Knowing dangerous blood sugar levels is key for managing diabetes well. High glucose levels over 300 mg/dL can cause serious problems. These include severe dehydration and diabetic coma.
At Liv Hospital, we stress the need to manage diabetes to avoid these dangers. High blood glucose can lead to serious health issues. These include diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic syndrome (HHS), which are very dangerous if not treated quickly.
Levels above 600 mg/dL are a medical emergency that needs immediate hospital care. We urge everyone to know these critical levels. This ensures they get help fast when needed.
Key Takeaways
- Blood sugar levels above 300 mg/dL are considered dangerous.
- Levels exceeding 600 mg/dL require immediate medical attention.
- Diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic syndrome (HHS) are life-threatening complications.
- Effective diabetes management is key to avoid such complications.
- Timely medical intervention is vital for survival in extreme hyperglycemia cases.
Understanding Blood Sugar Levels: Normal vs. Dangerous
Knowing about blood sugar levels is key for managing diabetes well. Blood sugar, or glucose, gives our cells energy. But, keeping it in a normal range is vital to avoid health problems.
Normal Blood Sugar Range for Different Age Groups
Normal blood sugar levels change with age and health. For adults with diabetes, it should be between 80-130 mg/dL before eating and less than 180 mg/dL after. Kids and teens might have different targets. Always check with a doctor to find out what’s right for you.
Age Group | Normal Fasting Blood Sugar (mg/dL) | Normal Postprandial Blood Sugar (mg/dL) |
Adults | 80-130 | <180 |
Children (6-12 years) | 80-180 | <180 |
Adolescents (13-19 years) | 80-130 | <180 |
When Blood Sugar Becomes Concerning
Blood sugar levels are a worry when they’re too high (hyperglycemia) or too low (hypoglycemia). High levels can cause serious issues if not handled right. Levels over 300 mg/dL are very dangerous and need quick medical help.
The Importance of Regular Monitoring
Checking blood sugar regularly is vital for those with diabetes. It helps spot problems early, so you can act fast. Always follow your doctor’s advice on when to check your blood sugar to keep it under control.
By managing blood sugar levels well, you can lower the risk of diabetes problems. Regular checks, a healthy lifestyle, and sticking to your treatment plan are key to managing diabetes.
The Danger Zone: Blood Sugar Levels Above 300 mg/dL
Blood sugar levels above 300 mg/dL are dangerous and can cause serious health problems. It’s important to know the risks, mainly for people with diabetes.
Short-term Effects of High Blood Sugar
High blood sugar, over 300 mg/dL, is called hyperglycemia. It can cause short-term and long-term health issues. Symptoms include feeling very thirsty, needing to pee a lot, feeling tired, and blurry vision.
Immediate Risks: High blood sugar can also cause dehydration and imbalances in electrolytes. These can be very dangerous if not treated right away.
Long-term Complications of Sustained High Levels
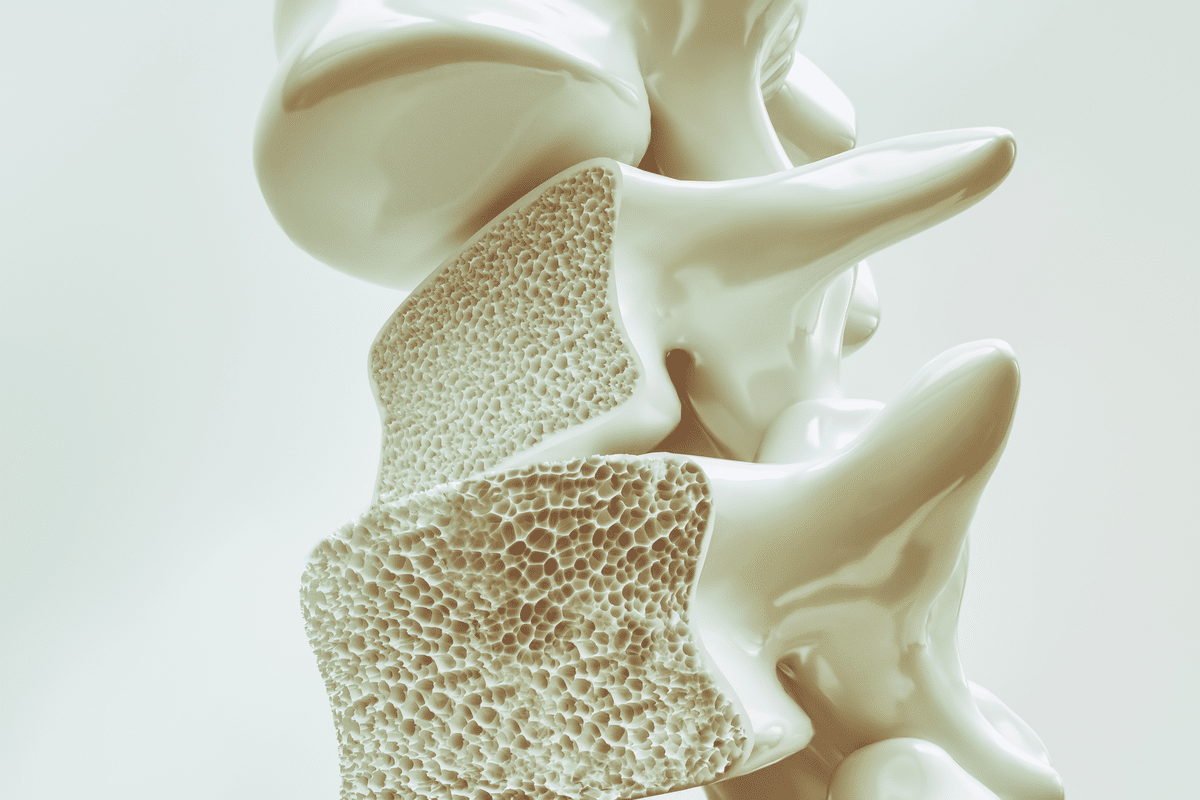
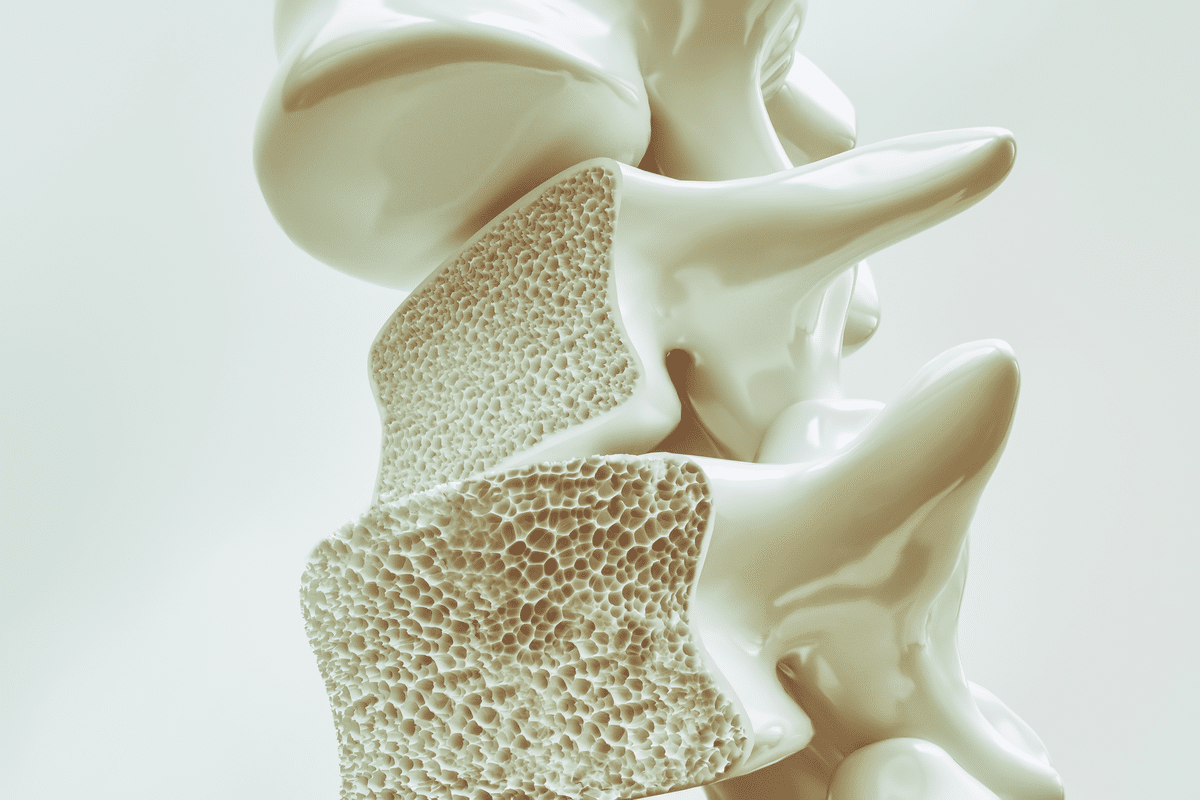
Having blood sugar over 300 mg/dL for a long time can harm your body. It can damage nerves, kidneys, and eyes. This can lead to numbness, tingling, pain, kidney failure, and vision loss.
Complication | Description | Potential Consequences |
Neuropathy | Nerve damage due to high blood sugar | Pain, numbness, tingling in extremities |
Nephropathy | Kidney damage from prolonged hyperglycemia | Kidney failure, requiring dialysis or transplant |
Retinopathy | Damage to the retina, potentially causing blindness | Vision loss, blindness if untreated |
Warning Signs to Watch For
Knowing the signs of high blood sugar is key. Look out for severe thirst, needing to pee a lot, feeling confused, and in extreme cases, losing consciousness. If you see these signs, get medical help fast.
Diabetic Ketoacidosis (DKA) and Hyperosmolar Hyperglycemic Syndrome (HHS) are serious conditions linked to high blood sugar. DKA is more common in Type 1 diabetes, while HHS is seen in Type 2. Both need quick medical care to avoid serious problems or death.
Medical Emergency: When Blood Sugar Level Reaches 600 mg/dL
When blood sugar levels hit 600 mg/dL, it’s a medical emergency. The body faces severe dehydration, coma, and death risks if not treated fast. We’ll look at the immediate effects, why hospitalization is key, and the danger of organ damage at such high levels.
Immediate Physiological Impact
A blood sugar level of 600 mg/dL leads to severe hyperglycemia. The body tries to get rid of extra glucose through urination. This causes dehydration and can lead to hyperosmolar hyperglycemic state (HHS).
Why Hospitalization Is Necessary
Hospitalization is vital when blood sugar hits 600 mg/dL. Doctors can give intravenous fluids to fight dehydration and insulin therapy to lower blood sugar. Hospital care allows for quick action against complications like seizures or coma.
Potential Organ Damage at Extreme Levels
High blood sugar levels of 600 mg/dL can cause permanent organ damage. The kidneys are at high risk due to increased workload and acute kidney injury. The heart also faces cardiac complications, making quick medical help essential to avoid lasting harm.
In summary, a blood sugar level of 600 mg/dL is a serious threat that needs immediate medical care. Knowing the risks and acting fast can save lives.
Blood Sugar Level 600: When Glucose Becomes Life-Threatening
When blood sugar levels hit 600 mg/dL, the body faces extreme stress. This can lead to severe health problems, even death. It’s vital to know how the body reacts to such high glucose levels and the dangers involved.
How the Body Responds to Extreme Hyperglycemia
Extreme hyperglycemia sets off a chain of responses to lower blood sugar. But at 600 mg/dL, these efforts fail. The body tries to get rid of excess sugar through urine, causing severe dehydration.
Doctors warn that severe hyperglycemia can lead to dehydration, electrolyte imbalance, and organ failure if not treated quickly. The body tries to make more urine, which can cause dehydration. This dehydration can lower blood volume and blood pressure. The risk of organ damage increases as the body’s compensatory mechanisms are exhausted.
Mortality Risk and Statistics
Blood sugar levels of 600 mg/dL or higher significantly increase mortality risk. Hyperosmolar Hyperglycemic Syndrome (HHS) is often linked to such high glucose levels. It has a mortality rate of 10% to 20% or more, depending on age, health, and treatment speed.
A study in a medical journal found, “The mortality rate for HHS remains high, stressing the need for early recognition and aggressive management.” The importance of timely medical intervention cannot be overstated in reducing fatal risks.
Case Studies of Severe Hyperglycemic Events
Several case studies show the severity of hyperglycemic events and the need for quick treatment. For example, a patient with a blood sugar level of 614 mg/dL improved with aggressive fluid and insulin therapy. The case report noted, “Prompt recognition and treatment of extreme hyperglycemia are key to preventing fatal outcomes.”
These studies show how patients react differently to extreme hyperglycemia and the need for tailored treatments. They also stress the importance of knowing the risks of very high blood sugar and seeking medical help right away.
Fatal Blood Sugar Levels: Understanding the Thresholds
Fatal blood sugar levels are complex and vary by person. There’s no single number that marks a fatal level. But knowing the dangers of very high levels is key to managing diabetes well.
Is There a Definitive Fatal Blood Sugar Level?
Studies show levels over 600 mg/dL are very dangerous. But how severe it is depends on many things. These include how long the blood sugar has been high and any other health issues.
Key factors influencing the severity of hyperglycemia include:
- Duration of elevated blood sugar levels
- Presence of diabetic ketoacidosis (DKA) or hyperosmolar hyperglycemic syndrome (HHS)
- Underlying health conditions, such as cardiovascular disease or kidney disease
- Age and overall health status of the individual
Individual Factors Affecting Tolerance
How well someone can handle high blood sugar varies a lot. Age, other health issues, and how long someone has had diabetes all matter. These factors help decide how well someone can handle high blood sugar.
The following table illustrates the factors affecting individual tolerance to high blood sugar levels:
Factor | Description | Impact on Tolerance |
Age | Older adults may have reduced tolerance due to decreased insulin sensitivity and other age-related factors. | Decreased tolerance |
Presence of Complications | Individuals with diabetes-related complications may have a lower tolerance to high blood sugar. | Decreased tolerance |
Duration of Diabetes | Long-standing diabetes can affect the body’s ability to manage high blood sugar levels. | Variable impact |
Documented Cases of Fatal Hyperglycemia
There are cases where very high blood sugar has been fatal. These often involve people with undiagnosed or poorly managed diabetes. Or those who have had severe hyperglycemic crises.
Learning from these cases helps healthcare providers and people with diabetes prevent such outcomes. It encourages better management of the condition.
Diabetic Ketoacidosis (DKA): A Life-Threatening Complication
DKA, or diabetic ketoacidosis, is a serious condition for people with diabetes, mainly Type 1. It shows up when there are ketones in the urine and blood sugar is very high, over 250 mg/dL. Knowing about DKA helps those with diabetes spot the signs early and get help fast.
Development of DKA in Type 1 Diabetes
In Type 1 diabetes, not having enough insulin can lead to DKA. Without enough insulin, the body starts breaking down fat for energy, making ketones. If not treated, it can turn into DKA. Early detection is key to stop it from getting worse.
Recognizing Warning Signs and Symptoms
The signs of DKA include high blood sugar, ketones in the urine, dry mouth, and frequent need to pee. It’s important to check blood sugar and ketone levels often, during sickness or when blood sugar seems high.
- High blood sugar levels
- Presence of ketones in the urine
- Dry mouth and throat
- Frequent urination
- Nausea and vomiting
- Abdominal pain
- Confusion or difficulty breathing in severe cases
Effective Treatment Protocols for DKA
Treating DKA means fixing the main problems, like insulin therapy and fluids. Prompt medical attention is essential to handle DKA well and avoid serious issues. Treatment usually includes:
- Administering intravenous fluids to rehydrate the body
- Providing insulin therapy to lower blood sugar levels and reduce ketone production
- Monitoring electrolyte levels and replacing them as necessary
- Treating any underlying conditions that may have triggered DKA
By knowing the dangers of DKA and its signs, people with diabetes can manage their condition better. This helps prevent serious problems.
Hyperosmolar Hyperglycemic Syndrome (HHS): Understanding the Risks
HHS, or Hyperosmolar Hyperglycemic Syndrome, is a serious condition that can be life-threatening. It happens when blood sugar levels get too high, often over 600 mg/dL, without ketones. This condition needs quick medical help.
Differentiating HHS from DKA
HHS and Diabetic Ketoacidosis (DKA) are different. DKA has high ketones because the body uses fat for energy. HHS does not have ketones. This makes their treatments different.
Who gets these conditions also varies. HHS often affects older people with Type 2 diabetes. DKA is more common in those with Type 1 diabetes.
Risk Factors in Type 2 Diabetes
There are several risks for HHS in Type 2 diabetes:
- Infections or acute illnesses
- Certain medications, like steroids and diuretics
- Poor diabetes management
- Undiagnosed or uncontrolled Type 2 diabetes
Knowing these risks helps prevent and treat HHS early.
Clinical Management of HHS
Managing HHS involves several important steps:
- Fluid Replacement: Rehydrating the body is the first step. It helps lower blood glucose and improves circulation.
- Insulin Therapy: Insulin helps lower blood sugar. But, it must be given carefully to avoid blood sugar drops.
- Electrolyte Replacement: It’s important to monitor and replace essential electrolytes. Their imbalance can cause serious problems.
- Treatment of Underlying Causes: Finding and treating the cause of HHS is key to preventing it from happening again.
Quick medical care and careful monitoring are key to managing HHS. This helps prevent serious problems and death.
Type 1 vs. Type 2 Diabetes: Different Risks for Dangerous Blood Sugar
Type 1 and Type 2 diabetes can both cause dangerous blood sugar levels. But, the risks and problems are different for each. Knowing these differences helps manage and prevent severe high blood sugar.
Why Type 1 Diabetics Are More Prone to DKA
Type 1 diabetes happens when the body attacks the insulin-making cells in the pancreas. People with Type 1 diabetes can’t make insulin and must take insulin shots. They are at a higher risk for Diabetic Ketoacidosis (DKA) because they can’t use insulin properly.
Several factors increase the risk of DKA in Type 1 diabetics:
- Not taking enough insulin
- Being sick or having an infection
- Not managing insulin pumps or monitors well
Common Patterns in Type 2 Diabetes Emergencies
Type 2 diabetes is about insulin resistance and not making enough insulin. While Type 2 diabetics are less likely to get DKA, they face a higher risk of Hyperosmolar Hyperglycemic Syndrome (HHS). HHS is a severe condition with very high blood sugar but little ketosis.
Here are common reasons for emergencies in Type 2 diabetes:
- Severe dehydration
- Not knowing or not controlling diabetes
- Medications that raise blood sugar
Special Considerations for Each Type
Managing Type 1 and Type 2 diabetes needs different strategies. For Type 1, it’s all about careful insulin use and checking blood sugar and ketones often. For Type 2, making healthy lifestyle choices and using medication or insulin is key to avoiding emergencies.
Important things to remember include:
- Checking blood sugar regularly
- Following medication or insulin plans
- Making healthy lifestyle choices
Causes of Severe Hyperglycemia
It’s important to know why severe hyperglycemia happens. This condition, with very high blood sugar, can cause serious health problems if not treated quickly.
Medication Issues and Insulin Deficiency
Medication and insulin problems are big reasons for severe hyperglycemia. Not taking medication as told or not having enough insulin can raise blood sugar too high. People with diabetes must take their medicine and insulin as directed.
Missing doses, taking the wrong amount, or using old medicine can mess up blood sugar control. For those on insulin, not getting enough or not changing doses can also cause high blood sugar.
Illness, Stress, and Other Triggers
Illness and stress can also cause severe hyperglycemia. Stress hormones like cortisol can make blood sugar go up. Medical issues, injuries, or stress can release these hormones, making it hard to control blood sugar.
- Infections such as pneumonia or urinary tract infections
- Surgical procedures
- Emotional stress
Knowing these triggers can help people with diabetes and their doctors manage blood sugar better during stressful times.
Undiagnosed Diabetes
Severe hyperglycemia can be the first sign of undiagnosed diabetes. Type 1 diabetes often shows up with high blood sugar because the body can’t make insulin. Type 2 diabetes can also lead to severe hyperglycemia if not caught and treated early.
It’s key to notice diabetes symptoms like being thirsty and peeing a lot, feeling tired, and blurry vision. Catching diabetes early is important for treatment.
Dietary Factors
What you eat is very important for managing blood sugar. Eating high-carb foods or sweet drinks can make blood sugar spike. People with diabetes need to know how different foods affect their blood sugar and choose wisely.
- Keep an eye on carb intake
- Stay away from sugary drinks
- Eat a balanced diet with fruits, veggies, and whole grains
Being careful with what you eat can help manage blood sugar and lower the chance of severe hyperglycemia.
Emergency Response to Critical Blood Sugar Levels
When blood sugar levels get too high, knowing what to do can save lives. We’ll show you how to react quickly and correctly in such emergencies.
When to Call 911
It’s key to know when to call for help. If someone’s blood sugar is over 300 mg/dL, or if they have symptoms like confusion or trouble breathing, call 911 right away.
First Aid Measures
While waiting for help, there are steps you can take. If the person can drink, give them water. But don’t give them insulin or medicine without a doctor’s say-so. If they’re not awake or breathing, don’t try to give them anything to eat or drink.
What to Tell Emergency Responders
When help arrives, tell them everything you know. Share the person’s diabetes details, their symptoms, any medicine they’ve taken, and their blood sugar reading. This info is important for their care.
Hospital Treatment Expectations
At the hospital, doctors will check the person’s condition and start treatment. They might give fluids to treat dehydration, insulin to lower blood sugar, and watch for any problems. Knowing what to expect can make the recovery easier.
Symptom | Action |
Blood sugar level above 300 mg/dL | Monitor closely and seek medical help if symptoms persist or worsen |
Confusion or altered mental state | Call 911 immediately |
Severe dehydration | Provide water if conscious and call 911 |
Recovery After Experiencing Dangerously High Blood Sugar
Recovering from a severe high blood sugar episode needs quick action and lasting lifestyle changes. Keeping blood sugar levels in check is key for health. When levels get too high, a detailed recovery plan is vital.
Stabilizing Blood Sugar
The first step is to bring blood sugar levels back to normal. This means adjusting medication, eating better, and being more active. It’s important to work with healthcare providers to track progress and make changes.
Keeping an eye on blood glucose levels is also critical. It helps figure out how diet, exercise, and meds affect blood sugar. This knowledge guides better choices for health.
Long-term Health Implications
High blood sugar can harm organs like the kidneys, heart, and eyes over time. Regular health checks are key to catch and prevent damage.
- Kidney damage (nephropathy)
- Heart disease and stroke
- Eye damage (retinopathy)
- Nerve damage (neuropathy)
Preventing Future Episodes
To avoid high blood sugar again, making lifestyle changes and sticking to treatment plans is essential. We suggest:
- Eating a balanced diet with healthy meals and snacks.
- Doing regular physical activity that fits your abilities.
- Following your medication schedule.
- Checking blood sugar levels often.
Follow-up Medical Care
Regular medical check-ups are vital to track recovery and tackle new problems. We recommend setting up regular visits with healthcare providers to review and adjust treatment plans.
By knowing how to recover and taking early action, people can lower the chance of future high blood sugar episodes. We’re here to support patients every step of the way.
Conclusion: Staying Vigilant About Blood Sugar Levels
Managing diabetes well means being proactive about blood sugar levels. High blood sugar can cause serious problems like diabetic ketoacidosis and hyperosmolar hyperglycemic syndrome. It’s vital to watch blood sugar closely to avoid these issues and manage diabetes well.
Regular checks, making lifestyle changes, and sticking to treatment plans are key in diabetes care. Knowing the dangers of high blood sugar and taking steps to avoid them helps people with diabetes live healthier lives. It’s a long-term effort to prevent diabetes complications.
It’s important to work closely with healthcare providers to create a diabetes management plan that fits you. This way, you can lower your risk of diabetes complications and enjoy a better quality of life. Being informed and proactive is essential for managing diabetes and keeping blood sugar levels in check.
FAQ
What is considered a dangerous blood sugar level?
Blood sugar levels over 300 mg/dL are dangerous. They can cause serious problems like diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic syndrome (HHS).
How high is too high for blood sugar?
Levels above 600 mg/dL are very dangerous. They need quick medical help to avoid organ damage and other severe issues.
What are the dangers of having a blood sugar level over 300 mg/dL?
Blood sugar over 300 mg/dL can cause dehydration, confusion, and stomach pain. It can also lead to nerve damage, kidney disease, and heart problems if not managed right.
What is the normal blood sugar range for different age groups?
Normal blood sugar levels change with age. For adults, a fasting blood glucose under 100 mg/dL is normal. Levels between 100-125 mg/dL mean prediabetes. Levels over 126 mg/dL show diabetes.
How does the body respond to extreme hyperglycemia?
Extreme hyperglycemia makes the body thirsty, urinate a lot, feel tired, and see things blurry. If not treated, it can lead to life-threatening conditions like DKA or HHS.
Is there a definitive fatal blood sugar level?
There’s no single fatal blood sugar level. But, levels over 600 mg/dL are very risky. How well someone handles high blood sugar depends on their health and diabetes complications.
What are the warning signs of Diabetic Ketoacidosis (DKA)?
DKA warning signs include high blood sugar, ketones in urine, nausea, vomiting, stomach pain, and a sweet smell on breath. It needs quick medical help to avoid serious problems.
How does Hyperosmolar Hyperglycemic Syndrome (HHS) differ from DKA?
HHS has very high blood sugar without ketones, mainly in Type 2 diabetes. DKA has ketones and acidosis, more common in Type 1 diabetes.
What are the risk factors for developing HHS in Type 2 diabetes?
Older age, infections, certain meds, and poor diabetes care increase HHS risk in Type 2 diabetes. It’s important to watch closely and act fast.
When should I call for emergency services for high blood sugar?
Call emergency services for severe symptoms like trouble breathing, chest pain, or severe stomach pain. Also, for very high blood sugar (over 600 mg/dL) with other concerning signs.
What can I expect during hospital treatment for severely high blood sugar?
Hospital treatment includes IV fluids, insulin, and blood glucose monitoring. The goal is to stabilize the patient and prevent further issues.
How can I prevent future episodes of dangerously high blood sugar?
Preventing high blood sugar means a healthy lifestyle. Eat well, exercise, follow your treatment plan, and check your blood sugar often to catch problems early.
What is the importance of follow-up medical care after experiencing high blood sugar?
After high blood sugar, follow-up care is key. It helps find the cause, adjust treatment, and watch for complications. It ensures diabetes is well-managed to avoid future episodes.
References:
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK430900/