It’s important to know the difference between diagnostic colonoscopy and screening colonoscopies. They both use the same tools and methods to look at your colon. But, they have different reasons and how insurance covers them.Is a colonoscopy surgery? This ultimate guide explains the procedure, polyp removal (polypectomy), and what to expect.
We’ll look into how diagnostic and screening colonoscopies help find and stop colorectal cancer. Screening colonoscopies are for people without symptoms who are 45 and older. They check for problems before they start.
A diagnostic colonoscopy is for when you have symptoms. It looks at your colon to find out what’s causing the symptoms.
Key Takeaways
- Diagnostic and screening colonoscopies serve different purposes.
- Screening colonoscopies are for asymptomatic individuals aged 45 and older.
- Diagnostic colonoscopies are used when symptoms are present.
- Both procedures use the same equipment and techniques.
- Insurance coverage differs between diagnostic and screening colonoscopies.
The Importance of Colorectal Cancer Screening
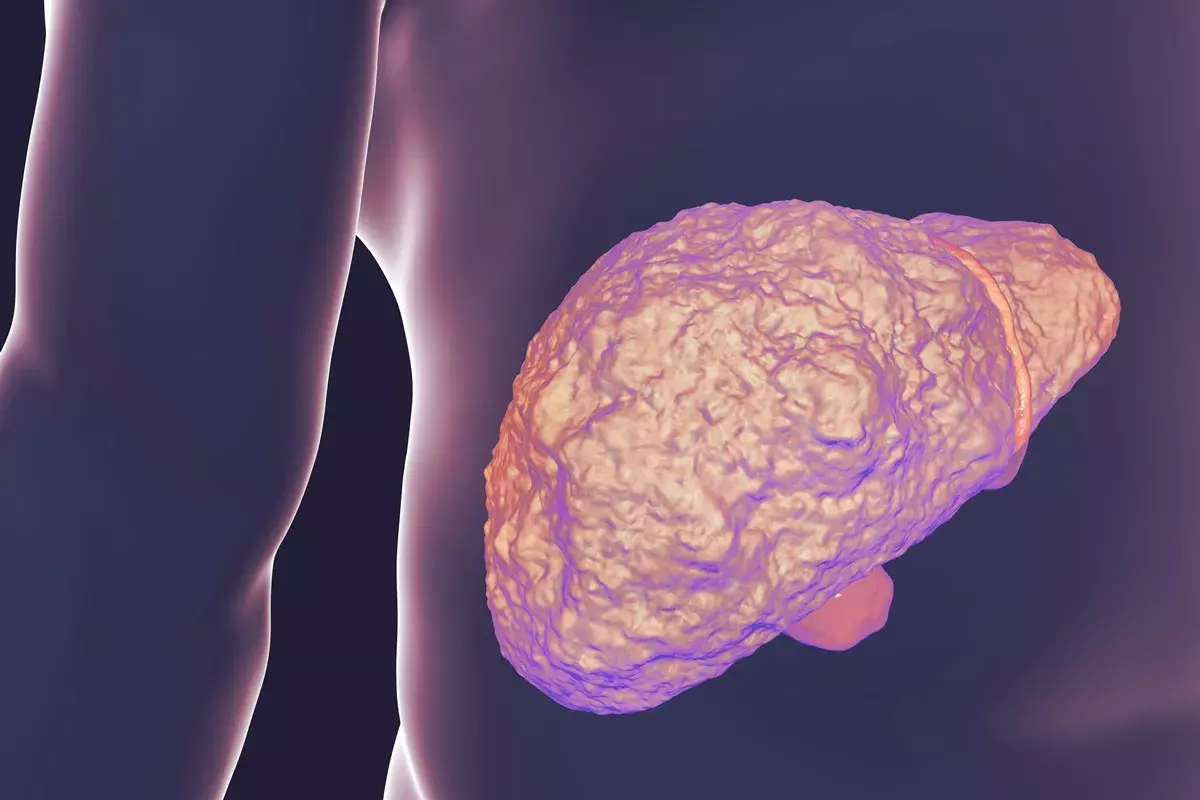
Colorectal cancer screening is vital for preventing and catching this disease early. It’s one of the most common and deadly cancers. So, screening is a key part of healthcare.
The American Cancer Society says colorectal cancer is a big health issue in the U.S. Regular screening is key to preventing and detecting this disease early.
Colorectal Cancer Statistics in the United States
Colorectal cancer stats show why screening is so important. The American Cancer Society says it’s the third most common cancer in both men and women in the U.S.
Year | New Cases | Deaths |
2020 | 147,950 | 53,200 |
2021 | 149,500 | 52,980 |
2022 | 151,030 | 52,550 |
These numbers show we need to keep raising awareness and screening efforts.
Risk Factors and Prevention
Knowing the risk factors is key to preventing colorectal cancer. People with a family history, certain genetic syndromes, or inflammatory bowel disease are at higher risk.
Prevention is possible through regular screening. Screening colonoscopies can find and remove polyps before they turn into cancer.
The American Cancer Society says people with average risk should get a screening colonoscopy every ten years. Those at higher risk might need to start screening sooner and have more frequent tests.
By understanding the importance of colorectal cancer screening and following the guidelines, people can lower their risk of getting this cancer.
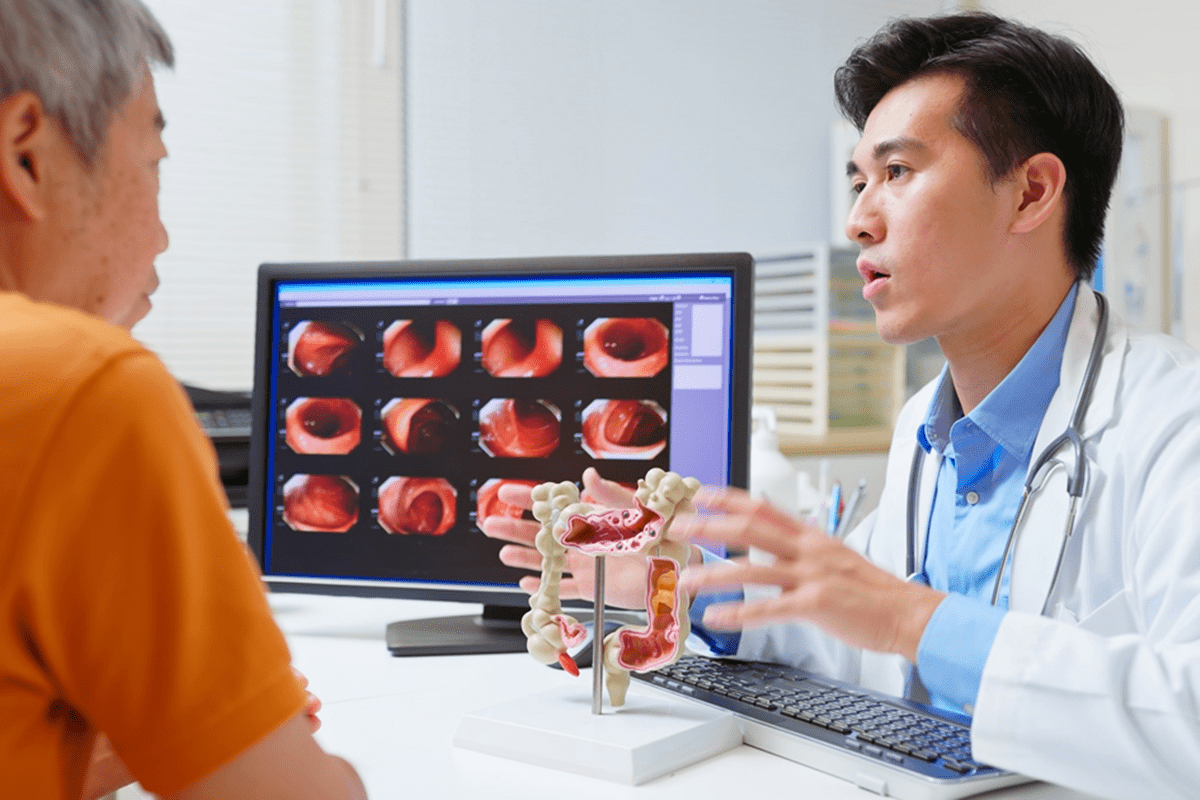
Understanding Colonoscopy Procedures
Colonoscopy procedures are key for checking the colon and rectum. Doctors use them to find and treat problems. Let’s look at why colonoscopies are important in healthcare.
The Purpose of Colonoscopies
A colonoscopy is done when a patient shows symptoms or has health concerns. It helps find issues like polyps, ulcers, or cancer in the colon.
These procedures can also help by removing polyps or taking biopsies. This makes colonoscopies great for both finding and treating problems in the gut.
Basic Procedure Overview
A colonoscopy uses a long, flexible tube with a camera to see inside the colon and rectum. First, the patient is sedated for comfort. Then, the tube is inserted through the rectum, and air is added to make the colon easier to see.
As the tube is pulled out, the doctor looks for any problems. The whole process usually takes 30 to 60 minutes.
Aspect | Description |
Purpose | Diagnostic and therapeutic |
Procedure Time | 30 to 60 minutes |
Preparation | Bowel cleansing and dietary restrictions |
Sedation | Typically used for patient comfort |
Screening Colonoscopy: Definition and Purpose
Screening colonoscopies play a key role in keeping our colon health in check. These tests are for people who don’t show any symptoms and are 45 or older. They help find colon cancer early, often before symptoms show up.
Who Should Get Screening Colonoscopies
People with a low risk of colon cancer should start screenings at 45. Early screening is key to catch and prevent colon cancer. The American Cancer Society says those with a family history of colon cancer or other risk factors might need to start sooner.
- Individuals aged 45 and older
- Those with a family history of colon cancer
- People with a history of colon polyps or other colorectal conditions
Recommended Screening Intervals
The American Cancer Society advises screenings every ten years for those at average risk. If you’re at higher risk, you might need to go more often.
“Regular screenings can significantly reduce the risk of colon cancer by detecting and removing precancerous polyps.”
Benefits of Early Detection
Screening colonoscopies can greatly improve treatment chances for colon cancer. Finding cancer early means better treatment and survival rates.
- Improved treatment outcomes
- Increased chances of survival
- Potential prevention of colon cancer through polyp removal
We stress the importance of following screening guidelines. This maximizes the benefits of early detection.
Diagnostic Colonoscopy: When and Why It’s Performed
When symptoms suggest colorectal issues, a diagnostic colonoscopy is often used. It’s different from screening colonoscopies, which are preventive. Diagnostic colonoscopies investigate specific symptoms or concerns.
Common Symptoms Leading to Diagnostic Procedures
Certain symptoms may lead to a doctor recommending a diagnostic colonoscopy. These include:
- Abdominal pain that persists or is severe
- Changes in bowel habits, such as diarrhea or constipation that last for more than a few days
- Rectal bleeding or blood in the stool
- Unexplained weight loss
These symptoms don’t always mean you have a serious condition. But, they do need further investigation to rule out any issues.
Conditions That May Require Diagnostic Evaluation
Several conditions may need a diagnostic colonoscopy. These include:
- Suspected colon cancer or polyps
- Inflammatory bowel disease (IBD), such as Crohn’s disease or ulcerative colitis
- Diverticulitis or other diverticular diseases
A diagnostic colonoscopy lets doctors visually check the colon and rectum. They can spot any abnormalities.
Diagnostic Follow-Up After Abnormal Tests
If tests like a CT scan or stool test show abnormal results, a diagnostic colonoscopy might be suggested. It’s a detailed look at the colon. This helps in making a clear diagnosis.
Getting a diagnostic procedure can be worrying. But, a diagnostic colonoscopy is key in finding and managing colorectal conditions. Knowing why and when it’s done helps patients prepare and understand the possible results.
Key Differences Between Screening and Diagnostic Colonoscopies
Screening and diagnostic colonoscopies have different goals and impacts on patient care and billing. They both look at the colon but serve different purposes. This affects how patients feel and how doctors code the procedures.
Medical Necessity vs. Preventive Care
Screening colonoscopies aim to find cancer or polyps before symptoms appear. They are for people without symptoms. Diagnostic colonoscopies, on the other hand, are for those with symptoms or signs of a problem. They are needed to diagnose a condition.
Key differences in medical necessity include:
- Screening colonoscopies are for people without symptoms as a preventive step.
- Diagnostic colonoscopies are for those with symptoms or abnormal test results.
Patient Experience Differences
The experience of patients can differ between these two types of colonoscopies. This is mainly because of the reasons they have the procedure.
Patient experience differences:
- Patients getting a screening colonoscopy are usually without symptoms and do it as a precaution.
- Those getting a diagnostic colonoscopy have symptoms like bleeding, changes in bowel habits, or pain. This can change how they see the procedure.
Documentation and Medical Coding Distinctions
The way doctors document and code these procedures is different. This shows their unique purposes and needs.
Coding distinctions include:
- Screening colonoscopies use specific codes that show they are for prevention.
- Diagnostic colonoscopies get codes based on the reason for the procedure and any treatments done.
Knowing these differences helps doctors with billing and patients know what to expect.
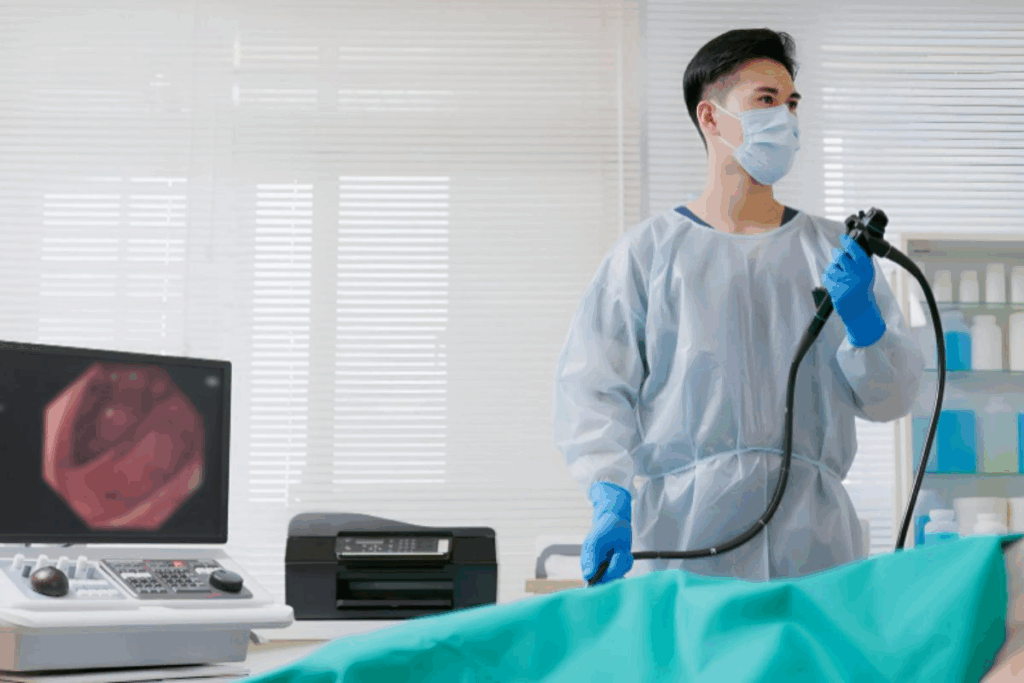
The Colonoscopy Surgery Process and Procedure
The colonoscopy procedure has several steps, from getting ready to the actual check-up. Knowing these steps can help reduce anxiety and make the experience better for patients.
Pre-Procedure Preparation
Before a colonoscopy, patients usually eat only clear liquids for a day or two. This diet helps clean the colon, making it easier for doctors to see inside.
Bowel preparation is key, using a special solution to clear the colon. This can be a liquid or a tablet, depending on the doctor’s order.
Sedation Options
Sedation is important for comfort during the colonoscopy. There are different sedation options, from light to deep sedation, based on the patient’s health and wishes.
The doctor and patient decide on sedation together. This ensures the patient feels comfortable during the procedure.
The Examination Process
A flexible tube with a camera and light is inserted into the rectum during the colonoscopy. This lets the doctor see the colon’s lining. The steps include:
- Insertion of the colonoscope
- Inflation of the colon with air
- Visual examination of the colon’s lining
- Removal of polyps or collection of biopsy samples if necessary
Polyp Removal and Biopsy Techniques
If polyps are found, they can be removed. This is called polypectomy and helps prevent cancer.
Biopsy samples might be taken for further testing. This helps diagnose conditions like inflammation or cancer.
The whole procedure usually takes 30 to 60 minutes, depending on the details of the examination.
Procedure Step | Description | Duration |
Pre-procedure preparation | Dietary restrictions and bowel cleansing | 1-2 days |
Sedation administration | Moderate to deep sedation | During procedure |
Colonoscopy examination | Visual inspection of the colon | 30-60 minutes |
Polyp removal or biopsy | Removal of polyps or taking biopsy samples | Variable |
Recovery and Post-Colonoscopy Care
Recovery and post-colonoscopy care are key parts of the colonoscopy experience. After the procedure, patients need to rest and follow instructions for a smooth recovery.
Immediate Recovery Period
The recovery starts right after the procedure. Patients are watched for a short time to check for any bad reactions to the sedation or the procedure. They might feel sleepy or confused because of the sedation.
It’s important to have someone with you to drive you home. You might not be able to drive yourself.
Managing Post-Procedure Discomfort
Patients might feel some discomfort, bloating, or gas after a colonoscopy. These symptoms are usually short-lived and can be managed with over-the-counter meds or special diets.
When to Contact Your Doctor
Most patients recover well without issues, but some symptoms need immediate medical help. These include severe abdominal pain, heavy bleeding, or fever.
- Severe abdominal pain that persists or gets worse
- Heavy bleeding or rectal bleeding that doesn’t stop
- Fever or chills
- Vomiting or trouble keeping fluids down
If you have any of these symptoms, contact your doctor right away.
Insurance Coverage and Cost Considerations
Insurance for colonoscopies can be tricky, depending on the reason for the test. The Affordable Care Act has helped a lot with this. It makes sure many preventive tests, like colonoscopies, are covered without extra costs.
How Insurance Handles Screening Colonoscopies
The Affordable Care Act says insurance must cover screening colonoscopies without extra costs for some plans. This helps people get the care they need without worrying about money.
Most plans cover these tests for people over 50 or those with a family history of colon cancer. But, the details can change based on the insurance and the patient’s plan.
Coverage for Diagnostic Procedures
Diagnostic colonoscopies are for when you have symptoms or a screening test shows something odd. These tests usually have different rules for insurance, which might include extra costs.
It’s key to know that while many plans cover these tests, how much they cover can differ. Some might need you to get approval first or have certain rules.
When a Screening Colonoscopy Becomes Diagnostic
At times, a screening test might turn into a diagnostic one if something unusual is found. This can change how your insurance covers it.
Knowing this can help you understand any extra costs you might face. It’s smart to talk about this with your doctor and insurance before the test.
Getting the hang of how insurance works for colonoscopies can make things easier. Knowing what’s covered and why helps you make better choices about your health.
Risks and Complications of Colonoscopy Procedures
Colonoscopy procedures are generally safe but can have risks and complications. It’s important to know about these to make informed choices.
Common Side Effects
Most people have mild and short-term side effects after a colonoscopy. These include:
- Bloating and gas
- Abdominal discomfort or cramps
- A feeling of fullness or pressure in the abdomen
- Nausea or vomiting (rarely)
These side effects usually go away within a few hours to days.
Serious Complications
Though rare, serious complications can happen. These include:
- Bleeding: This can happen if a polyp is removed or a biopsy is taken. Most of the time, it’s controlled during the procedure. But sometimes, it needs extra treatment.
- Perforation: A tear or hole in the colon wall is rare but serious. It might need surgery to fix.
- Infection: Though rare, infection can happen, mainly if bacteria are introduced during the procedure.
- Reaction to sedation: Some people may have a bad reaction to the sedation used during the procedure.
Risk Factors to Discuss With Your Doctor
Some factors can increase the risk of complications. It’s key to talk about these with your doctor:
- Age and overall health
- Previous abdominal surgery or colon conditions
- Use of certain medications, such as blood thinners
- Presence of conditions like diverticulitis or inflammatory bowel disease
Talking about these risk factors with your doctor helps you understand the risks and benefits of a colonoscopy.
Following your doctor’s instructions before, during, and after the procedure is vital. If you have severe symptoms like heavy bleeding, severe abdominal pain, or fever after a colonoscopy, get medical help right away.
Alternatives to Traditional Colonoscopy
For those who don’t like traditional colonoscopy, there are other options. These alternatives are good for people at average risk or who worry about the procedure’s invasiveness. They also help with the prep work needed for a traditional colonoscopy.
Stool-Based Tests
Stool-based tests are easy and don’t hurt. They find hidden blood or DNA changes in your stool. These signs can mean colorectal cancer or polyps. You do these tests at home and send them to your doctor.
- Fecal Occult Blood Tests (FOBT): Detect hidden blood in the stool.
- Fecal Immunochemical Tests (FIT): Find human hemoglobin in the stool.
- Stool DNA Tests: Look for DNA changes and blood in the stool.
Virtual Colonoscopy
Virtual colonoscopy, or CT colonography, uses X-rays and computer software. It shows detailed images of your colon. It needs bowel prep like traditional colonoscopy but is less invasive and doesn’t need sedation.
Flexible Sigmoidoscopy
Flexible sigmoidoscopy uses a tube with a camera in the rectum. It looks at the sigmoid colon and rectum. It’s not as thorough as a full colonoscopy but can find polyps and cancer in the lower colon.
When Alternatives May Be Appropriate
These alternatives are good for those at average risk who can’t or won’t have a traditional colonoscopy. But, if these tests find polyps or abnormalities, a follow-up colonoscopy is usually needed.
Preparing for Your Colonoscopy: Tips and Guidelines
Getting ready for a colonoscopy is a detailed process. It helps make sure the colonoscopy diagnosis goes well. We know it can seem scary, but with the right help, you can get through it easily.
Dietary Restrictions
Following the diet rules is a big part of getting ready. You’ll need to stick to a clear liquid diet the day before. This means:
- Clear broths
- Plain gelatin
- Water
- Clear juices (like apple or white grape)
- Black coffee or tea (without milk or cream)
It’s important to avoid solid foods and some liquids. This helps clean your bowel well for the test.
Bowel Preparation Process
The bowel prep is a key part of getting ready. You’ll take a bowel-cleansing solution to empty your colon. This solution makes sure there’s no stool left, so the doctor can see everything clearly.
“Adequate bowel preparation is key to a successful colonoscopy, as it directly impacts the accuracy of the diagnosis.”
— Gastroenterology Guidelines
Make sure to follow your doctor’s advice on when and how much of the solution to take.
Medications to Avoid
Some medicines might need to be stopped before your colonoscopy. Tell your doctor about all the medicines you’re taking, like:
- Blood thinners
- Diabetes medications
- Certain supplements
Your doctor will tell you which medicines to skip and for how long.
What to Bring to Your Appointment
On the day of your colonoscopy, don’t forget to bring:
- A responsible adult to drive you home
- Your insurance cards and identification
- A list of your current medications
- Any relevant medical records or test results
Being ready will help your colonoscopy go smoothly and quickly.
Conclusion
Colonoscopy procedures are key in stopping and finding colorectal cancer early. We’ve talked about the big differences between diagnostic and screening colonoscopies. Each has its own role in keeping our colon health in check.
It’s important for patients to know the difference between a diagnostic and a screening colonoscopy. A diagnostic colonoscopy is done when you have symptoms or after an abnormal screening. It tries to find out what’s causing your symptoms or look into any odd findings.
On the other hand, screening colonoscopies are for people without symptoms. They aim to catch polyps or cancer early. Knowing the difference between these two types is more than just words. It affects how you prepare, what insurance covers, and how the procedure is done.
Understanding these differences helps patients make better choices about their health care. We suggest talking to your doctor about your specific needs and risks. This way, you can choose the right screening or diagnostic plan for you.
FAQ
What is the difference between a diagnostic colonoscopy and a screening colonoscopy?
A diagnostic colonoscopy looks for symptoms or abnormalities. A screening colonoscopy is for those without symptoms to find cancer or polyps early.
What are the symptoms that may require a diagnostic colonoscopy?
Symptoms like rectal bleeding, changes in bowel habits, or abdominal pain may need a diagnostic colonoscopy. This is to find the cause.
Who should undergo a screening colonoscopy?
Adults 45 and older, or those with a family history of colorectal cancer, should get regular screening colonoscopies. This is a preventive measure.
How often should I have a screening colonoscopy?
Screening colonoscopies are usually every 10 years for those with no symptoms or risk factors. But, this can change based on your or your family’s health history.
What is the purpose of bowel preparation before a colonoscopy?
Bowel preparation cleans the colon. This lets doctors see the colon’s lining clearly during the procedure.
Are there alternatives to traditional colonoscopy?
Yes, alternatives include stool-based tests, virtual colonoscopy, and flexible sigmoidoscopy. Each has its own benefits and drawbacks.
What are the risks and complications associated with colonoscopy?
Colonoscopy is generally safe but can have risks like bleeding or perforation. Adverse reactions to sedation are also possible, though serious problems are rare.
How is a colonoscopy performed?
A colonoscopy involves a flexible tube with a camera inserted into the rectum. It examines the colon’s lining, often under sedation for comfort.
What should I expect during recovery from a colonoscopy?
After, you might feel mild discomfort, bloating, or gas. These usually go away in a few hours. It’s best to have someone with you when you go home.
Will my insurance cover the cost of a colonoscopy?
Many insurance plans cover screening colonoscopies as preventive care. But, coverage for diagnostic colonoscopies can vary based on your insurance and the reason for the procedure.
What is the difference in medical coding between screening and diagnostic colonoscopies?
Screening and diagnostic colonoscopies are coded differently. This reflects their different purposes and medical needs.
Can I continue my medications before a colonoscopy?
It’s important to talk to your doctor about your medications before a colonoscopy. Some may need to be paused or adjusted.
What dietary restrictions should I follow before a colonoscopy?
Usually, you’ll be on a clear liquid diet the day before. Some foods and drinks may be restricted to help with bowel preparation.
What are the benefits of early detection through screening colonoscopy?
Early detection through screening colonoscopy can greatly improve treatment outcomes. It finds colorectal cancer or polyps early, when they’re easier to treat.
When does a screening colonoscopy become diagnostic?
If a polyp is found and removed during a screening colonoscopy, or if an abnormality is investigated, it may be considered diagnostic. This is for billing and medical records.
References:
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6329457/