If you have a herniated or bulging lumbar disc, minimally invasive lumbar discectomy might help. It’s a good choice when other treatments don’t work and you have serious nerve problems.
At Liv Hospital, we focus on you and your needs. We offer minimally invasive treatments for herniated or bulging discs. Our goal is to help you heal quickly and with less harm to your body.
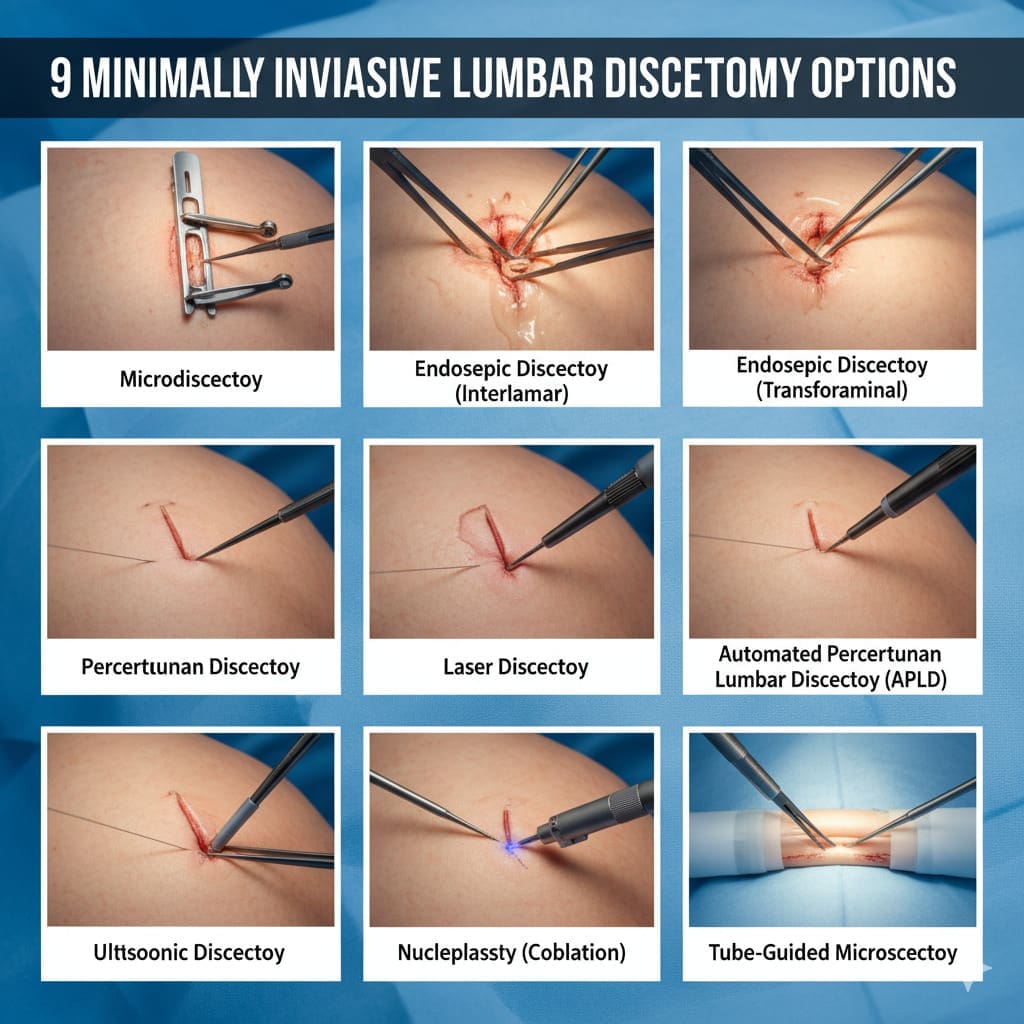
Key Takeaways
- Minimally invasive lumbar discectomy is a surgical option for herniated or bulging discs.
- Surgery is considered when conservative care fails and neurological deficits are severe.
- Liv Hospital offers patient-centered care and surgical excellence.
- Minimally invasive treatments result in less tissue damage and rapid recovery.
- Our team is dedicated to delivering personalized care for optimal outcomes.
The Evolution of Modern Lumbar Disk Surgery

Lumbar disk surgery has changed a lot over time. New technology and better understanding of spinal issues have led to these changes. Now, we see a move from old open surgeries to newer, less invasive methods.
From Open Procedures to Minimally Invasive Techniques
Old lumbar disk surgeries needed big cuts, leading to long recovery times and more risks. But, new spinal decompression surgery methods are less invasive. They cause less damage and help patients heal faster.
Today’s lumbar disk surgery uses special tools and techniques for smaller cuts. This makes recovery quicker and reduces pain and infection risks.
Common Indications for Surgical Intervention
Doctors usually suggest surgery for severe nerve problems or when other treatments fail. The main reasons for surgical disk removal are:
- Severe or getting worse nerve problems
- Not getting better with other treatments
- Big disk herniation causing nerve pain
| Indication | Description |
|---|---|
| Severe Neurological Deficits | Significant nerve symptoms like muscle weakness or cauda equina syndrome |
| Failure of Conservative Management | Not getting better with other treatments |
| Significant Disk Herniation | Disk problem causing nerve pain or big spinal pressure |
The Impact of Technology on Surgical Outcomes
New technology has made back surgery better. Tools like endoscopes, precise tests, and advanced images have made surgeries safer and more precise.
Thanks to technology, surgeons can do complex surgeries with less risk. As tech keeps getting better, so will the results of lumbar disk surgery.
Understanding Lumbar Disk Pathology

It’s important to know about lumbar disk pathology to treat lower back pain well. This term refers to problems with the disks in the lower back. These issues can cause pain, discomfort, and make it hard to move.
Anatomy of the Lumbar Spine
The lower back, or lumbar spine, has five vertebrae (L1-L5) with disks in between. These disks help absorb shock and allow for movement. The spine’s anatomy is complex, with nerves, muscles, and ligaments supporting it.
Common Problematic Levels: L3-L4, L4-L5, and L5-S1
Some parts of the lumbar spine are more likely to have disk problems. Levels L3-L4, L4-L5, and L5-S1 are often affected. These areas face a lot of stress, making them more likely to wear out or get injured.
A study on lumbar disk herniation shows that knowing which level is affected is key. This helps doctors choose the best treatment.
- L3-L4 Level: Degenerative changes can cause disk herniation or bulging here.
- L4-L5 Level: High mechanical stress makes it a common site for disk problems.
- L5-S1 Level: The junction between the lumbar spine and sacrum is also prone to disk issues.
Differentiating Between Herniated and Bulging Disks
Disk problems can show up as herniated or bulging disks. A herniated disk happens when the soft center leaks out through a tear. This can irritate nerves and cause pain. A bulging disk bulges out but doesn’t rupture, which can also irritate nerves.
It’s important to know the difference to choose the right herniated disk treatment. The right treatment depends on how severe the problem is, where it is, and the patient’s health.
Benefits of Minimally Invasive Disk Surgery Approaches
Minimally invasive disk surgery has changed the game in treating back problems. It’s now the go-to method for many lumbar disk issues. This approach offers big advantages over old-school open surgery.
Reduced Tissue Trauma and Blood Loss
One key perk of this surgery is less damage to tissues and blood loss. Smaller cuts and special tools mean less harm to nearby areas. This leads to less pain and discomfort for patients after surgery.
Faster Recovery Times and Hospital Stays
These new methods mean patients get better faster and spend less time in the hospital. With less pain, they can get back to their lives sooner than with traditional surgery.
Lower Infection Rates and Post-Operative Pain
The smaller cuts in minimally invasive surgery also mean fewer infections and less pain after surgery. This is because there’s less tissue damage. It makes recovery smoother and safer.
Long-Term Outcomes Compared to Traditional Surgery
Research shows that minimally invasive surgery can lead to better long-term results than traditional surgery. The less damage and quicker recovery help patients feel better and have fewer long-term problems.
| Outcome Measure | Minimally Invasive Surgery | Traditional Open Surgery |
|---|---|---|
| Average Recovery Time | 2-4 weeks | 6-12 weeks |
| Infection Rate | 1-2% | 3-5% |
| Blood Loss | Minimal | Moderate to Significant |
Choosing minimally invasive surgery means less damage, quicker healing, fewer infections, and better long-term results. As technology gets better, we’ll see even more improvements in patient care.
Microscopic Lumbar Discectomy
Microscopic lumbar discectomy is a top choice for treating herniated disks. It causes little damage to tissues. A microscope helps surgeons see better, making the surgery more precise.
Surgical Technique and Equipment
To do this surgery, a small cut is made in the back. A microscope lets the surgeon see the disk and nerves clearly. This way, they can safely remove the part of the disk that’s pressing on the nerve.
The tools used are a microscope, special retractors, and tiny surgical instruments. These help the surgeon remove the disk carefully. This way, they avoid hurting the nearby tissues.
Ideal Candidates and Success Rates
People with a herniated disk causing pain or nerve problems are good candidates. Most patients see big improvements after the surgery.
| Candidate Criteria | Success Rate |
|---|---|
| Patients with single-level disk herniation | 80-90% |
| Patients with significant neurological symptoms | 85-95% |
| Patients who have not responded to conservative treatment | 75-85% |
Recovery Timeline and Return to Activities
Recovery from microscopic lumbar discectomy is faster than traditional surgery. Most people can get back to normal in a few weeks.
Right after surgery, some pain is normal. But it can be managed with medicine. As the wound heals, patients can start doing more. Most are back to work and normal activities in 2-6 weeks.
It’s key to follow the doctor’s advice on care and rehab. This helps ensure the best results.
Endoscopic Lumbar Discectomy
Endoscopic lumbar discectomy is a new way to treat lumbar disk herniations. It’s a less invasive option compared to traditional surgery. This method can cause less damage to tissues, reduce pain after surgery, and help patients recover faster.
Procedure Overview and Visualization Benefits
This procedure uses a small endoscope and special tools through tiny cuts in the skin. It lets doctors see the herniated disk and nerves clearly. This makes it easier to remove the disk fragment accurately.
Key benefits of endoscopic visualization include:
- Enhanced clarity of the surgical site
- Better identification of anatomical structures
- Improved precision in disk removal
Patient Selection Criteria
Not every patient with a herniated disk is right for this surgery. Doctors look at several things before deciding. These include:
- Symptomatic disk herniation confirmed by imaging studies
- Failure of conservative management
- Specific types of disk herniations (e.g., foraminal or extraforaminal)
- Absence of significant spinal instability or severe stenosis
Comparative Advantages Over Open Techniques
Endoscopic lumbar discectomy has many benefits over traditional surgery. These include:
| Feature | Endoscopic Lumbar Discectomy | Open Lumbar Discectomy |
|---|---|---|
| Incision Size | Small (typically | Larger (typically 3-5 cm) |
| Tissue Trauma | Minimal muscle disruption | More significant muscle dissection |
| Recovery Time | Faster return to normal activities | Longer recovery period |
| Post-operative Pain | Generally less pain | More post-operative pain |
While endoscopic lumbar discectomy has many benefits, choosing the right patients is key. It’s also important to have an experienced surgeon to get the best results.
Tubular Microdiscectomy
Tubular microdiscectomy is a big step forward in spine surgery. It’s designed to fix the problems of old surgery methods. It’s a better way to treat disk problems in the lower back.
The Tubular Retractor System
The tubular retractor system is key in this surgery. It uses special tools to make a small hole in the muscle. This hole lets surgeons use special tools to fix the problem.
Key Features of the Tubular Retractor System:
- Minimal muscle disruption
- Reduced risk of nerve damage
- Enhanced visualization through the surgical microscope
Muscle-Sparing Approach and Benefits
This surgery is special because it doesn’t hurt the muscles much. This means patients feel less pain after and heal faster.
The benefits of this approach include:
- Less tissue trauma
- Reduced blood loss
- Shorter hospital stays
Post-Operative Care and Outcomes
After the surgery, taking it easy is important. Patients start moving around and seeing a physical therapist soon.
| Outcome Measure | Typical Result |
|---|---|
| Return to normal activities | 2-6 weeks |
| Pain reduction | Significant improvement within the first few weeks |
| Complication rate | Low, comparable to other minimally invasive techniques |
Tubular microdiscectomy is a great choice for back problems. It’s a modern surgery that works well and has good results.
Percutaneous Endoscopic Lumbar Discectomy (PELD)
PELD is a modern method for treating lumbar disk herniations. It uses an endoscope to see the disk and surrounding areas. This allows for the exact removal of herniated disk material.
Transforaminal vs. Interlaminar Approaches
PELD can be done in two ways: transforaminal and interlaminar. The transforaminal approach goes through the intervertebral foramen. It’s good for some herniations. The interlaminar approach goes through the interlaminar space. It offers a different angle for removing the disk.
Each method has its own benefits and when to use them. The choice depends on the herniation’s location and type, and the patient’s body.
Addressing Different Disk Herniation Types
PELD can treat many disk herniation types, including:
- Contained disk herniations
- Non-contained or extruded herniations
- Migrated disk herniations
This technique removes herniated disk material precisely. It can reduce nerve pressure and ease symptoms.
Evidence-Based Results and Limitations
Many studies show PELD’s success in treating lumbar disk herniations. It offers:
- High success rates in symptom relief
- A minimally invasive method with less tissue damage
- Quicker recovery times than traditional surgery
But, PELD has its limits. It requires surgeons to learn a lot and has specific uses. It’s not for every herniation.
PELD results can differ based on patient, surgeon skill, and care after surgery. It’s key for patients to talk to a spine surgeon. They can decide if PELD is right for them.
Automated Percutaneous Lumbar Discectomy
The automated percutaneous lumbar discectomy is a new way to treat back pain. It’s less invasive than old surgeries. This method helps fix problems with the lumbar disk.
Mechanism and Implementation
This method uses a special device to remove part of the disk. It’s done under local anesthesia, so recovery is faster. “It’s great for surgeons who want to do less harm,” say experts.
A probe is used to remove the herniated disk material. It’s less invasive than open surgery. This means smaller wounds and fewer complications.
Suitable Disk Pathologies
This method works best for contained disk herniations. It’s good for those with smaller herniations. It’s also for those who haven’t gotten better with other treatments.
Research shows it helps at levels L4-L5 and L5-S1. Choosing the right patient is key.
Success Rates and Patient Satisfaction
Success rates are between 70% to 90%. Patients are happy because it’s less painful and they recover faster.
Results can vary, but it’s a good option for many. It’s effective and quick to recover from.
Laser-Assisted Disk Surgery for Lumbar Herniation
Laser technology in disk surgery is a big step forward for treating lumbar herniation. It’s a minimally invasive method that aims to cut down on recovery time and tissue damage.
How Laser Technology is Applied
In laser-assisted disk surgery, a laser is used to vaporize or remove the herniated disk material. This is done under local anesthesia, leading to a quicker recovery than traditional surgery. The laser’s precision helps avoid damage to nearby tissues.
Our goal with laser technology is to decompress the nerve root, remove the herniated disk, and minimize tissue trauma. This method is great for those who haven’t seen results from other treatments.
Contraindications and Limitations
Laser-assisted disk surgery isn’t right for everyone. It’s not good for severe disk degeneration, significant spinal instability, or certain types of disk herniations. Also, some medical conditions make it unsuitable.
Before considering laser-assisted disk surgery, a thorough evaluation is needed. This includes checking the type and severity of the herniation and the patient’s overall health.
Current Research and Outcomes
Research on laser-assisted disk surgery shows promising results. Many studies point to high success rates in pain relief and functional improvement. But, outcomes can differ based on the technique, patient condition, and surgeon’s skill.
| Study | Success Rate | Complication Rate |
|---|---|---|
| Study A | 85% | 5% |
| Study B | 90% | 3% |
| Study C | 78% | 7% |
We keep up with the latest research and advancements in laser-assisted disk surgery. This ensures our patients get the safest and most effective treatments.
Biportal Endoscopic Discectomy
Biportal endoscopic discectomy is a big step forward in spine surgery. It’s known for better views and more room to work than old methods.
The Two-Portal Technique Explained
This method uses two small openings to reach the spine. It lets us move tools better and see clearly with the endoscope. This helps us relieve pressure on nerves.
We start by making two small cuts. Then, we put the endoscope and tools through these openings. This lets us do the surgery with great care.
Enhanced Visualization and Surgical Freedom
One big plus of this method is the better view it gives. The endoscope shows us the area clearly, helping us remove the disk material well. This helps us free up the nerve better.
Also, the two-portal way gives us more room to work. Being able to move tools through different openings helps us do the surgery more carefully. This might lead to better results.
Learning Curve and Adoption Rates
Like any new surgery, biportal endoscopic discectomy takes time to learn. Doctors need special training to get good at it. But, more doctors are starting to use it because of its benefits.
Research shows that with practice, doctors can do well with this surgery. As more doctors learn it, it will likely become more common for patients.
| Aspect | Biportal Endoscopic Discectomy | Traditional Discectomy |
|---|---|---|
| Visualization | Enhanced through endoscope | Limited by incision size |
| Surgical Freedom | Greater with two-portal technique | Restricted by single incision |
| Recovery Time | Generally faster | Variable, often longer |
Conclusion: Making an Informed Decision About Disk Surgery
Throughout this article, we’ve looked at many ways to treat herniated disks. When thinking about spine surgery, it’s key to choose what’s best for you. This choice should be based on your needs and the latest research.
We’ve talked about several minimally invasive surgery methods. Each has its own advantages and results. Knowing about these options helps patients talk to doctors about their treatment plans.
The main aim of treating herniated disks is to ease pain and boost your life quality. By looking at the info we’ve shared and talking to a doctor, you can make a smart choice. This choice is the first step towards feeling better.
What is lumbar discectomy surgery?
Lumbar discectomy surgery removes a damaged disk in the lower spine. It relieves pressure on nerves and eases pain.
What are the benefits of minimally invasive disk surgery?
Minimally invasive disk surgery has many benefits. It causes less tissue damage and blood loss. Recovery is faster, and hospital stays are shorter. It also lowers infection rates and reduces post-operative pain.
How does endoscopic lumbar discectomy compare to traditional open surgery?
Endoscopic lumbar discectomy is less invasive. It offers better visualization and less tissue damage. Recovery is also faster compared to traditional open surgery.
What is the difference between a herniated and a bulging disk?
A herniated disk has a tear, allowing the soft center to bulge out. A bulging disk doesn’t have a tear and causes less severe symptoms.
What are the most common levels of the lumbar spine affected by disk pathology?
Disk problems often occur at L3-L4, L4-L5, and L5-S1. These levels are most commonly affected.
What is microscopic lumbar discectomy, and who is it suitable for?
Microscopic lumbar discectomy uses a microscope to remove herniated disk material. It’s for patients with specific disk herniations and those who haven’t improved with conservative care.
How does percutaneous endoscopic lumbar discectomy (PELD) work?
PELD uses an endoscope to remove herniated disk material through a small incision. It’s available in two approaches: transforaminal and interlaminar.
What is the success rate of automated percutaneous lumbar discectomy?
Automated percutaneous lumbar discectomy’s success rate varies. It’s effective for certain disk problems, with reported success and patient satisfaction.
How is laser technology used in disk surgery?
Laser technology vaporizes or removes herniated disk material. It’s a minimally invasive option with specific benefits and limitations.
What is biportal endoscopic discectomy, and what are its benefits?
Biportal endoscopic discectomy uses two portals for better visualization and surgical freedom. It offers benefits in some cases but has a learning curve and varying adoption rates.
What are the key factors in deciding on a surgical approach for disk surgery?
Choosing a surgical approach depends on the patient’s needs, the disk’s type and location, and overall health. A healthcare professional’s advice is key to finding the best treatment.
What is the typical recovery time for minimally invasive lumbar discectomy?
Recovery times vary by procedure and patient. Minimally invasive techniques usually allow for quicker recovery, often within weeks.
Are there any risks or complications associated with disk surgery?
Disk surgery carries risks like infection, nerve damage, and bleeding. These are rare with modern techniques.
References
NCBI Bookshelf (StatPearls): Lumbar Microdiscectomy
PubMed Central (NCBI): Postoperative Outcome of Lumbar Microdiscectomy





