends on their specific needs and CKD stage.
Conclusion: Living Well with CKD
Living with chronic kidney disease (CKD) needs a full plan to manage it. Knowing the different stages and their GFR levels helps patients act early. This can slow down the disease.
Managing CKD well means making lifestyle changes, getting medical help, and keeping an eye on your health. We talked about how to manage CKD, from changing your diet to using renal replacement therapy.
With the right care, people with CKD can live full and happy lives. Working with doctors and following a treatment plan can improve life quality. It also lowers the chance of serious problems.
Dealing with CKD is a big commitment, but it’s doable. We urge patients to stay informed, ask questions, and get support. This way, they get the best care possible.
FAQ
What are the 5 stages of Chronic Kidney Disease (CKD)?
CKD has five stages. They are based on the Glomerular Filtration Rate (GFR) levels. The stages range from normal kidney function (Stage 1) to kidney failure (Stage 5).
How is GFR used to determine CKD stages?
GFR measures how well kidneys filter fluid. It shows the volume of filtered fluid per minute. Lower GFR levels mean more severe kidney damage.
What is the difference between GFR and eGFR?
GFR directly measures kidney function. eGFR is an estimated value based on age, sex, and serum creatinine levels. eGFR is often used to diagnose and monitor CKD.
What are the symptoms of CKD, and how do they vary by stage?
Symptoms of CKD vary by stage. Early stages may have few or no symptoms. As CKD worsens, symptoms include fatigue, swelling, and changes in urination.
How is CKD staged, and what is the role of albuminuria in classification?
CKD stages are based on GFR levels. Albuminuria, or albumin in the urine, is key in classification. It shows kidney damage and predicts disease progression.
What are the characteristics of Stage 3 CKD, and how does it differ from other stages?
Stage 3 CKD has moderate kidney damage. GFR levels are between 30-59. It’s divided into Stage 3a (GFR 45-59) and Stage 3b (GFR 30-44). Stage 3b shows more severe damage.
How can CKD progression be slowed or managed?
Slowing CKD progression involves lifestyle changes. These include a healthy diet, regular exercise, and managing conditions like hypertension and diabetes. Medications and renal replacement therapy may also be needed.
What are the treatment options for Stage 5 CKD?
Stage 5 CKD, or end-stage renal disease, has two main treatments. These are dialysis and kidney transplantation. They aim to replace lost kidney function and manage symptoms.
How does creatinine relate to CKD stages, and what do creatinine test results indicate?
Creatinine levels help diagnose CKD. High levels indicate poor kidney function. Higher levels mean more severe damage.
What are the common symptoms across all CKD stages, and why is it essential to recognize them?
Common symptoms include fatigue, swelling, and changes in urination. Recognizing these symptoms is key. CKD can progress silently until it’s advanced.
What lifestyle modifications can help manage CKD?
Managing CKD involves lifestyle changes. These include a healthy diet, regular exercise, and managing conditions. These can slow CKD progression and improve health.
How do doctors determine the stage of CKD?
Doctors evaluate GFR levels, albuminuria, and other factors. These include medical history and physical examination. This helps determine the CKD stage.
References
National Center for Biotechnology Information. (2025). 5 CKD Stages GFR Levels Symptoms Classification. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC3100281/