Last Updated on October 21, 2025 by mcelik
What is the common cause thrombocytopenia children? Learn the crucial primary reasons for low platelets in kids. Powerful knowledge for parents and pediatricians.
Thrombocytopenia is when kids have too few platelets, leading to easy bruising and bleeding. It’s when a child’s platelet count drops below 150,000/microL. Doctors might suspect it if a child bruises easily or bleeds a lot.

The big worry with thrombocytopenia is how it affects a child’s health. Immune thrombocytopenic purpura (ITP) is the top reason for it in kids. ITP happens when the immune system mistakenly attacks and destroys platelets.
Knowing why thrombocytopenia happens, like with ITP, is key to helping kids get better. We’ll look into the signs, how doctors figure it out, and how to treat it and other causes.
It’s important to understand thrombocytopenia in kids. This condition means there are not enough platelets in the blood. It can cause serious health problems in children.
Thrombocytopenia happens when platelet counts are too low. In kids, a normal count is between 150,000 to 450,000 platelets per microliter of blood. Platelets help blood clot, and not enough can lead to bleeding.
A low platelet count can be due to several reasons. It’s important to know why it’s happening to treat it right. Thrombocytopenia can cause bleeding, from small bruises to serious hemorrhages.
There are many reasons why thrombocytopenia happens. Some include:
Thrombocytopenia can be caused by many things. Studies show that how common it is in kids depends on the cause.
Important things to know about thrombocytopenia in kids include:
Immune thrombocytopenic purpura (ITP) is one of the leading causes of thrombopenia in children, and its top reason for low platelet counts in kids. We’ll dive into what ITP is, how common it is, and who it usually affects.
ITP happens when the immune system attacks platelets. This makes the platelet count drop, raising the chance of bleeding. The pathophysiology of ITP is complex, involving immune cells and platelets.
Platelets are mainly destroyed in the spleen. This is because the immune system marks them for removal. Knowing this helps doctors find better ways to treat ITP.
ITP is found in about 3“8 kids per 100,000 each year. It can hit kids of all ages, but most often between 2 and 5 years old.
Boys and girls get ITP about the same, but some studies say boys might get it more often in younger years. Viral infections can sometimes trigger ITP in kids.
ITP can be either acute or chronic in kids. Acute ITP starts suddenly and usually goes away in 3 to 6 months. Chronic ITP lasts more than 12 months and needs ongoing care.
It’s important to know if a child has acute or chronic ITP. Most kids have the acute form, which often gets better on its own.
It’s key to know how pediatric ITP presents to manage it well. Kids with ITP show symptoms that can be mild or severe.
Kids with ITP often bruise easily and have petechiae. They might also bleed from their gums or nose. This happens because they don’t have enough platelets to form blood clots.
Easy bruising is a common first sign. Petechiae show up on the skin, often on the legs.
ITP’s severity depends on the platelet count and bleeding. Mild ITP has few symptoms, while severe ITP causes a lot of bleeding.
Parents and caregivers should know when to get medical help. If a child has severe bleeding, bleeding in the mouth, blood in urine or stool, OA, or a severe headache, get help right away.
“Prompt recognition of the symptoms of ITP and understanding when to seek medical help can significantly impact the outcome for children with this condition.”
Knowing the symptoms and how ITP presents helps parents and doctors give the best care to kids with this condition.
Infections are a big reason for thrombocytopenia in kids. It’s important to know how they affect platelets. This helps us treat them better.
Viral infections often lead to low platelet counts in children. Viruses like Epstein-Barr and HIV can harm platelet production. We’ll look at how these viruses affect platelets and what it means for kids.
Viruses can stop bone marrow from making platelets, destroy platelets, or trap them in the spleen. Knowing this helps us find better ways to treat kids.
Dengue fever is a big reason for low platelets in kids, mainly in areas where it’s common. Up to 51% of kids in some places get dengue. We’ll explore how dengue affects platelets and what symptoms to watch for.
Dengue virus lowers platelet count by affecting bone marrow and causing the immune system to attack platelets. Spotting dengue symptoms early is key to treating them right.
Malaria is another major cause of low platelets in kids, mostly in tropical areas. It brings fever, anemia, and low platelets. We’ll talk about how malaria affects platelets and what it means for kids.
Other diseases like leishmaniasis and tick-borne illnesses can also lower platelet counts in kids. Knowing all the causes helps us find the best ways to diagnose and treat.
Thrombocytopenia in kids can come from many sources, not just ITP and infections. It can also be caused by some medicines and not getting enough nutrients. Knowing these causes helps doctors find and treat the problem correctly.
Some medicines can make kids’ platelet counts drop. Drug-induced thrombocytopenia happens when a drug makes the body attack its own platelets. This can be caused by antibiotics, medicines for seizures, and some pain relievers.
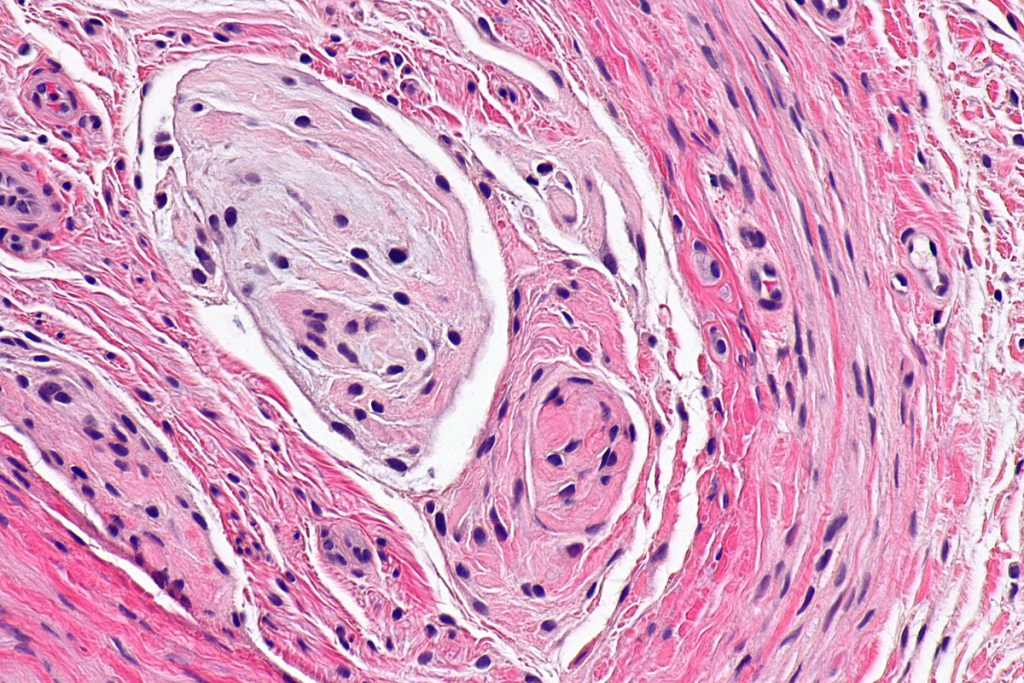
Bone marrow problems can really affect how many platelets are made. Issues like aplastic anemia and leukemia can stop the bone marrow from making enough platelets. Doctors usually do a bone marrow biopsy to see how the marrow is doing.
Not getting enough of certain vitamins can also lower platelet counts. Not having enough B12 or folate can hurt platelet production. It’s important to eat well to keep platelet counts healthy.
By knowing all these causes, doctors can make better plans to help kids with thrombocytopenia.
Diagnosing thrombocytopenia in children is a detailed process. We look at many possible causes and use different tests to find the root problem.
The first step is a complete blood count (CBC) and a blood smear. The CBC shows the platelet count. The blood smear checks for platelet shape and other cell issues.
We also test liver and spleen function. This helps find if these organs are causing the low platelet count.
If the first tests don’t show a cause, we do more tests. Bone marrow tests are key. They check platelet production and look for bone marrow problems.
Other tests look for antibodies against platelets. These are often seen in immune thrombocytopenic purpura (ITP).
When we diagnose thrombocytopenia, we think of many possible causes. This includes infections, autoimmune diseases, and bone marrow issues.
We look at the child’s symptoms, medical history, and lab results. This helps us find the most likely cause.
A bone marrow test is very important in some cases. It checks if the bone marrow can make platelets. It can also find leukemia, aplastic anemia, or other problems.
This test is key when we think of bone marrow issues or when we’re not sure after the first tests.
Managing pediatric thrombocytopenia requires understanding its causes. The right treatment depends on the cause. This can range from immune issues to infections or bone marrow problems.
ITP in kids aims to raise platelet counts to prevent bleeding. First-line treatments include corticosteroids like prednisone. Sometimes, intravenous immunoglobulin (IVIG) is used to quickly increase platelets.
If first-line treatments fail or the condition is chronic, second-line therapies like rituximab or thrombopoietin receptor agonists may be used.
Treating the cause is key to infections or other conditions. For viral infections, antiviral therapy is needed. Stopping the drug that causes drug-induced thrombocytopenia is also essential.
“The key to managing thrombocytopenia lies in accurately diagnosing its cause and tailoring the treatment.”
Expert Opinion
Severe thrombocytopenia with bleeding needs quick action. Platelet transfusions may be given to quickly raise platelet counts. Hospitalization is often needed for close monitoring and care.
In conclusion, treating pediatric thrombocytopenia is highly individualized. It depends on the cause, severity, and the child’s health. A detailed treatment plan, made with healthcare professionals, is key to managing the condition well.
Knowing how thrombocytopenia in children will turn out is key to managing it well. The future for kids with thrombocytopenia, like those with Immune Thrombocytopenic Purpura (ITP), can be different for everyone.
Pediatric ITP is hard to predict. Some kids get better in a few months, while others have it for a long time. About 70-80% of kids with ITP get better on their own within six months.
“The natural history of ITP in children is diverse,” studies say. “Some have a mild illness that goes away, while others have a chronic condition that needs ongoing care.”
Keeping an eye on kids with ITP is important. This means:
Each child’s follow-up plan is different. Kids with very low platelets or bad bleeding need to see their doctor more often.
ITP can affect a child’s life. It can limit their physical activities and affect their mental health. Doctors try to help by making care plans that fit each child’s needs.
New treatments for pediatric ITP have come out. These offer options for kids who don’t get better with the usual treatments. These new treatments have helped many kids with ITP live better lives.
“New therapies have changed how we treat pediatric ITP,” says a top pediatric hematologist. “They give hope for better futures for these kids.”
Understanding what happens with pediatric thrombocytopenia helps doctors give better care. They can tailor their approach to meet each child’s specific needs.
Thrombocytopenia in children is a complex issue with many causes. These include immune thrombocytopenic purpura (ITP), infections, and bone marrow problems. We’ve looked at how these factors lead to low platelet counts in kids, focusing on ITP as the main cause.
Knowing what causes thrombocytopenia is key to finding good treatments. Doctors can help kids more by spotting ITP and other causes early. This way, they can improve the care for children with low platelet counts.
As we learn more about thrombocytopenia in kids, we must think about each child’s needs. This approach helps us give better care and support. It makes a big difference in their lives, improving their overall well-being.
Thrombocytopenia in children is when they have too few platelets. This can cause bruising and bleeding. It can happen for many reasons, like infections or certain medicines.
The most common reason is Immune Thrombocytopenic Purpura (ITP). It’s when the body’s immune system attacks and destroys platelets by mistake.
Kids with ITP might bruise easily, have small spots called petechiae, and bleed. How bad these symptoms are can vary. It’s important to know when to see a doctor to avoid serious problems.
Finding out if a child has thrombocytopenia involves several steps. First, doctors do some tests. Then, they might do more tests or even take a bone marrow sample to find out why.
Treatment for thrombocytopenia depends on why it’s happening. For ITP, doctors might use medicines. They also try to fix the cause, like infections or problems with the bone marrow. Sometimes, they need to act fast to stop serious bleeding.
Knowing how well a child will do with thrombocytopenia is key. Doctors need to understand ITP in kids, how to keep an eye on them, and how it affects their lives. This helps in caring for them better.
Yes, infections can lower platelet counts in kids. Viruses, dengue, and malaria are examples. It’s important to know how infections affect platelets to treat them well.
Low platelet counts can also come from other things. This includes medicines, problems with the bone marrow, and not getting enough nutrients.
ITP is an autoimmune disease. It’s different from other reasons for low platelets, like infections or bone marrow issues. Knowing the cause helps doctors find the right treatment.
Sometimes, doctors need to check the bone marrow to figure out why a child has low platelets. This is important if they’re not sure or if they worry about the bone marrow.
Neunert, C., Stasi, R., & Buchanan, G. R. (2019). Immune thrombocytopenia (ITP): A clinical perspective. Hematology/Oncology Clinics of North America, 33(4), 607“620. https://www.sciencedirect.com/science/article/pii/S0889858819300520
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us