Last Updated on October 31, 2025 by Batuhan Temel
At Liv Hospital, we aim to provide top-notch healthcare. We support international patients fully. We’re looking into how potassium channel blockers help with heart rhythm problems.
Learn about class III antiarrhythmics and potassium channel blocker functions.
Class III antiarrhythmics, or potassium channel blockers, are key in treating irregular heartbeats. They do this by making the heart’s recovery time longer. Drugs like amiodarone, dofetilide, ibutilide, and sotalol are examples of these life-saving treatments.
It’s important for doctors to know how these drugs work and when to use them. In this article, we’ll share seven key facts about Class III antiarrhythmics. This will help us understand their role in heart health.
The heart’s electrical system is complex and can be affected by many factors. This leads to arrhythmias. To understand how arrhythmias happen and how they’re treated, we need to know the basics of cardiac electrical activity.
The cardiac conduction system controls the heartbeat. It includes the SA node, AV node, Bundle of His, and Purkinje fibers. The SA node is the heart’s natural pacemaker, starting electrical impulses at 60-100 beats per minute.
Arrhythmias happen when the heart’s electrical system is disrupted. This can be due to problems with impulse formation or conduction. For example, if the SA node fires too quickly or too slowly, it can cause tachycardia or bradycardia. A blockage in the conduction pathway can also lead to arrhythmias.
“Arrhythmias can be caused by a variety of factors, including electrolyte imbalances, medication side effects, and underlying heart conditions.”
Antiarrhythmic medications are grouped based on how they work. The Vaughan-Williams classification is commonly used. It divides these drugs into four classes. Class III antiarrhythmics block potassium channels, lengthening the repolarization phase and increasing the refractory period.
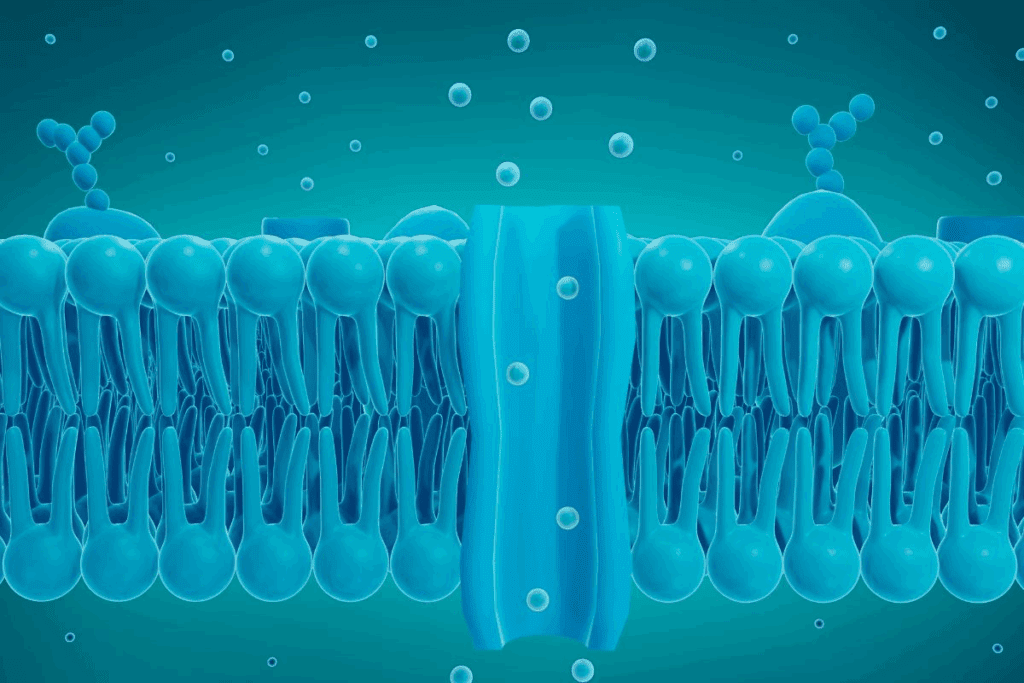
Class III antiarrhythmics work by blocking potassium channels. This helps keep the heart rhythm stable. They are key in treating heart rhythm problems.
Class III antiarrhythmics extend the repolarization phase of the heart’s action. They do this by blocking potassium channels. These channels are vital for repolarization.
By blocking these channels, Class III drugs delay repolarization. This makes the heart’s refractory period longer. This helps stop reentrant arrhythmias.
Class III drugs affect different potassium channels in the heart. The rapid and slow components of the delayed rectifier potassium current (IKr and IKs) are key. Some drugs, like amiodarone, affect even more channels.
The blockade of IKr is very important. It affects the QT interval on the electrocardiogram. While this can be beneficial, too much prolongation can cause dangerous arrhythmias.
The development of Class III antiarrhythmics has taken decades. Early drugs had limited specificity and side effects. Amiodarone, developed in the 1960s, was first used as a vasodilator but later found to have antiarrhythmic effects.
Later, more targeted drugs like dofetilide and ibutilide were developed. These newer agents aim to reduce side effects and improve effectiveness.
Prolonged repolarization is key for Class III antiarrhythmics. It helps prevent arrhythmias by affecting the heart’s rhythm. This is vital for keeping the heart beating steadily and safely.
Class III antiarrhythmics mainly work by slowing down repolarization. They do this by blocking potassium channels. These channels are important for the heart’s repolarization phase.
Medical Expert, a well-known cardiologist, says, “Prolonging repolarization is a key part of Class III antiarrhythmic therapy. It helps manage arrhythmias better.”
“The use of Class III antiarrhythmics has changed how we treat arrhythmias. It offers a great option for those at risk of serious arrhythmias.”
The cardiac action has several phases, with phases 2 and 3 being key for repolarization. Class III antiarrhythmics extend these phases by blocking potassium channels. This makes it harder for arrhythmias to start.
The effective refractory period (ERP) is when the heart can’t be excited again. Class III antiarrhythmics make this period longer. This helps protect against arrhythmias caused by early electrical signals.
The increase in ERP is central to Class III antiarrhythmics’ action. Knowing how they work is key to understanding their benefits and risks.
The Class III antiarrhythmics category includes several key drugs. These medications block potassium channels to treat cardiac arrhythmias. Each drug has its own unique characteristics and uses.
Amiodarone is the most well-known Class III antiarrhythmic. It affects multiple ion channels, making it effective for many arrhythmias. Its broad efficacy comes with a complex side effect profile, requiring careful patient monitoring.
Dofetilide is a more selective potassium channel blocker than amiodarone. It’s mainly used for maintaining sinus rhythm in patients with atrial fibrillation or flutter. Its selectivity reduces some side effects, but it can cause QT prolongation and Torsades de Pointes.
Ibutilide is used for quickly converting atrial fibrillation or flutter to sinus rhythm. It prolongs action potentials and increases refractoriness. Its rapid action is useful in scenarios where quick rhythm restoration is needed.
Sotalol is unique because it blocks beta receptors in addition to potassium channels. This makes it effective for many arrhythmias and provides rate control. But, its beta-blocking effects need careful consideration, mainly in patients with certain comorbidities.
In conclusion, the major drugs in Class III antiarrhythmics each have their own strengths and uses. Understanding these differences is key to choosing the right medication for each patient.
Class III antiarrhythmics have changed how we treat heart rhythm problems. They help manage atrial fibrillation and flutter, treat ventricular tachycardia, and prevent sudden cardiac death.
Atrial fibrillation and flutter can really affect a person’s life. Class III antiarrhythmics help bring the heart back to a normal rhythm. Amiodarone and sotalol are good at stopping atrial fibrillation and keeping it from coming back.
Doctors pick the right medicine based on the patient’s health and how long they’ve had the problem.
Ventricular tachycardia is a serious heart rhythm problem that needs quick action. Class III antiarrhythmics, like amiodarone and lidocaine (though lidocaine is not a pure Class III), stop ventricular tachycardia and prevent it from coming back.
In emergencies, these medicines are given through an IV to quickly fix the heart rhythm. For ongoing care, patients might take oral versions of these drugs to stop it from happening again.
Sudden cardiac death (SCD) is a big worry for people with heart rhythm problems or heart disease. Class III antiarrhythmics, like amiodarone, help lower the risk of SCD by stopping dangerous heart rhythms.
Using implantable cardioverter-defibrillators (ICDs) with Class III antiarrhythmics can lower SCD risk even more. These medicines help cut down on arrhythmia events, which improves patient results.
Amiodarone is special because it blocks many channels in the heart. It’s not just a potassium blocker. It also affects sodium and calcium channels.
Amiodarone blocks sodium and calcium channels, too. This helps it treat many arrhythmias. It slows the heart’s electrical signals and reduces muscle contraction.
This makes amiodarone very useful. It works on different channels to treat various heart rhythm problems.
Amiodarone does block calcium channels, but it’s not just a calcium blocker. It blocks many channels, making it versatile. This is why it’s different from other heart medications.
Amiodarone’s body handling is complex. It stays in the body for a long time. This can cause side effects like thyroid problems and lung issues.
Class III antiarrhythmics can cause QT prolongation, raising the risk of a serious heart rhythm problem called torsades de pointes. This happens because these drugs make the QT interval longer. The QT interval is how long it takes for the heart’s ventricles to get ready for the next beat.
The QT interval is from the start of the Q wave to the end of the T wave in the heart’s electrical cycle. It shows how long the heart takes to repolarize. A long QT interval can lead to dangerous heart rhythms.
Torsades de pointes is a fast, irregular heartbeat linked to a long QT interval. It can turn into ventricular fibrillation, causing sudden death if not treated fast. It starts with early afterdepolarizations during the long repolarization phase.
Many factors can increase the chance of getting torsades de pointes. These include hypokalemia, bradycardia, and drug interactions that lengthen the QT interval. To prevent it, we should watch the QT interval in patients on Class III antiarrhythmics. We also need to fix electrolyte imbalances and avoid other drugs that prolong the QT interval.
When we give Class III antiarrhythmics, we must think about the benefits and risks. This is very important for patients with risk factors for QT prolongation and torsades de pointes.
Class III antiarrhythmics are effective but come with many side effects. They are key in treating heart rhythm problems. But, doctors must watch out for these side effects and safety issues.
Each Class III antiarrhythmic has its own set of side effects. For example, amiodarone has many because of its iodine and long half-life. It can cause thyroid problems, lung issues, and skin reactions to sunlight.
| Drug | Common Adverse Effects | Serious Adverse Effects |
| Amiodarone | Thyroid dysfunction, pulmonary toxicity, skin photosensitivity | Hepatic toxicity, pulmonary fibrosis |
| Dofetilide | Headache, dizziness | Torsades de Pointes |
| Ibutilide | Nausea, headache | Sustained ventricular tachycardia |
| Sotalol | Fatigue, dizziness | Torsades de Pointes, bradycardia |
Class III antiarrhythmics can harm different body systems. Amiodarone, for example, can cause lung fibrosis, a serious condition. It’s important to watch for these toxicities to use these drugs safely.
These drugs can also interact with other medications, leading to serious problems. For example, mixing them with drugs that prolong the QT interval can cause dangerous heart rhythms. It’s vital to carefully review a patient’s medications to avoid these interactions.
Knowing the side effects and safety issues of Class III antiarrhythmics helps doctors use them better. This way, they can reduce risks for their patients.
Understanding how Class III antiarrhythmics work is key to their use. Their pharmacokinetics affects how well and safely they work. We’ll look at how they are absorbed, distributed, metabolized, and eliminated. We’ll also discuss how to dose them for different patients.
Class III antiarrhythmics absorb at different rates. For example, amiodarone’s lipophilic nature makes its absorption complex. On the other hand, dofetilide is absorbed quickly. Amiodarone’s lipophilic nature also means it spreads out in the body, reaching many tissues.
This affects how fast and long these drugs work. For instance, ibutilide’s quick distribution makes it good for sudden heart rhythm changes.
| Drug | Absorption Rate | Volume of Distribution |
| Amiodarone | Variable | Large |
| Dofetilide | Rapid | Moderate |
| Ibutilide | Rapid | Moderate |
How Class III antiarrhythmics are broken down and removed from the body is important. Amiodarone mainly breaks down in the liver, taking a long time to leave the body. Dofetilide is also broken down in the liver but more quickly.
How these drugs are removed from the body varies. For example, sotalol is mostly removed through the urine, so doses need to be adjusted in patients with kidney problems.
“The pharmacokinetics of antiarrhythmic drugs are complex and influenced by multiple factors, including patient-specific characteristics and drug interactions.”
— Journal of Clinical Pharmacology
Dosing Class III antiarrhythmics needs to be tailored for each patient. Elderly patients, for example, might need smaller doses because their kidneys work less efficiently. Patients with liver or kidney issues also need special consideration.
For instance, dofetilide’s dose depends on how well the kidneys are working to avoid heart rhythm problems. Amiodarone’s dose might need to be adjusted in patients with thyroid issues because of its iodine content.
By understanding how these drugs work and tailoring their doses, we can make them more effective and safer for everyone.
Understanding the differences between Class III antiarrhythmics and other classes is key in managing cardiac arrhythmias. Class III antiarrhythmics, also known as potassium channel blockers, have unique benefits and risks compared to other classes.
Class III antiarrhythmics are effective against various arrhythmias, like atrial fibrillation and ventricular tachycardia. Amiodarone, a Class III antiarrhythmic, is very effective in keeping the heart in a normal rhythm in patients with atrial fibrillation.
Class I antiarrhythmics (sodium channel blockers) work better for ventricular arrhythmias but not as well for atrial fibrillation. Class II antiarrhythmics (beta-blockers) are mainly used to control the heart rate in atrial fibrillation and prevent ventricular arrhythmias.
| Antiarrhythmic Class | Efficacy in Atrial Fibrillation | Efficacy in Ventricular Tachycardia |
| Class III (Potassium Channel Blockers) | High | High |
| Class I (Sodium Channel Blockers) | Low | High |
| Class II (Beta-Blockers) | Rate control | Moderate |
Class III antiarrhythmics are effective but carry a risk of QT prolongation and Torsades de Pointes. This risk is high with drugs like sotalol and dofetilide.
“The risk of Torsades de Pointes with Class III antiarrhythmics necessitates careful patient selection and monitoring.”
Class II antiarrhythmics (beta-blockers) have a safer profile but can cause bradycardia and hypotension. Class I antiarrhythmics can have dangerous effects, mainly in patients with heart disease.
The choice between Class III antiarrhythmics and other classes depends on the arrhythmia and the patient’s health. For example, in atrial fibrillation with heart failure, amiodarone is often chosen for its effectiveness.
Choosing an antiarrhythmic class should be based on the patient’s health and the arrhythmia’s characteristics.
Using Class III antiarrhythmics well means knowing how they work, their uses, and possible side effects. We’ve covered the main points about these drugs. They help by making the heart’s electrical cycle longer and are used for different heart rhythm problems.
When choosing a Class III antiarrhythmic, we must think about each patient’s needs and health history. Creating a treatment plan that fits each patient and keeping a close eye on them is key. This way, we can get the most benefits with the least risks.
Knowing the special features of each Class III antiarrhythmic, like amiodarone’s effects on multiple channels, helps us make better choices. This knowledge helps us improve treatment results and care for our patients better.
As we move forward in cardiology, keeping up with new research and guidelines on Class III antiarrhythmics is vital. This ensures our patients get the top care for their heart rhythm issues.
Class III antiarrhythmic drugs are special medicines. They block potassium channels in the heart. This action helps manage heart rhythm problems.
These drugs block potassium channels. This delay in heart repolarization makes the heart action longer. It also makes the heart less likely to have arrhythmias.
The main drugs in this class are amiodarone, dofetilide, ibutilide, and sotalol. Each is used for different heart rhythm issues.
Yes, amiodarone blocks potassium channels. It also affects sodium and calcium channels, making it a multi-channel blocker.
Amiodarone does block calcium channels a bit. But, it’s mainly known for blocking potassium channels. It has effects on other channels too.
These drugs can cause the QT interval to get longer. This increases the risk of a dangerous heart rhythm called torsades de pointes.
Managing this risk involves watching the QT interval and fixing any electrolyte imbalances. It’s also important to avoid other drugs that can prolong the QT interval. Dosages may need to be adjusted based on how the patient responds and their risk factors.
Side effects vary by drug but can include specific issues and organ damage. For example, amiodarone can harm the lungs. It’s also important to watch for drug interactions, which can be dangerous.
These drugs are compared to others based on how well they work and their safety. They offer a unique way to treat heart rhythm problems, which can be beneficial in some cases.
These drugs are key in treating atrial fibrillation. They help keep the heart in a normal rhythm and control the heart rate. Drugs like amiodarone and sotalol are often used for this.
Yes, drugs like amiodarone can help prevent sudden cardiac death. They do this by reducing the risk of dangerous heart rhythms in high-risk patients.
National Center for Biotechnology Information. (2025). 7 Key Facts About Class III Antiarrhythmics Potassium. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/11607542
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us