As diabetes progresses, patients face severe complications needing special care. It’s key for patients, families, and doctors to know the symptoms and how to manage end-stage diabetes.
Studies show that over a quarter of people nearing the end of life have diabetes. The disease status varies widely. If diabetes is not treated, it can cause serious problems and even death from blood sugar issues.
At Liv Hospital, we understand the need for top-notch, team-based care with a focus on ethics. Our team is dedicated to making patients comfortable and cared for. We aim to manage symptoms and enhance life quality during this challenging time.
Key Takeaways
- End-stage diabetes is a critical phase with severe complications.
- Knowing the symptoms is vital for patients and caregivers.
- Diabetes can lead to death from blood sugar issues if untreated.
- Liv Hospital offers specialized care for end-stage diabetes patients.
- Our care focuses on symptom management and improving life quality.
Understanding End Stage Diabetes
It’s key for healthcare teams to grasp end-stage diabetes to better manage it. This stage is complex, with severe complications affecting the patient’s life quality.
Definition and Classification
End-stage diabetes is a serious condition with severe and life-threatening issues. It’s mainly Type 2 diabetes that’s common. Knowing the types helps in managing the disease well.
The American Diabetes Association breaks down diabetes into types like Type 1 and Type 2. Type 2 is the most common, linked to insulin issues.
Prevalence and Statistics
Type 2 diabetes is growing worldwide, posing a big health challenge. The International Diabetes Federation says diabetes will keep rising, affecting many globally.
Studies show that diabetes is common among those nearing the end of life. This underlines the need for good management. Type 2 diabetes can shorten life due to health problems, making management critical.
Is Diabetes Considered a Terminal Illness?
Diabetes is a complex condition that affects millions worldwide. It raises questions about its classification as a terminal illness. While diabetes itself is not considered a terminal illness, people with diabetes face higher mortality risks due to related conditions.
Diabetes as a Chronic vs. Terminal Condition
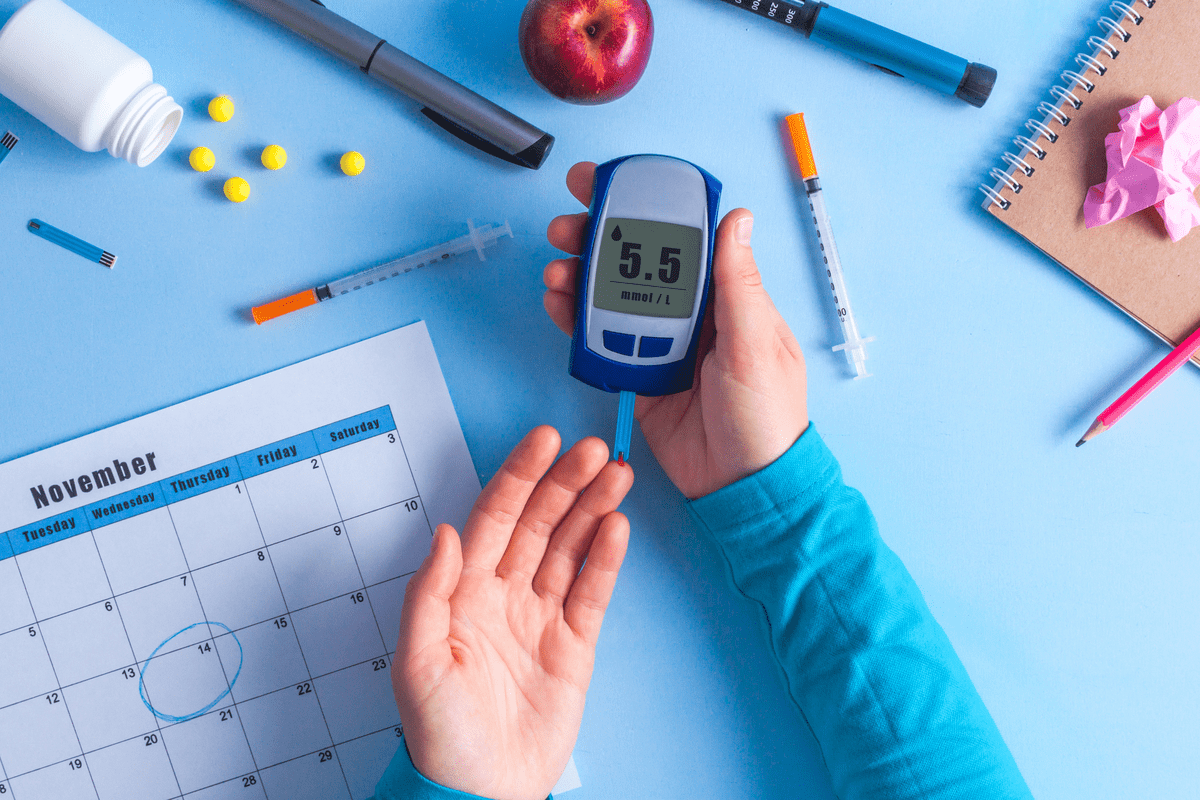
Diabetes is seen as a chronic condition, not a terminal illness. Chronic conditions are long-term health issues that need ongoing management. For diabetes, this means checking blood sugar levels, eating healthy, and possibly using medication or insulin.
But, the line between chronic and terminal gets fuzzy when looking at diabetes complications. Advanced diabetes can cause serious health problems like heart disease, kidney failure, and nerve damage. These can greatly shorten life expectancy.
Mortality Risk Factors
Several factors increase the risk of death in people with diabetes, including:
- Cardiovascular disease: The main cause of death in people with diabetes, often from heart attacks or strokes.
- Kidney failure: Diabetic nephropathy can lead to end-stage renal disease, needing dialysis or a kidney transplant.
- Infections: People with diabetes are more likely to get infections, which can be severe and life-threatening if not managed well.
It’s important for patients and healthcare providers to understand these risks. By controlling blood sugar and addressing related health issues, people with diabetes can lower their risk of complications. This improves their quality of life.
We know diabetes itself is not a terminal illness. But, its risks can greatly affect mortality. So, it’s vital to have thorough care and management to reduce these risks.
Progression to End Stage Diabetes
Understanding how diabetes progresses to its end stage is key for managing it well. The speed and way diabetes gets worse can differ a lot between people. This depends on the type of diabetes, how well it’s managed, and if there are complications.
Type 1 Diabetes Progression
Type 1 diabetes happens when the body attacks and destroys insulin-making cells. This means people need insulin to live. It can start quickly, in weeks or months, mostly in the young. But, it can take years or decades to reach the end stage, depending on how well it’s managed.
Type 1 diabetes patients face a high risk of serious complications. These include kidney damage, nerve damage, and eye problems. These issues can really affect their life quality and how long they live.
Type 2 Diabetes Progression
Type 2 diabetes is about insulin resistance and not making enough insulin. It’s often linked to lifestyle choices and can be managed with diet, exercise, and pills at first. But, many people with type 2 diabetes will need insulin as their condition worsens. It progresses slower than type 1, taking years or decades. Obesity, lack of exercise, and bad diet can make it get worse faster.
How long someone lives with diabetes depends on when they get diagnosed and treated. It also depends on how well they and their healthcare team manage it.
Timeline of Disease Advancement
The time it takes to reach end-stage diabetes varies a lot. For some, it can take 20-30 years or more after diagnosis. Good management, like keeping blood sugar in check, can slow it down. But, bad management and other health problems can speed it up.
Knowing what affects how fast diabetes gets worse is key. It helps in making better management plans and improving patient outcomes.
The Last Stages of Diabetes Before Death
Knowing the last stages of diabetes is key for good care and support. As diabetes gets worse, many complications can happen, showing the end is near. It’s important for patients and caregivers to understand these signs.
Warning Signs of Critical Decline
In the final stages, several signs show a big drop in health. Diabetic ketoacidosis (DKA) is a severe complication that can happen fast. It can lead to coma. Signs of DKA include:
- Abdominal pain
- Decreased alertness
- Difficulty breathing
- Dry mouth and skin
- Excess thirst
- Frequent urination
- Fruity-smelling breath
Another serious condition is hyperosmolar hyperglycemic state (HHS). It has blood sugar levels over 800 mg/dL. Spotting these signs early is key for quick medical help.
Common Symptoms in Final Stages
In the last stages, patients face many symptoms. These come from the disease getting worse and related problems. Symptoms include:
Symptom | Description |
Severe Fatigue | A constant feeling of tiredness and no energy |
Increased Thirst and Urination | High blood sugar causes dehydration and more trips to the bathroom |
Nausea and Vomiting | These can cause dehydration and imbalance of body salts |
A leading diabetes researcher says, “Knowing the final stages of diabetes is key for caring for patients at the end.”
This care helps manage symptoms and improve life quality for patients.
Timeframe Considerations
The time left in the last stages of diabetes varies. It depends on health issues, how well the disease is managed, and the patient’s overall health. While it’s hard to guess exactly when death will come, knowing the disease’s progression helps plan for the future.
The final stages of diabetes bring complex and severe symptoms. It’s vital to care for this stage fully, making sure the patient is comfortable and respected.
Signs That Diabetes Is Becoming Life-Threatening
As diabetes gets worse, it’s key to spot signs that it’s becoming serious. Diabetes can cause severe problems, some of which can be deadly if not treated fast.
Physical Indicators
One important sign is severe physical signs. These include:
- Severe hypoglycemia showing as shakiness and anxiety
- Advanced kidney disease, which can cause kidney failure
- Heart problems like heart failure and stroke
These signs show the body is under a lot of stress from diabetes. Quick medical help is needed to stop things from getting worse.
Cognitive and Behavioral Changes
Changes in thinking and behavior are also warning signs. People with diabetes might feel more anxious and depressed. This can make it harder to manage their diabetes. Stress hormones can raise blood sugar levels, starting a bad cycle.
Some common changes include:
- Feeling more anxious and depressed
- Being confused or disoriented
- Acting differently, like being more irritable or withdrawn
As one expert says,
“Managing diabetes is not just about keeping blood sugar in check; it’s also about keeping your mind healthy.”
When to Seek Emergency Care
It’s important to know when to get emergency care. If you or someone you know has any of these symptoms, get help right away:
- Severe hypoglycemia that doesn’t get better with treatment
- Signs of diabetic ketoacidosis (DKA), like high blood sugar, ketones in urine, and vomiting
- Heart attack or stroke symptoms, such as chest pain, trouble speaking, or numbness in face or limbs
Acting fast can save lives. Spotting these signs and getting help quickly can stop serious problems and even death.
Diabetic Ketoacidosis (DKA) as an End Stage Complication
It’s vital for people with diabetes to know about diabetic ketoacidosis (DKA). It’s a serious condition that can be deadly if not treated right. DKA happens when the body can’t use glucose for energy because it lacks insulin. This leads to the production of ketones, which are harmful acids.
Mechanism and Development
DKA can occur due to illness, skipping insulin, or taking certain meds. Without glucose, the body breaks down fat, making ketones. This can cause a buildup of ketones in the blood, leading to DKA.
Key factors that contribute to DKA include:
- Insufficient insulin dosage or omission
- Infections or illnesses that increase glucose levels
- Certain medications that affect glucose metabolism
Symptoms and Progression to Coma
DKA symptoms can appear quickly, often in 24 hours. Early signs are high blood sugar, ketones in urine, and symptoms like nausea and fruity breath. If not treated, DKA can worsen, leading to coma.
Recognizing symptoms early is key for effective treatment. If you or someone you know shows these signs, get medical help right away.
How High Can Blood Sugar Go Before Death
In DKA, blood sugar levels can soar, often over 250 mg/dL. They can go even higher, above 500 mg/dL. Such high levels can cause severe dehydration, electrolyte imbalances, and even coma or death if not treated quickly.
Immediate intravenous (IV) insulin therapy is critical in managing DKA and preventing fatal outcomes. Alongside insulin, fluid replacement and electrolyte management are vital for treating DKA.
Hyperosmolar Hyperglycemic State (HHS)
HHS is a serious condition where blood sugar levels get very high, often over 800 mg/dL.
Extreme Blood Glucose Levels
In HHS, blood sugar levels are very high, usually over 600 mg/dL. They can go up to 1000 mg/dL or more. This high sugar level is a key sign of HHS, differentiating it from other diabetic emergencies.
Key characteristics of extreme blood glucose levels in HHS include:
- Severe hyperglycemia without significant ketosis
- Blood glucose levels often exceeding 800 mg/dL
- Significant osmotic diuresis leading to dehydration
Dehydration and Cognitive Symptoms
Dehydration is a big part of HHS. It happens because the body tries to get rid of extra sugar through urine. This dehydration can cause confusion, tiredness, and even coma in severe cases.
The interplay between dehydration and cognitive impairment in HHS is complex:
- Severe dehydration can cause a decrease in blood volume, leading to reduced perfusion of vital organs.
- Cognitive symptoms can range from mild confusion to coma.
- Prompt treatment of dehydration is critical to prevent long-term cognitive damage.
Differences from DKA
Both HHS and Diabetic Ketoacidosis (DKA) are serious but different. HHS is more common in type 2 diabetes and is marked by very high blood sugar without much ketosis.
The main differences between HHS and DKA are:
Characteristic | HHS | DKA |
Typical Diabetes Type | Type 2 | Type 1 (but can occur in type 2) |
Blood Glucose Level | Very high (often >600 mg/dL) | High (usually >250 mg/dL) |
Ketosis | Absent or minimal | Present |
Knowing these differences is key to the right treatment. HHS is marked by extreme blood sugar, severe dehydration, and brain symptoms, setting it apart from DKA.
Diabetic Coma and Mortality
A diabetic coma is a serious condition that happens in people with diabetes. It’s caused by very high or very low blood sugar levels. It’s a medical emergency that needs quick help.
Types of Diabetic Coma
There are three main types of diabetic coma. Each has its own causes and symptoms:
- Diabetic Ketoacidosis (DKA) Coma: This is caused by high blood sugar and ketones in the blood.
- Hyperosmolar Hyperglycemic State (HHS) Coma: It happens when blood sugar is extremely high but doesn’t have ketones.
- Hypoglycemic Coma: This is when blood sugar drops too low.
Diabetic Coma: How Long Before Death
The time from diabetic coma to death can vary a lot. It depends on the cause, how fast and well medical care is given, and the person’s health. If treated quickly and correctly, many can get better. But, if treatment is late, it can cause brain damage or death.
It’s very important to act fast. The longer someone is in a coma, the greater the risk of death or brain damage.
Intervention Possibilities
Helping someone in a diabetic coma involves several important steps:
- Immediate Medical Attention: Calling for emergency help or getting to a hospital fast is key.
- Administration of Insulin and Fluids: For DKA and HHS, giving insulin and fluids is very important.
- Correction of Blood Sugar Levels: Slowly fixing blood sugar levels to avoid more problems.
- Monitoring and Supportive Care: Keeping an eye on vital signs and giving supportive care to handle any issues.
Knowing the causes, symptoms, and treatments for diabetic coma is key. It helps prevent death and improves chances of recovery for people with diabetes.
Advanced Renal Disease and Kidney Failure
As diabetes gets worse, a big problem that can happen is advanced renal disease. This is also known as diabetic nephropathy. It’s a major reason for sickness and death in people with diabetes.
Diabetic Nephropathy Progression
Diabetic nephropathy is a kidney disease caused by diabetes damage. It starts with damage to the tiny blood vessels in the kidneys. It goes through stages, from early signs to complete kidney failure.
Early detection and management are key to slowing down diabetic nephropathy. Keeping blood sugar and blood pressure in check is important. Doctors might also prescribe medicines to protect the kidneys.
Uraemia as a Leading Cause of Death
Uraemia is when there’s too much urea in the blood. It happens when the kidneys can’t filter waste anymore. Symptoms include nausea, tiredness, and problems with thinking clearly, making life hard.
In severe diabetes, uraemia is a top reason for death. It’s because the kidneys can’t filter blood. To manage it, treatments like dialysis or a kidney transplant are needed.
Dialysis in End Stage Diabetes
Dialysis uses a machine to clean the blood when kidneys fail. It’s a lifesaver for people with end-stage diabetes. It helps manage uraemia and other kidney problems.
Starting dialysis is a big decision. It depends on the patient’s health, how bad their kidney disease is, and their quality of life. Dialysis is a big commitment that changes your life, needing regular sessions and big lifestyle changes.
Cardiovascular Complications in End Stage Diabetes
Cardiovascular issues are a big worry for those with end-stage diabetes. People with diabetes are twice as likely to die from heart disease. High blood sugar can harm blood vessels and heart nerves. We’ll look at the heart problems that can happen in end-stage diabetes.
Myocardial Infarction Risk
Myocardial infarction, or a heart attack, is a big risk for those with end-stage diabetes. High blood pressure, high cholesterol, and damaged blood vessels are risk factors. Early detection and management of these risk factors are key to avoiding heart attacks.
Heart Failure and Stroke
Heart failure happens when the heart can’t pump enough blood. Diabetes can damage the heart and blood vessels, leading to heart failure. The risk of stroke is also higher in people with diabetes. Monitoring and controlling blood sugar levels can help reduce these risks.
Vascular Deterioration
Vascular deterioration means blood vessels get damaged over time, a common problem in diabetes. High blood sugar can damage blood vessels, reducing blood flow to organs. This can lead to heart disease. Managing blood pressure and cholesterol levels is vital to slow down this damage.
In summary, heart problems are a big threat for those with end-stage diabetes. Knowing the risks and taking steps to manage them can help. We stress the need for full care for diabetes patients to prevent and manage heart issues.
Conclusion
It’s important to know the signs of end stage diabetes before it’s too late. This knowledge helps patients and their caregivers give the best care. Managing diabetes well can prevent serious problems and improve life quality.
We’ve looked at how diabetes gets worse, its complications, and the dangers of end-stage diabetes. Spotting the signs of a serious decline is key. Knowing the difference between diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic state (HHS) is also important. This helps patients get medical help quickly.
At our institution, we aim to give top-notch healthcare and support to international patients. Effective diabetes management can lower the risk of heart problems, kidney disease, and other serious conditions.
Our goal is to give patients the tools and support they need to manage their diabetes. This way, we can improve their health outcomes and quality of life. Knowing the symptoms and risks of end stage diabetes is a big step in this journey.
FAQ:
What are the last stages of diabetes before death?
The final stages of diabetes include severe complications like diabetic ketoacidosis and hyperosmolar hyperglycemic state. Patients may also face cardiovascular disease and kidney failure. Symptoms include extreme fatigue, confusion, and severe dehydration.
Is diabetes considered a terminal illness?
Diabetes itself is not a terminal illness. But, it can lead to severe complications if not managed well. These complications can be fatal.
What are the signs that diabetes is becoming life-threatening?
Signs include severe hyperglycemia and diabetic ketoacidosis. Hyperosmolar hyperglycemic state, cardiovascular events, and kidney failure are also signs. Patients may also show confusion and altered mental status.
How high can blood sugar go before death?
Blood sugar levels over 600 mg/dL can cause life-threatening conditions. These include diabetic ketoacidosis and hyperosmolar hyperglycemic state. If untreated, these can be fatal.
What is end-stage diabetes?
End-stage diabetes is when the disease causes severe and potentially fatal complications. These include cardiovascular disease and kidney failure.
Can you die from diabetes complications?
Yes, diabetes can lead to fatal complications. These include diabetic ketoacidosis, hyperosmolar hyperglycemic state, and cardiovascular disease. Kidney failure is another risk.
What is diabetic coma, and how long before death?
Diabetic coma is a severe complication of diabetes. It happens when blood sugar levels are extremely high or low. The time from coma to death varies based on the cause and treatment.
What are the symptoms of diabetic ketoacidosis?
Symptoms include severe hyperglycemia and metabolic acidosis. Patients may also have ketosis, dehydration, nausea, vomiting, and abdominal pain. Altered mental status is common.
What is hyperosmolar hyperglycemic state (HHS)?
HHS is a severe complication of diabetes. It is characterized by extremely high blood sugar, dehydration, and cognitive symptoms. It often affects older adults with type 2 diabetes.
Can dialysis be used in end-stage diabetes?
Yes, dialysis can manage kidney failure in end-stage diabetes. The decision to start dialysis depends on the patient’s health and quality of life.
What are the cardiovascular complications in end-stage diabetes?
Cardiovascular complications include myocardial infarction, heart failure, stroke, and vascular deterioration. These can be fatal if not managed well.
How can diabetes be managed to prevent complications?
Managing diabetes involves controlling blood sugar, monitoring for complications, and adopting a healthy lifestyle. A balanced diet and regular exercise are key. Regular medical check-ups help prevent and detect complications early.
References:
Government Health Resource. Evidence-Based Medical Guidance. Retrieved from https://www.diabetesatlas.org/