Many people feel pelvic discomfort without knowing why. The National Institutes of Health (NIH) says about 16 out of 100 adults have constipation symptoms.
It’s important to know if constipation can cause pelvic pain and uterus discomfort. At Liv Hospital, we focus on health services with ethics and new solutions.
We look into how these issues are connected. We give you facts to understand how bowel movements might affect your pelvic health.
Addressing whether could constipation cause pelvic pain and discomfort due to pressure on adjacent organs like the uterus.
Key Takeaways
- Constipation affects a significant portion of the adult population.
- There is a possible link between constipation and pelvic pain.
- Uterus discomfort might be linked to bowel movements.
- Getting the right diagnosis is key for treatment.
- Liv Hospital offers full care for related health problems.
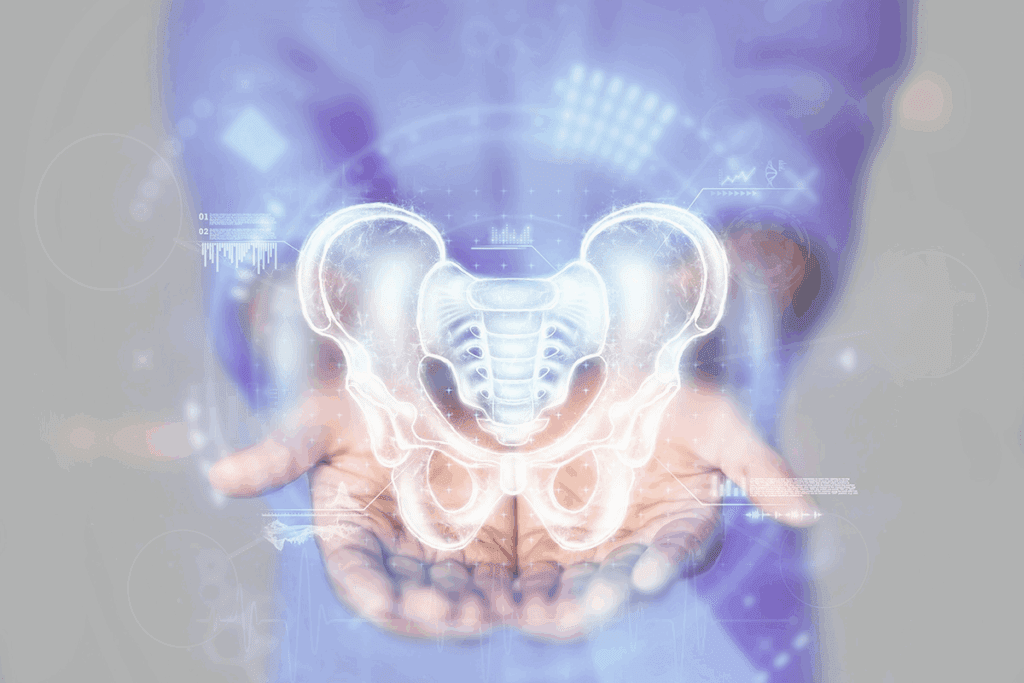
The Relationship Between Digestive and Reproductive Systems

The digestive and reproductive systems are closely linked, mainly in the pelvic area. This connection means problems in one system can affect the other, causing pain or discomfort.
Anatomical Proximity of Pelvic Organs
The pelvic cavity is home to important organs like parts of the digestive and reproductive systems. The rectum and sigmoid colon are near the uterus and ovaries in females. This close location can lead to issues affecting both systems.
For example, the rectum is right behind the uterus in females. The sigmoid colon is near the left ovary. Problems like constipation or inflammation in the digestive tract can cause pain or discomfort in other areas.
| Organ/System | Location | Potential Impact on Other Systems |
|---|---|---|
| Rectum (Digestive) | Behind the uterus | Constipation can cause uterine discomfort |
| Sigmoid Colon (Digestive) | Near the left ovary | Diverticulitis can cause left-sided pelvic pain |
| Uterus (Reproductive) | Between the bladder and rectum | Uterine conditions can cause urinary or bowel symptoms |
How the Intestines Interact with Surrounding Structures
The intestines, mainly the large intestine, are close to other pelvic structures. When they are distended or inflamed, like in constipation, they can press on or irritate nearby organs.
Shared Nerve Pathways: The nerves for the intestines are connected to those for other pelvic organs. This can cause pain or sensations in the pelvic area when there are problems like constipation.
It’s important to understand how these systems interact to treat pelvic pain and discomfort well. By knowing how the digestive and reproductive systems affect each other, doctors can provide better care.
Could Constipation Cause Pelvic Pain? The Scientific Evidence

Scientists have been studying the connection between constipation and pelvic pain. They’ve found strong evidence. It shows a clear link between these two issues.
Prevalence Statistics and Research Findings
Research shows women with chronic pelvic pain often have constipation too. It seems constipation might cause pelvic pain. This is important for diagnosing pelvic pain.
A study found many patients with chronic pelvic pain also had constipation. This shows doctors should look at stomach symptoms when treating pelvic pain.
Higher Incidence in Women with Chronic Pelvic Pain
Women with chronic pelvic pain often have constipation. Hormones, pelvic floor issues, and nerve connections play a role. It’s key to treat both conditions together.
By studying constipation and pelvic pain, researchers can find better treatments. This helps patients get better faster and with less treatment.
One-Sided Pelvic Pain from Constipation
Constipation can also cause pain on one side of the pelvis. The exact reason is not fully understood. But it might have to do with how the bowel is positioned.
It’s important to know constipation can cause one-sided pelvic pain. Doctors should look for this when treating pelvic pain. This ensures the right treatment for the cause.
Mechanisms Behind Constipation-Related Pelvic Discomfort
Constipation can cause pelvic discomfort in several ways. It affects the reproductive organs and the structures around them. Knowing how constipation leads to pelvic pain is key to solving the problem.
Physical Pressure on Reproductive Organs
Constipation puts pressure on the reproductive organs. This happens because stool builds up in the intestines. The pressure can cause pain and discomfort in the pelvic area.
Key factors contributing to physical pressure include:
- Increased stool volume in the intestines
- Distension of the bowel walls
- Anatomical proximity to reproductive organs
Pelvic Floor Muscle Strain and Dysfunction
Straining during bowel movements can strain the pelvic floor muscles. This strain can lead to muscle dysfunction. This dysfunction causes pelvic discomfort and pain.
The impact of pelvic floor muscle strain includes:
- Muscle fatigue and weakness
- Increased tension in the pelvic region
- Potential for chronic pain development
Shared Nerve Pathways Between Bowel and Pelvic Structures
The bowel and pelvic structures share nerve pathways. This can cause referred pain when constipation occurs. Irritation or inflammation in the bowel can stimulate these nerves, leading to pelvic pain.
The role of shared nerve pathways involves:
- Cross-talk between bowel and pelvic nerves
- Referred pain mechanisms
- Potential for sensitization of pelvic nerves
Why Your Uterus Hurts When Pooping: Explained
Feeling pain in your uterus when you poop can be scary and uncomfortable. It happens more often than people think. We’ll look into why this happens, focusing on the pressure and straining during bowel movements.
Pressure Dynamics During Bowel Movements
When you poop, your body goes through changes that can affect other organs. The pressure dynamics in your pelvic area are key to this discomfort. The muscles in your bowel contract and relax, putting pressure on your uterus, mainly if you have constipation or straining.
The Role of Straining in Uterine Discomfort
Straining during bowel movements often causes uterine discomfort. When you strain, you increase the pressure inside your belly, which can put more pressure on your uterus. This can lead to temporary discomfort or pain. It’s important to understand how straining affects your pelvic floor.
Distinguishing Normal Discomfort from Problematic Pain
It’s key to tell normal discomfort from pain that might mean something’s wrong. Normal discomfort is usually temporary and mild, going away after you poop. But persistent or severe pain could mean you need to see a doctor.
| Symptom | Normal Discomfort | Problematic Pain |
|---|---|---|
| Duration | Temporary | Persistent |
| Intensity | Mild | Severe |
| Triggers | Bowel movements | Various, including bowel movements |
Understanding why your uterus hurts when you poop involves looking at the complex mix of pressure and straining during bowel movements. Knowing the difference between normal discomfort and serious pain helps you figure out when to see a doctor.
Recognizing Symptoms of Constipation-Induced Pelvic Pain
It’s important to know the signs of pelvic pain caused by constipation. This helps in getting the right treatment. We must understand how constipation can lead to pelvic pain to help patients better.
Common Pain Patterns and Sensations
Constipation can lead to different types of pain in the pelvic area. Some common feelings include:
- Dull, aching pain in the lower abdomen
- Sharp, stabbing sensations during bowel movements
- Cramping pain that may radiate to the lower back
- Feeling of pressure or heaviness in the pelvic area
The pain can change in intensity and how often it happens. It often ties to how often you go to the bathroom and what your stool is like.
How Constipation Can Mimic Other Pelvic Conditions
Constipation-induced pelvic pain can be mistaken for other conditions. The pain from constipation can:
- Mimic symptoms of irritable bowel syndrome (IBS)
- Resemble menstrual cramps or endometriosis pain
- Be confused with urinary tract infections or bladder issues
It’s key to think about constipation as a possible cause of pelvic pain. This helps avoid wrong diagnoses and ensures the right treatment.
Effects on Ovaries and Surrounding Tissues
Constipation can really affect the ovaries and tissues around them. The pressure from a constipated bowel can:
| Effect | Description |
|---|---|
| Pressure on Ovaries | The constipated bowel can press against the ovaries, potentially causing discomfort or pain. |
| Increased Inflammation | Constipation can lead to inflammation in the pelvic region, affecting surrounding tissues. |
| Nerve Irritation | The pressure and inflammation can irritate nearby nerves, exacerbating pain sensations. |
Knowing these effects is key for managing constipation-induced pelvic pain well.
Diagnosing the Root Cause of Pelvic Pain
Figuring out why you have pelvic pain is key to feeling better. When you have pain in your pelvis, it’s important to get a full check-up. This helps find out what’s really causing the pain.
Medical Evaluation Process
The first step in checking for pelvic pain is talking about your symptoms. Your doctor will want to know when the pain started and what makes it better or worse. They’ll also do a physical exam to look for any problems.
They might do a pelvic exam to see if there’s anything wrong in the pelvic area. This can help find things like tumors, infections, or muscle issues.
Tests to Differentiate Constipation from Other Conditions
To find out what’s causing your pain, we might use different tests. These can include:
- Imaging studies like ultrasound or MRI to see the pelvic organs and find any problems.
- Laboratory tests, like blood work and urinalysis, to check for infections or inflammation.
- Endoscopic procedures, like colonoscopy, to look at the bowel and check for diseases.
These tests help us tell if your pain is from constipation or something else. This way, we can give you the right diagnosis.
| Diagnostic Test | Purpose |
|---|---|
| Pelvic Ultrasound | To see the reproductive organs and find any issues. |
| Colonoscopy | To check the colon and rule out diseases. |
| Laparoscopy | To look directly at the pelvic organs and find conditions like endometriosis. |
Questions Your Doctor May Ask
Your doctor will ask you lots of questions to learn more about your symptoms. They might ask:
“Can you describe the pain you’re experiencing? Is it constant or does it come and go?”
They might also ask about your bowel habits, menstrual cycle, and any recent health changes. Giving detailed answers helps your doctor find the cause of your pain.
Finding the right diagnosis is important for treatment. By knowing the cause of your pain, we can find the best way to help you.
Effective Treatment Approaches for Constipation and Pelvic Pain
To treat constipation and pelvic pain, we need a full plan. This includes diet changes, medicine, and physical therapy. By tackling the causes and symptoms, we can greatly improve life quality.
Dietary and Lifestyle Modifications
Diet is key in managing constipation and pelvic pain. Increasing fiber from fruits, veggies, and grains softens stool. Drinking enough water also helps move food through the digestive system.
Other lifestyle tips include a regular bowel routine and avoiding holding it in. Exercise also helps move things along and boosts digestive health.
Medication Options for Constipation Relief
If diet changes don’t work, medicine might be needed. Osmotic laxatives draw water into the bowel to soften stool. Stimulant laxatives help move things along by stimulating the bowel muscles.
Always talk to a doctor before starting any medication. They can help find the best option for you.
Physical Therapy for Pelvic Floor Dysfunction
Physical therapy is great for pelvic floor issues, often linked to constipation and pain. Pelvic floor physical therapy strengthens and relaxes muscles. This improves bowel function and reduces pain.
A physical therapist can create a custom exercise plan. This might include biofeedback therapy to manage symptoms and enhance pelvic health.
Home Remedies and Self-Care Strategies
There are also home remedies and self-care methods to help. Abdominal massage can stimulate bowel movements. Relaxation techniques like deep breathing or meditation can reduce stress and improve well-being.
Keeping a symptom journal is also helpful. It tracks bowel movements, pain, and other symptoms. This info helps doctors tailor treatments.
Prevention Strategies for Long-Term Pelvic Comfort
To keep your pelvis comfortable for a long time, you need to tackle many areas of your life. Healthy habits and lifestyle changes can greatly lower the chance of pelvic pain and discomfort.
Daily Habits to Maintain Bowel Regularity
Having a regular bowel routine is key to avoiding constipation, a common cause of pelvic pain. Drinking enough water and eating a diet full of fiber are important habits. Make sure to eat lots of fruits, vegetables, and whole grains.
- Eat a balanced diet with plenty of fiber
- Stay hydrated by drinking enough water
- Establish a consistent bowel routine
- Avoid processed foods that can cause constipation
Pelvic Floor Strengthening Exercises
Pelvic floor exercises, also known as Kegel exercises, are vital for keeping your pelvis comfortable. These exercises strengthen the muscles that support your pelvic organs, lowering the risk of pain and discomfort.
- Identify the correct muscles to engage during Kegel exercises
- Perform Kegels regularly, ideally 3 sets of 10 repetitions daily
- Combine Kegels with other pelvic floor exercises for complete strengthening
Stress Management Techniques
Stress can make pelvic pain and discomfort worse. Using stress management techniques like meditation, deep breathing exercises, or yoga can help reduce tension and improve pelvic comfort.
- Practice mindfulness and meditation daily
- Engage in physical activities that help reduce stress
- Consider seeking professional help for managing chronic stress
Posture and Toileting Habits
Good posture and healthy toileting habits are often overlooked but are very important for pelvic comfort. Avoid straining during bowel movements and think about using a stool or footrest to elevate your feet while on the toilet.
- Maintain good posture during daily activities
- Avoid straining during bowel movements
- Use a stool or footrest to support your feet while toileting
By adding these prevention strategies to your daily routine, you can greatly improve your long-term pelvic comfort and lower the risk of constipation-related pelvic pain.
Conclusion: When to Seek Medical Help
It’s important to understand how constipation and pelvic pain are connected. Constipation can lead to discomfort in the pelvic area. If you have persistent or severe pain, it’s time to see a doctor.
See a healthcare professional if your symptoms are unusual or get worse. They can find out why you’re in pain and help you feel better. They’ll create a plan just for you to tackle constipation and pelvic pain.
If your symptoms are impacting your daily life, don’t wait to get help. Taking action early can help you feel better and improve your overall health.
FAQ
Can constipation cause uterus pain?
Yes, constipation can cause uterus pain. The pressure from constipated bowels can strain the uterus and nearby areas. This can lead to discomfort or pain.
Why does my pelvic hurt when I poop?
Pelvic pain when you poop comes from the pressure on your pelvic organs. This includes the uterus. The pressure can cause discomfort or pain in the pelvic area.
Can constipation cause pelvic pain on one side?
Yes, constipation can cause pelvic pain on one side. The pressure from constipated bowels can be uneven. This can lead to pain or discomfort on one side of the pelvis.
How can I tell if my pelvic pain is caused by constipation?
Check for symptoms like infrequent bowel movements and hard or lumpy stools. Straining during bowel movements is also a sign. If you have these symptoms with pelvic pain, constipation might be the cause.
Can constipation cause pain in the ovaries?
Yes, constipation can cause pain in the ovaries. The pressure from constipated bowels can spread to the ovaries and surrounding tissues. This can cause discomfort or pain.
What can I do to relieve constipation-induced pelvic pain?
Try increasing fiber intake and staying hydrated. Regular exercise can also help. You might also consider medication or physical therapy for pelvic floor dysfunction.
When should I seek medical help for pelvic pain and constipation?
Seek medical help if your pelvic pain is severe or doesn’t go away. Also, if you have symptoms like heavy bleeding, fever, or trouble urinating. Your doctor can find the cause and treat it.
Can stress make constipation-related pelvic pain worse?
Yes, stress can make constipation-related pelvic pain worse. Stress can affect your bowel habits and worsen constipation. This can lead to more pelvic pain and discomfort.
Are there any exercises that can help prevent constipation and pelvic pain?
Yes, pelvic floor strengthening exercises like Kegels can help. These exercises can improve bowel habits and reduce the risk of pelvic floor dysfunction.
How can I maintain bowel regularity and prevent constipation?
To keep your bowels regular and prevent constipation, eat a high-fiber diet and stay hydrated. Regular exercise is also key. Stress management techniques like meditation or deep breathing can also help regulate your bowel habits.