Last Updated on October 31, 2025 by Saadet Demir

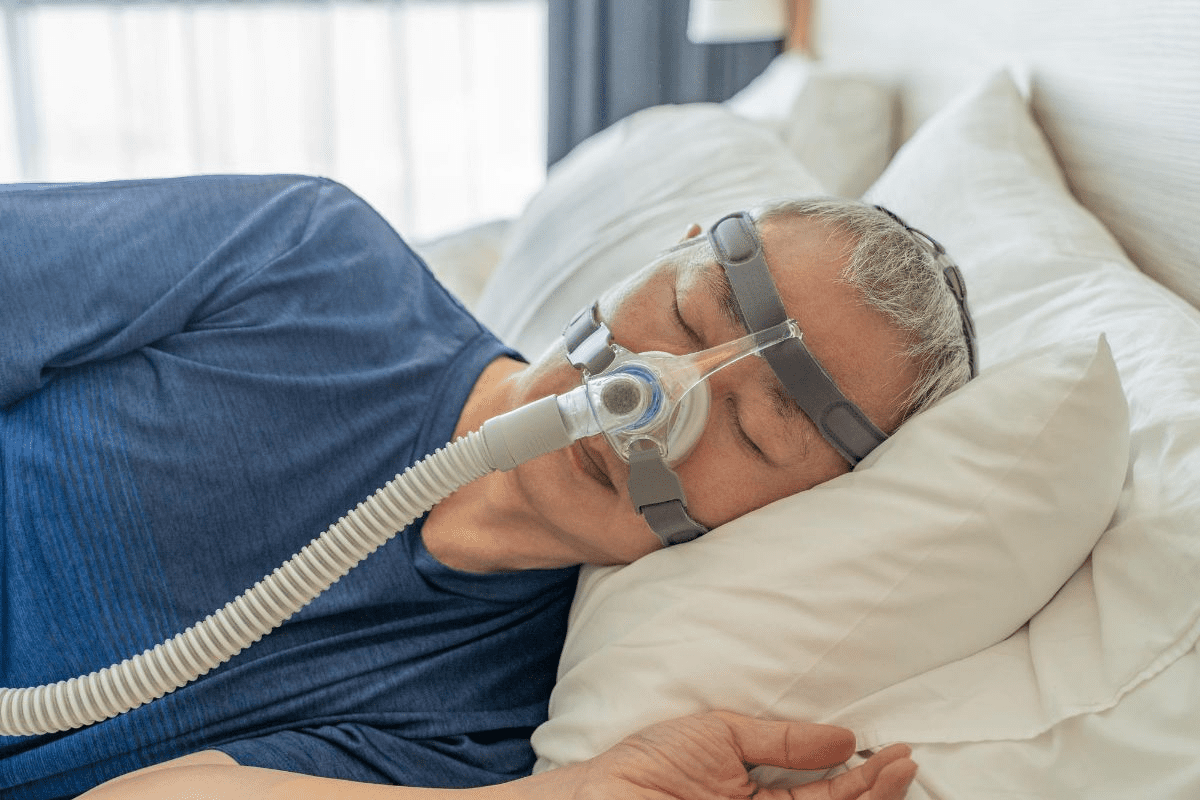
At Liv Hospital, we know how sleep disorders affect health. Continuous Positive Airway Pressure (CPAP) is a treatment that sends pressurized air through a mask. It keeps the airway open while you sleep.
This therapy helps those with obstructive sleep apnea (OSA) a lot. It stops the airway from closing and makes sleep better. Using a CPAP machine can make you feel less tired during the day. It also lowers the chance of heart disease.
We offer detailed sleep disorder checks and care that puts patients first. Our aim is to help you sleep well and feel better overall.
What is cpap therapy and how does it work to treat obstructive sleep apnea by providing continuous positive airway pressure?
It’s important to understand sleep apnea to tackle this widespread sleep disorder. Sleep apnea affects millions, causing serious health issues. We need to diagnose and treat it properly.
Obstructive sleep apnea (OSA) means breathing stops many times during sleep. This happens when the airway partially or fully closes. It leads to broken sleep and low blood oxygen, harming health and life quality.
Sleep apnea symptoms include loud snoring, morning headaches, and feeling very tired during the day. If not treated, it can cause serious health problems. These include heart disease, diabetes, and brain problems. We must spot these signs early to avoid these risks.
Sleep apnea greatly affects a person’s life, impacting sleep and daily activities. It can cause lower productivity, strained relationships, and a lower quality of life if not managed well.
CPAP therapy is key in treating sleep disorders, like obstructive sleep apnea. We’ll look into its definition, history, and main uses. This will help us see why it’s so important in sleep medicine.
CPAP therapy uses a constant flow of air through a mask that covers your nose and/or mouth. This positive airway pressure keeps your airway open while you sleep. It stops breathing pauses that happen in sleep apnea.
The right pressure is set based on a sleep study. This makes sure the therapy fits you perfectly. CPAP improves sleep quality and lowers risks from untreated sleep apnea.
CPAP therapy started in the 1980s by Medical Expert. Over time, it has gotten better with new mask designs and systems for delivering pressure.
These changes have made CPAP easier to use and more comfortable. Now, CPAP is the gold standard for treating sleep apnea. Research keeps going to make it even better.
CPAP is mainly for treating obstructive sleep apnea (OSA). It stops airway blockages during sleep. This reduces symptoms like snoring, tiredness, and brain fog.
CPAP is also used for other sleep breathing problems. It shows how versatile and vital CPAP is in sleep medicine. As we learn more about sleep disorders, CPAP’s role will keep growing.
CPAP therapy works by creating a pneumatic splint to stop airway collapse. It does this by delivering continuous positive airway pressure. This keeps the airway open during sleep.
CPAP machines send pressurized air through a mask. This air creates a positive pressure that keeps the airway open. It prevents collapse during sleep.
A leading sleep specialist says, “The key to effective CPAP therapy is understanding the balance between pressure settings and patient comfort.” This balance is key for treatment success.
“The key to effective CPAP therapy lies in understanding the delicate balance between pressure settings and patient comfort.”
The pneumatic splint concept is key to CPAP’s function. CPAP machines deliver constant pressurized air. This creates a splint that keeps the airway open.
Benefits of Pneumatic Splint | Description |
Prevents Airway Collapse | The pneumatic splint keeps the airway open, preventing collapse during sleep. |
Reduces Sleep Apnea Symptoms | By keeping the airway open, CPAP therapy reduces sleep apnea symptoms. |
Improves Sleep Quality | The pneumatic splint ensures a stable airway, improving sleep quality. |
Pressure settings are vital in CPAP therapy. The pressure must be high enough to prevent collapse but not too high. The ideal setting is found through sleep studies or titration.
Key factors influencing pressure settings include:
Healthcare providers adjust these settings carefully. They ensure patients get effective treatment with minimal side effects.
To understand CPAP therapy, we need to look at its parts. A CPAP system has several key parts that work together. They deliver continuous positive airway pressure therapy.
The pressure generator, or main unit, is the heart of the CPAP machine. It makes the pressurized air that goes to the user’s airway. Inside, a motor creates the pressure, and a control system lets you adjust it based on your needs.
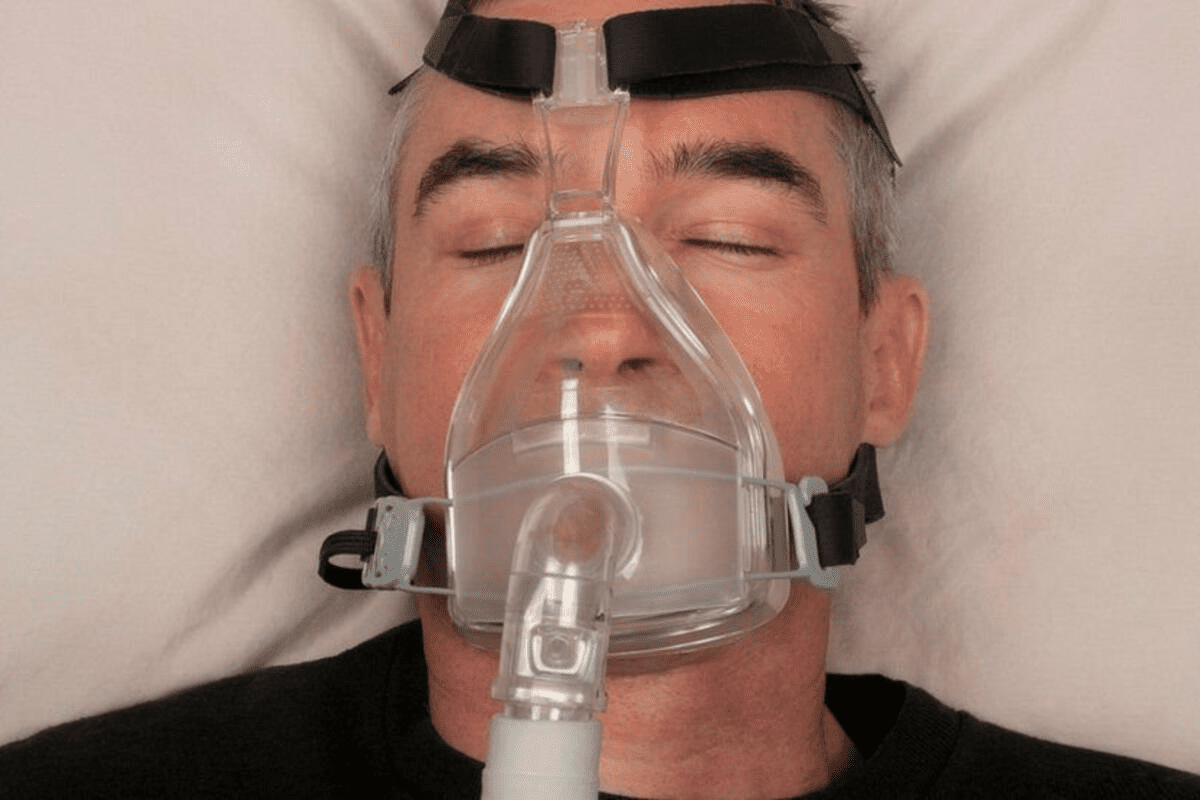
Masks are key in the CPAP system. They connect the pressurized air to the user’s airway. There are many types, like nasal masks, full-face masks, and nasal pillow masks. Each is designed for different users, affecting comfort and therapy success.
The delivery tubing links the mask to the pressure generator. It lets the air flow from one to the other. The tubing is flexible and strong, fitting comfortably without restricting movement. Connectors keep the tubing in place, ensuring no leaks.
Humidifiers add moisture to the air, making it more comfortable. They help prevent dryness in the nose and throat. Comfort accessories, like mask liners and tubing covers, also enhance the CPAP experience. They can reduce noise and improve comfort, making therapy more effective.
Knowing about CPAP system components helps users understand how they work together. It’s important to talk to a healthcare professional to find the right CPAP setup for you.
CPAP therapy has grown to include many machine types. Each is made for different needs. This variety lets patients pick the best machine for them, making treatment more effective.
Standard CPAP machines give a steady flow of air all night. They are prescribed for patients needing a constant pressure based on sleep studies. This constant pressure keeps the airway open, stopping apneic events.
APAP machines change the air pressure as needed during sleep. This change ensures the airway stays open, possibly making sleep more comfortable.
BiPAP systems offer two pressures: one for breathing in and a lower one for breathing out. This is great for those who find it hard to exhale with a standard CPAP’s constant pressure.
Portable CPAP machines are made for travel. They are small, light, and work well. These machines are battery-powered and come with travel cases, perfect for patients who need to travel with their therapy.
When picking a CPAP machine, think about:
Today’s CPAP machines offer a tailored approach to treating sleep apnea. Knowing the different types and their features helps patients make better choices for their therapy.
Starting CPAP therapy is a big step. We’ll guide you through the key steps. This includes diagnosis and setup for smooth sleep apnea management.
Your CPAP journey starts with a sleep study. This test checks your sleep patterns and finds sleep apnea disruptions. You might do it at home or in a sleep lab, based on your needs and doctor’s advice.
The study records your brain waves, muscle activity, and heart rate while you sleep. It also watches your breathing. This data shows if you have sleep apnea and how severe it is. It helps decide if you need CPAP therapy.
Type of Sleep Study | Description | Setting |
Home Sleep Apnea Test (HSAT) | A simple test that records airflow, breathing, and oxygen levels. | Home |
Polysomnography (PSG) | A detailed overnight study that records many physiological activities. | Sleep Laboratory |
After the sleep study, a doctor will look at the results and prescribe CPAP if needed. The prescription will tell you the right pressure for your machine. This is key for treating sleep apnea.
With your prescription, you’ll set up your CPAP machine with a supplier. You’ll choose a mask that fits well and any extra features, like a humidifier.
Getting used to CPAP therapy takes time. You might feel uncomfortable or trapped at first. But most people get used to it in a few weeks.
Start with short CPAP sessions and increase them as you get more comfortable. A humidifier can also help by keeping your nose and throat moist. Plus, finding a mask that fits well and is comfy can make a big difference.
CPAP therapy greatly improves sleep quality and overall health. It keeps the airway open during sleep. This tackles the main cause of sleep apnea, bringing many health benefits.
CPAP therapy makes sleep better by cutting down on sleep breaks and boosting deep and REM sleep. This means you wake up feeling more refreshed and alert.
CPAP therapy improves sleep, leading to less daytime tiredness and sleepiness. People using CPAP often feel more awake and ready to tackle the day.
CPAP therapy also boosts brain function and mental health. It can improve focus, memory, and mood. This lowers the chance of depression and anxiety.
CPAP therapy is good for the heart by lowering risks linked to sleep apnea, like high blood pressure and heart disease. This can cut down on the risk of death, helping you live longer.
CPAP therapy is very effective but can be tough to get used to. We know it can feel overwhelming. But, with the right tips, you can beat these challenges and sleep better.
Many CPAP users struggle with mask discomfort. A mask that fits right is key for comfort. Try out different masks like nasal, full-face, or nasal pillow masks to find your best match.
Dry mouth and nasal congestion are common problems. A heated humidifier can help a lot by adding moisture to the air.
CPAP machines can be noisy, which might bother your partner. New CPAP devices are quieter, but there are ways to make it even less disturbing.
Some people feel anxious or claustrophobic with a CPAP mask. Slowly getting used to it and using relaxation methods can help.
To keep CPAP therapy working well, regular upkeep is key. Taking good care of your equipment helps it last longer. It also makes sure it keeps working right.
Cleaning every day is important for keeping things clean and safe. Wash the mask, tubing, and humidifier with mild soap and warm water. Make sure to rinse well and let them dry in the air.
For a deeper clean, do a weekly soak. Use warm water and a CPAP cleaning solution for the mask and parts. Then, rinse and dry them as usual. Use a damp cloth to clean the outside of the CPAP machine.
Key daily cleaning steps include:
Changing filters and parts regularly is important. Filters should be swapped out every 1-3 months. This depends on how often you use it and what the maker says.
Other parts, like the mask and tubing, might need to be replaced every 6-12 months. Always follow what the maker says for the best results.
Some key replacement guidelines include:
Fixing common problems with your CPAP is also part of the upkeep. If you have leaks, issues with the humidifier, or strange noises, fix them fast. Look in the user manual or talk to a healthcare provider for help.
By sticking to these care tips, you can keep your CPAP in top shape. This ensures your therapy works well and helps you sleep better.
Insurance coverage is key for making CPAP therapy available. In the US, Medicare and private insurance both cover CPAP therapy. But, they have different rules and levels of coverage.
Medicare covers CPAP therapy if you have obstructive sleep apnea (OSA) confirmed by a sleep study. Private insurance also covers it, but their rules can vary a lot.
Medicare’s main requirements are:
Private insurers might ask for similar or extra things, like pre-authorization or specific tests.
Even with insurance, patients might have to pay some costs. These can include deductibles, copays, and expenses for supplies and maintenance.
To handle these costs, patients can look into different financing options:
Insurance companies often check if you’re using your CPAP as directed. This might mean regular visits to your doctor and downloading data from your CPAP machine.
“Sticking to your CPAP treatment plan is important. It helps you get the most out of your therapy and keeps your insurance coverage. Not following the plan can cause you to lose coverage or face higher costs.”
Knowing about insurance and costs helps patients deal with the financial side of CPAP therapy. It ensures they get the treatment they need.
CPAP therapy is a top choice for treating obstructive sleep apnea. It offers many health benefits. Knowing how CPAP works and its parts helps users choose the right treatment.
The CPAP device sends a steady flow of air to keep the airway open. This ensures sleep without interruptions. CPAP therapy improves sleep quality, reduces daytime tiredness, and boosts heart health.
In wrapping up our look at CPAP therapy, it’s clear it’s changed how we manage sleep apnea. It greatly improves health and life quality. We urge those with sleep apnea to talk to doctors about starting CPAP therapy.
CPAP therapy helps treat obstructive sleep apnea (OSA). This condition makes the airway block or collapse during sleep. It causes breathing pauses or shallow breaths.
CPAP stands for Continuous Positive Airway Pressure.
A CPAP machine sends a constant flow of air through a mask. This keeps the airway open, preventing it from collapsing during sleep.
A CPAP system includes a pressure generator, mask, tubing, and humidifier. Together, they deliver pressurized air to the user.
There are many CPAP machines. These include standard CPAP devices, auto-adjusting CPAP (APAP) machines, BiPAP systems, and portable machines for travel.
The pressure setting is found through a sleep study or titration process. This identifies the best pressure to keep the airway open.
CPAP therapy improves sleep quality and reduces daytime sleepiness. It also enhances cardiovascular health.
Adapting to CPAP therapy means starting slowly and using a humidifier. Finding a comfortable mask fit is also important.
Challenges include mask discomfort, dry mouth, and nasal congestion. These can be solved with proper mask fitting, humidifier use, and relaxation techniques.
Keep your CPAP equipment clean daily and weekly. Replace filters and parts as needed. Troubleshoot any problems that arise.
Yes, CPAP therapy is covered by Medicare and private insurance in the US. Coverage levels and requirements vary.
CPAP in medical terms means delivering continuous positive airway pressure. It keeps the airway open during sleep, treating obstructive sleep apnea.
A humidifier adds moisture to the air from the CPAP machine. This makes breathing more comfortable and reduces dry mouth and nasal congestion.
Yes, CPAP therapy can improve sleep quality. This, in turn, can enhance cognitive function and mental health.
National Center for Biotechnology Information. (2025). What is CPAP Therapy and How Does It. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK482178/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us