Cranial nerve palsies are a big deal in the world of brain health. They happen when the twelve cranial nerves coming out of the brain and brainstem get messed up. These nerves are key for things like moving your eyes and opening your eyelids. What are CN palsies? Our essential guide explains how these alarming nerve issues (CN 3, 4, 6) cause double vision and droopy eyelids.
When these nerves don’t work right, you might see double or have eyelids that droop. At Liv Hospital, we get how cranial nerve palsies can mess with your eyes. We focus on you, making sure you get the best care for your eye problems.
Key Takeaways
- Cranial nerve palsies involve paralysis or weakness of muscles controlled by cranial nerves.
- These conditions significantly impact ocular motor function and overall eye health.
- Symptoms include double vision, drooping eyelids, and difficulty moving the eyes.
- Understanding causes, symptoms, and treatment options is key for managing them well.
- Getting expert help is vital for those dealing with cranial nerve palsy symptoms.
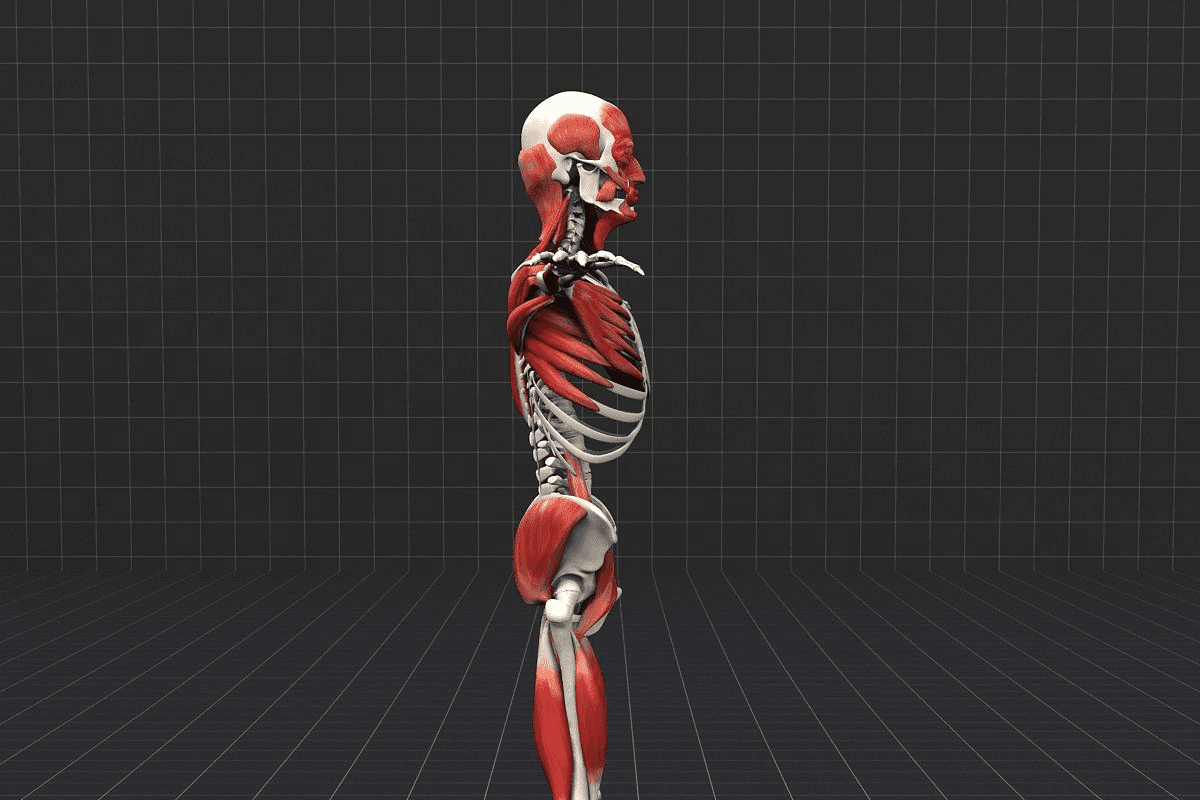
The Cranial Nerve System and Visual Function
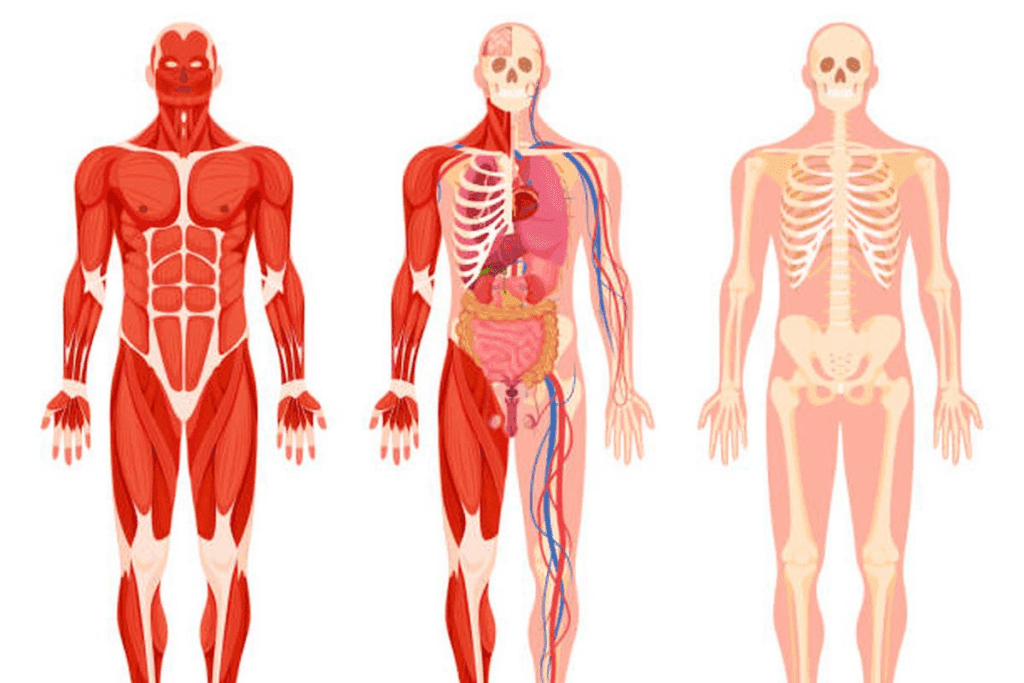
The cranial nerve system is key for eye movement and more. It has 12 pairs of nerves. These nerves help the brain talk to the body, including the eyes.
The 12 Cranial Nerves: From Brain to Body
The 12 cranial nerves do many things. They help with eye movements, smell, and hearing. Each nerve is named based on its function or what it connects to.
Let’s look at each of the 12 cranial nerves:
- Olfactory Nerve (I): It sends smell information to the brain.
- Optic Nerve (II): It carries visual info from the retina to the brain.
- Oculomotor Nerve (III): It controls most eye movements, eyelid opening, and pupil size.
- Trochlear Nerve (IV): It works with the superior oblique muscle to rotate the eyeball.
- Trigeminal Nerve (V): It handles facial sensation and chewing.
- Abducens Nerve (VI): It controls the lateral rectus muscle for outward eye movement.
- Facial Nerve (VII): It manages facial expressions, taste, and more.
- Vestibulocochlear Nerve (VIII): It’s linked to hearing and balance.
- Glossopharyngeal Nerve (IX): It’s involved in swallowing, salivation, and taste.
- Vagus Nerve (X): It controls heart rate, digestion, and more.
- Accessory Nerve (XI): It helps with neck and shoulder movements.
- Hypoglossal Nerve (XII): It controls tongue movements.
How Cranial Nerves Control Eye Movement and Vision
The third, fourth, and sixth cranial nerves control eye movements. The Oculomotor Nerve (III) handles most eye movements and eyelid opening. The Trochlear Nerve (IV) works with the superior oblique muscle, and the Abducens Nerve (VI) moves the eye outward.
These nerves work together for smooth eye movements. Any problem can cause issues like cranial nerve palsies. This can really affect vision and eye movement.
For example, sixth cranial nerve palsy is more common, affecting people over 60. It went from 3.92 per 100,000 in 2006 to 10.08 per 100,000 in 2015.
Cranial Nerve | Function |
Oculomotor (III) | Controls most eye movements, eyelid opening, and pupil constriction |
Trochlear (IV) | Innervates the superior oblique muscle, rotating the eyeball |
Abducens (VI) | Controls the lateral rectus muscle, responsible for outward eye movement |
Knowing about these nerves is key for treating eye problems. As we learn more about cranial nerve palsies, we see how important it is to understand the cranial nerve system. This knowledge helps us care for patients better.
What Are CN Palsies? Understanding the Basics
‘Cranial nerve palsy’ means damage to one or more of the twelve cranial nerves that start from the brain. These nerves help with eye movements, facial expressions, and swallowing. Damage to a nerve can cause different symptoms, depending on the nerve.
Definition and Mechanism of Cranial Nerve Palsy
Cranial nerve palsies can happen for many reasons, like tumors, inflammation, or trauma. Damage to these nerves can cause problems like vision loss, double vision, and a drooping eyelid. Knowing how cranial nerve palsies work is key to treating them.
The oculomotor nerve (CN III) is important for eye movements. Damage to it can cause a third nerve palsy, leading to a drooping eyelid and double vision. The trochlear nerve (CN IV) and abducens nerve (CN VI) also control eye movements. Their problems can cause specific double vision.
Epidemiology: Who Gets Affected and How Often
The frequency of cranial nerve palsies varies by nerve and cause. For example, fourth cranial nerve palsy happens at a rate of 5.73 per 100,000 people per year. It often affects people in their 40s. Early detection is important.
Studying cranial nerve palsies can give us important information. The table below shows some key findings:
Cranial Nerve | Incidence per 100,000 per year | Common Causes |
Third (Oculomotor) | Variable | Diabetes, aneurysms |
Fourth (Trochlear) | 5.73 | Congenital, trauma |
Sixth (Abducens) | 4.66 | Trauma, vascular issues |
The table shows that the incidence and causes of cranial nerve palsies differ. Knowing this helps doctors find and help at-risk groups.
“Cranial nerve disorders can result from a wide range of causes, including tumors, inflammation, trauma, systemic disorders, and degenerative or other processes, causing symptoms such as vision loss, diplopia, ptosis, and pupillary abnormalities.” This highlights the complexity and variability of cranial nerve palsies, stressing the need for detailed diagnostic methods.
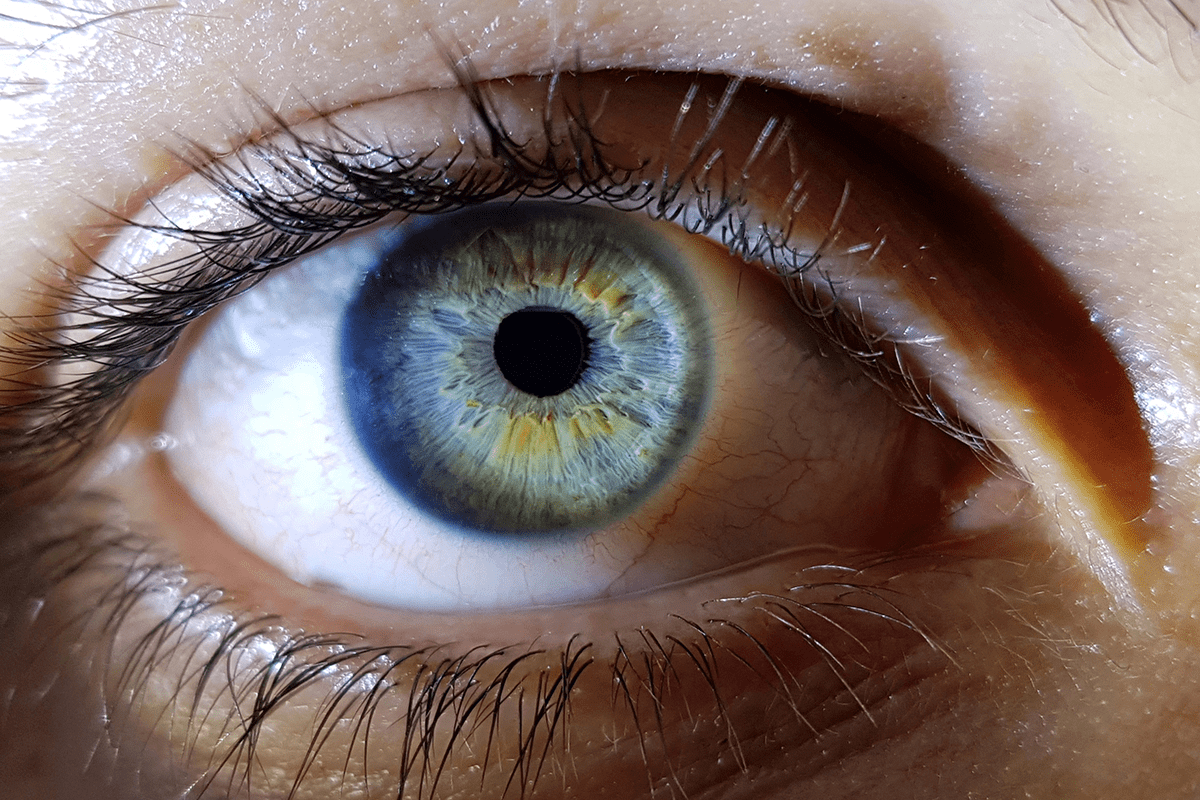
Anatomy of Eye-Related Cranial Nerves
Cranial nerves are vital for eye movement control. Their anatomy helps us understand palsies related to the eyes. These nerves work together to ensure smooth eye movements.
Oculomotor Nerve (CN III): The Primary Eye Movement Controller
The oculomotor nerve, or CN III, controls most eye movements. It rotates the eyeball, constricts the pupil, and keeps the eyelid open. Problems with this nerve can cause ptosis, or eyelid drooping, affecting vision and appearance.
Trochlear Nerve (CN IV): The Smallest Yet Crucial Nerve
The trochlear nerve, or CN IV, is the thinnest and longest cranial nerve. It controls the superior oblique muscle, which rotates the eyeball downward. Trochlear nerve palsy can cause vertical and torsional diplopia, or double vision, worse when looking down.
Abducens Nerve (CN VI): The Lateral Gaze Specialist
The abducens nerve, or CN VI, controls the lateral rectus muscle for outward gaze. It’s key for sideways vision. Abducens nerve palsy prevents eye abduction, causing horizontal diplopia. This makes everyday navigation hard.
Other Nerves Affecting Eye Function
Other cranial nerves also play a role in eye function. The trigeminal nerve (CN V) sends sensory signals to the face, including the eyes. The facial nerve (CN VII) controls facial muscles, including those around the eyes. Knowing their roles is key to diagnosing eye-related conditions.
Types of Ocular Cranial Nerve Palsies
It’s important to know about the different types of ocular cranial nerve palsies. This knowledge helps in diagnosing and treating visual problems. Each type affects a specific nerve, leading to unique symptoms.
Third Nerve (Oculomotor) Palsy: Symptoms and Characteristics
The third cranial nerve controls eye movements, pupil constriction, and eyelid opening. Damage to this nerve can cause ptosis (drooping eyelid), eye movement issues, and a dilated pupil.
Causes of third nerve palsy include diabetes, high blood pressure, and trauma. Symptoms vary based on the nerve damage’s extent and whether it’s partial or complete.
Fourth Nerve (Trochlear) Palsy: The 5.73 per 100,000 Condition
The fourth cranial nerve controls the superior oblique muscle for eye rotation. Fourth nerve palsy causes vertical diplopia (double vision), where images are vertically displaced.
This condition affects about 5.73 per 100,000 people. It can stem from trauma, vascular issues, or birth defects. A detailed eye exam is needed for diagnosis.
Sixth Nerve (Abducens) Palsy: Understanding the 4.66 per 100,000 Incidence
The sixth cranial nerve controls the lateral rectus muscle for outward eye movement. Sixth nerve palsy results in horizontal diplopia, where images are horizontally displaced.
It affects about 4.66 per 100,000 people. Causes include vascular diseases, trauma, and increased brain pressure. A thorough evaluation is essential for treatment.
Multiple Cranial Nerve Palsies: When More Than One Nerve Is Affected
Sometimes, more than one cranial nerve is affected. This leads to complex symptoms like ptosis, diplopia, and limited eye movements.
Diagnosing and treating multiple cranial nerve palsies is complex. It requires a team effort from neurologists, ophthalmologists, and other specialists. Treatment depends on the cause and nerve involvement.
Visual Symptoms and Manifestations
Cranial nerve palsies can cause a range of visual symptoms. These include drooping eyelids, double vision, and eyes that don’t align properly. These issues happen because the nerves that control eye movement are affected.
Ptosis: When Your Eyelid Droops
Ptosis, or a drooping eyelid, is a common sign of third cranial nerve palsy. It happens when the nerve that controls the levator palpebrae superioris muscle is damaged. This can lead to weakness or paralysis of the muscle. Ptotic eyelids can make it hard to see and often come with double vision.
Diplopia: The Challenge of Double Vision
Diplopia, or double vision, is a common problem with cranial nerve palsies. It occurs when the nerves that control the extraocular muscles are damaged. This misalignment causes the brain to see two images, leading to double vision. The type of double vision depends on which nerves are affected.
- Horizontal diplopia is often associated with sixth nerve palsy.
- Vertical diplopia can occur with third or fourth nerve palsies.
- Torsional diplopia is less common but can be seen in fourth nerve palsies.
Strabismus: When Eyes Don’t Align
Strabismus is when the eyes don’t line up properly. This can happen due to palsies of the third, fourth, or sixth cranial nerves. The severity of strabismus varies based on the nerve affected. For example, third nerve palsy can cause the eye to point outward and downward.
Pupillary Changes and Other Visual Disturbances
Pupillary changes, like dilation or constriction, can also happen in cranial nerve palsies. A dilated pupil might indicate a serious issue, like an aneurysm. Other symptoms include blurred vision, trouble moving the eyes, and light sensitivity.
- Pupillary dilation is often seen in third nerve palsy.
- Some patients may experience pupillary constriction.
- Other visual disturbances can include blurred vision and sensitivity to light.
Causes and Risk Factors of Cranial Nerve Palsies
Understanding the causes and risk factors of cranial nerve palsies is key to effective treatment. These palsies can stem from various conditions. Knowing these factors helps in providing the right care.
Vascular Conditions: Diabetes, Hypertension, and Stroke
Certain vascular conditions, like diabetes and hypertension, raise the risk of cranial nerve palsies. These conditions can harm the blood vessels that supply the nerves, causing palsy. For example, diabetes can lead to third cranial nerve palsy due to blood vessel damage.
Vascular Condition | Risk Factor for Cranial Nerve Palsy | Commonly Affected Nerve |
Diabetes | Microvascular ischemia | Third cranial nerve (CN III) |
Hypertension | Vascular damage | Sixth cranial nerve (CN VI) |
Stroke | Ischemia or hemorrhage affecting cranial nerve nuclei or pathways | Multiple cranial nerves |
Trauma and Injury to Cranial Nerves
Head or neck trauma can cause cranial nerve palsies by damaging the nerves or their surroundings. The severity and location of the trauma determine which nerves are affected.
Common traumatic causes include:
- Head injuries from accidents or falls
- Surgical complications
- Penetrating injuries
Inflammatory and Infectious Processes
Inflammatory and infectious processes can also lead to cranial nerve palsies. Conditions like meningitis, encephalitis, and sarcoidosis can cause inflammation that damages the nerves.
Examples of inflammatory and infectious causes:
- Meningitis
- Encephalitis
- Sarcoidosis
- Lyme disease
Tumors and Space-Occupying Lesions
Tumors and other space-occupying lesions can compress or invade cranial nerves, leading to palsies. These can be benign or malignant and may arise from the nerves themselves or surrounding tissues.
Types of tumors that can cause cranial nerve palsies:
- Schwannomas
- Meningiomas
- Pituitary adenomas
- Metastatic tumors
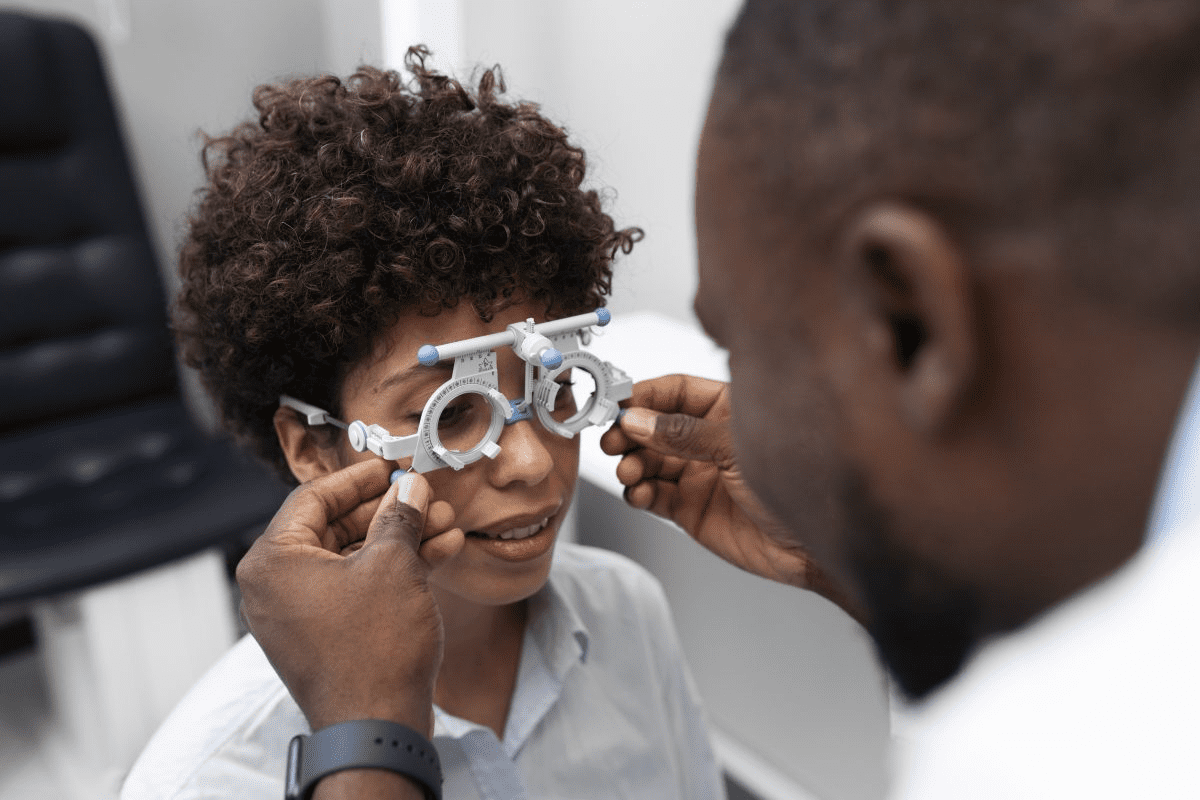
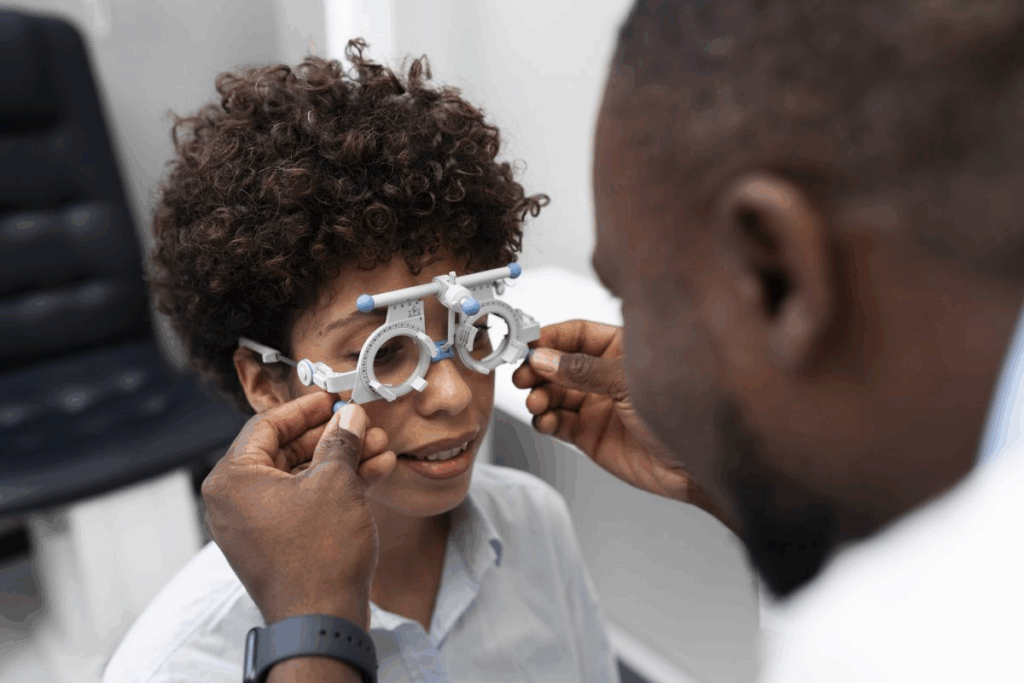
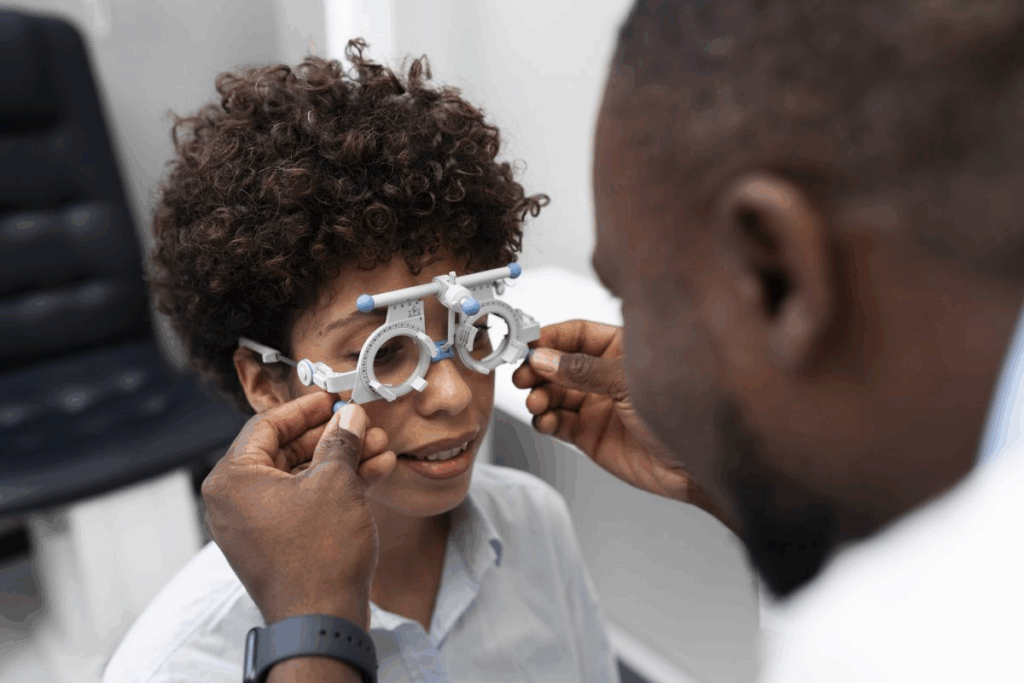
Diagnosing Eye-Related CN Palsies
To find out if cranial nerve palsies are affecting your eyes, doctors use several methods. They look at your eyes, use special scans, and do blood tests. Getting the right diagnosis is key to treating these conditions well.
The Neurological Examination Process
First, doctors do a detailed check-up of your nerves. They check how well you see, how your eyes move, and how your pupils react. They also look at your medical history and do a physical check to find any other health issues.
This check-up includes tests to see how your nerves are working. For example:
- They check how your eyes move and line up.
- They look at your pupils to see if they react right.
- They check how your eyelids move and sit.
- They test your vision.
Advanced Imaging: MRI, CT, and Angiography
Special scans are very important in finding out what’s wrong with your nerves. MRI, CT, and angiography scans help doctors see the nerves and the area around them.
Imaging Modality | Advantages | Disadvantages |
MRI | Shows soft tissues clearly, no radiation | Not good for people with metal implants, can make you feel claustrophobic |
CT | Fast and easy to get, shows bone problems well | Uses radiation, not as good for soft tissues |
Angiography | Shows blood vessels well, great for blood problems | Needs to go inside, uses contrast, can have risks |
Laboratory Tests and Biomarkers
Lab tests help find out what might be causing your nerve problem. Doctors check your blood for things like sugar levels, electrolytes, and inflammation markers. This helps them figure out if you have diabetes, high blood pressure, or other issues.
Differential Diagnosis: Ruling Out Other Conditions
Doctors also have to think about other conditions that might look like a nerve problem. They look at things like myasthenia gravis, thyroid eye disease, or tumors. A thorough check helps them rule out these other conditions and find the right diagnosis.
By using the results from the check-ups, scans, lab tests, and ruling out other conditions, doctors can accurately diagnose and treat eye-related nerve problems. This helps patients get better faster.
Treatment Approaches for Ocular Cranial Nerve Palsies
Ocular cranial nerve palsies need a treatment plan that fits each person’s needs. These conditions are complex. They require a detailed approach that looks at the cause, manages symptoms, and tries different treatments.
Addressing the Underlying Cause
The first step is to find and fix the cause. This might mean managing diabetes or high blood pressure. It could also mean treating infections or injuries.
For vascular causes, controlling blood sugar or blood pressure helps. For trauma, proper care and rehab are key.
Non-Surgical Management Options
Non-surgical treatments are often the first choice. This includes:
- Watching and waiting to see if it gets better
- Prism lenses or other optical aids for double vision
- Eye patches or occlusion therapy to help symptoms
- Botox injections to weaken muscles and fix eye alignment
- Physical therapy to improve eye movement and coordination
These methods can help manage symptoms and improve life quality for patients.
Surgical Interventions: When and Why
Surgery might be needed if other treatments don’t work. It’s considered if the cause needs surgical fixing. Surgery can include:
- Eye muscle surgery to align the eyes
- Decompression surgery for thyroid eye disease
- Tumor removal or debulking
Choosing surgery is a careful decision made with a team of healthcare experts.
Emerging Treatments and Research
New treatments for ocular cranial nerve palsies are being researched. These might include new medicines, advanced surgery, and new rehab methods.
“The future of ocular cranial nerve palsy treatment lies in our ability to develop personalized, evidence-based therapies that address the unique needs of each patient.”
Expert Opinion
Keeping up with new research is important for the best care for patients with ocular cranial nerve palsies.
Living with Cranial Nerve Palsies: Coping Strategies
Living with cranial nerve palsies means understanding the condition and its effects. It’s about adapting to visual changes and finding ways to cope. Psychological support and assistive devices can help a lot.
Adapting to Visual Changes
Visual changes from cranial nerve palsies can affect daily life a lot. Adapting to these changes is key to staying independent and happy. Using prismatic lenses and finding new ways to do things can help.
For example, third nerve palsy can cause a droopy eyelid and double vision. An eye patch can help with double vision. Prismatic glasses can also help align images.
Psychological Impact and Support
The mental side of living with cranial nerve palsies is important. People often feel anxious, depressed, and frustrated. Getting psychological support is a big part of coping.
“The emotional toll of cranial nerve palsy can be as challenging as the physical symptoms. Support from family, friends, and mental health professionals is vital.”
Medical Expert, Neurologist
Assistive Devices and Technologies
There are many tools that can make life better for those with cranial nerve palsies. These include:
- Specialized glasses and lenses
- Eye tracking technology
- Adaptive software for computers and mobile devices
- Low vision aids
Assistive Device | Function | Benefit |
Prismatic Glasses | Aligns images to reduce double vision | Improves visual comfort and reduces eye strain |
Eye Tracking Technology | Allows control of digital devices with eye movements | Enhances independence in using technology |
When to Seek Emergency Care
It’s important to know when to get emergency help. Sudden vision changes, severe pain, or stroke symptoms need quick action.
By understanding the condition, using assistive devices, and getting support, people with cranial nerve palsies can live fulfilling lives.
Conclusion: Navigating Life with Cranial Nerve Palsies
Cranial nerve palsies can really change a person’s life. They affect how we see and move our eyes. We’ve looked into what causes these problems, their signs, how doctors find them, and how to treat them.
Living with cranial nerve palsies needs a lot of care and support. Doctors can help by understanding the cause and treating it right. A team effort, including doctors, surgeons, and therapists, can make a big difference.
With the right care, people can take back control of their lives. They can see better and feel better overall. If symptoms don’t go away or get worse, it’s important to see a doctor. This way, they can get the best help possible.
FAQ
What is cranial nerve palsy?
Cranial nerve palsy is when one or more of the 12 cranial nerves don’t work right. This can mess with things like eye movement and vision.
What are the symptoms of cranial nerve palsy affecting the eyes?
You might see double, have eyelids that droop, or have trouble moving your eyes. You could also have eyes that don’t line up right.
What causes cranial nerve palsies?
Many things can cause it, like diabetes, high blood pressure, or injuries. Infections, tumors, and other growths can also play a part.
How are cranial nerve palsies diagnosed?
Doctors use a neurological exam and scans like MRI or CT to find out. They also do lab tests and compare symptoms to other conditions.
What are the treatment options for ocular cranial nerve palsies?
Treatment depends on the cause. It can include non-surgical ways, surgery, and new treatments.
Can cranial nerve palsies be cured?
It depends on the cause and how much damage there is. Some might get better on their own, but others need ongoing care.
How can patients cope with the visual changes caused by cranial nerve palsies?
Patients can use special devices and tech to help. They should also get support for the emotional side of their condition.
What are the risk factors for developing cranial nerve palsies?
Risks include things like diabetes, injuries, infections, and tumors.
Are there any specific cranial nerves more commonly affected than others?
Yes, the third, fourth, and sixth cranial nerves are often hit. They help control how our eyes move.
When should someone seek emergency care for cranial nerve palsy symptoms?
Get help right away if you have sudden vision problems, a bad headache, or trouble moving your eyes.
What is the prevalence of cranial nerve palsies?
It varies by nerve and cause. For example, trochlear nerve palsy happens about 5.73 times per 100,000 people, and abducens nerve palsy about 4.66 times per 100,000.
References
National Center for Biotechnology Information. Cranial Nerve Disorders: Symptoms, Causes, and Treatment. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6462363/)