
Diabetic retinopathy is a big health problem in ophthalmology, affecting millions globally. It damages the blood vessels in the retina, the light-sensitive tissue at the back of the eye. This is a complication of diabetes.dm retinopathyTop 5 Worst Autoimmune Diseases: Fatal Risks, Symptoms & Deadliest Types
Diabetic retinopathy is a serious condition that can cause blindness if not treated. At Liv Hospital, we offer top-notch healthcare for international patients. Our team is here to help people with diabetes keep their vision and quality of life.
Key Takeaways
- Diabetic retinopathy is a complication of diabetes that affects the eyes.
- It is caused by damage to the blood vessels in the retina.
- Early detection and treatment can help prevent vision loss.
- Liv Hospital offers complete screening and preventive care for diabetic retinopathy.
- Our team of experts is dedicated to providing personalized care and guidance.
Understanding Diabetic Retinopathy
Diabetic retinopathy is a common problem for people with diabetes. It affects the blood vessels in the retina, which can lead to vision loss. We will look into what it is, how common it is, and its impact on those with diabetes.
Definition and Prevalence
Diabetic retinopathy damages the blood vessels in the retina. This damage can cause blood vessels to bleed or leak fluid. This can distort vision. In 2021, about 9.6 million Americans (26.4 percent of those with diabetes) had this condition.
Worldwide, about 22.27 percent of people with diabetes have diabetic retinopathy. It can happen to anyone with type 1 or type 2 diabetes. The risk grows with time and poor blood sugar control.
Year | Prevalence of Diabetic Retinopathy in the US | Global Prevalence |
2021 | 26.4% of Americans with diabetes | 22.27% among individuals with diabetes |
2020 | 25.6% of Americans with diabetes | 21.9% among individuals with diabetes |
Impact on Vision and Quality of Life
Diabetic retinopathy can greatly affect vision and quality of life. If not treated, it can cause severe vision loss or blindness. It not only affects daily tasks but also emotional well-being.
Early detection and management are key to preventing vision loss. Regular eye exams and good blood sugar control are important strategies.
Living with diabetic retinopathy can be tough. But with the right care and management, people can lower the risk of complications. This helps maintain their quality of life.
The Rising Prevalence of DM Retinopathy
Diabetic retinopathy is becoming more common worldwide. As more people live with diabetes, so does this eye problem. It can cause serious vision loss if not treated.
Statistics in the United States
In the U.S., diabetic retinopathy is a big health worry. Millions of Americans are dealing with it. It can happen to anyone with diabetes, including type 1, type 2, and gestational diabetes.
Regular eye checks and early treatment are key to avoiding vision loss.
Worldwide Prevalence and Projections
The world is facing a big problem with diabetic retinopathy. “The global burden of Medical Expert 103.12 million cases in 2020 to 160.50 million by 2045”. This shows we need better ways to prevent and manage it.
Understanding the risks and using proven prevention methods is vital. Regular eye exams and quick action are essential to manage diabetic retinopathy and save vision.
Types of Diabetic Retinopathy
Diabetic retinopathy is divided into two main types. Each type has its own signs and treatment needs. Knowing about these types helps doctors plan better care for patients.
Non-Proliferative Diabetic Retinopathy (NPDR)
Non-proliferative diabetic retinopathy (NPDR) is the early stage of the disease. It shows signs like microaneurysms and retinal hemorrhages. NPDR is split into mild, moderate, and severe based on how much the retina is damaged.
- Mild NPDR: Has a few microaneurysms, showing the disease’s start.
- Moderate NPDR: Shows more damage, like hemorrhages and exudates.
- Severe NPDR: Has lots of retinal hemorrhages and microaneurysms in four parts, or venous beading in two or more parts.
Proliferative Diabetic Retinopathy (PDR)
Proliferative diabetic retinopathy (PDR) is the advanced stage. It’s marked by new, fragile blood vessels in the retina. If not treated, it can cause serious vision loss.
Key characteristics of PDR include:
- Neovascularization: New blood vessels form, which can bleed easily.
- Vitreous Hemorrhage: Bleeding into the vitreous gel can cause sudden vision loss.
- Retinal Detachment: New blood vessels can cause the retina to detach, leading to severe vision loss.
Pathophysiology: How Diabetes Damages the Retina
Diabetes harms the retina in many ways. It changes blood vessels, affects chemistry, and increases stress. Too much sugar damages the tiny blood vessels that feed the retina, cutting off its blood supply.
Vascular Changes in the Retina
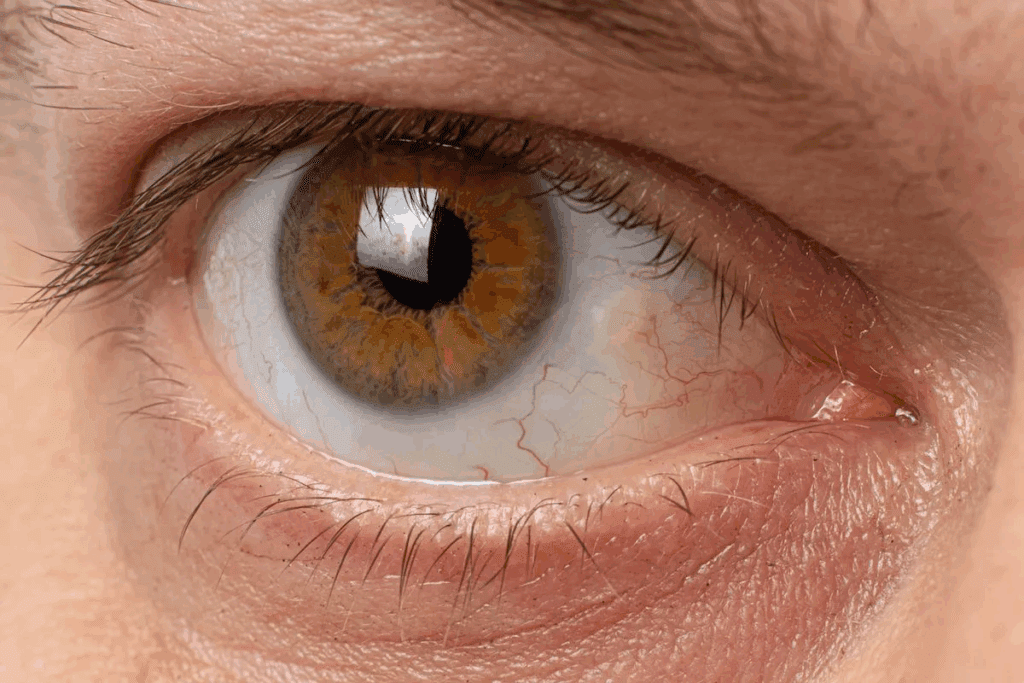
The retina’s blood vessels are greatly affected by diabetes. High blood sugar weakens these vessels, leading to problems like microaneurysms and hemorrhages. These issues can be seen during an ophthalmoscopy exam, a key tool for diabetic retinopathy diagnosis.
As diabetes worsens, the retina tries to make new, fragile blood vessels to get more oxygen. But these new vessels often leak and bleed, making things worse.
Biochemical Mechanisms
The biochemical changes in diabetic retinopathy are complex. High blood sugar leads to the buildup of harmful substances in the retina. This causes stress and inflammation. The activation of certain pathways, like the protein kinase C (PKC) pathway, also plays a big role in retinal damage.
“Hyperglycemia-induced biochemical changes lead to the activation of various cellular pathways that damage the retinal vasculature.”
Inflammation and Oxidative Stress
Inflammation and oxidative stress are major factors in diabetic retinopathy. High levels of reactive oxygen species (ROS) harm retinal cells and break the blood-retinal barrier. Inflammatory cytokines, like VEGF, are also increased, leading to more blood vessel growth and leakage.
Factor | Effect on Retina |
Advanced Glycosylation End-products (AGEs) | Accumulate in retina, contributing to oxidative stress |
Protein Kinase C (PKC) Pathway | Activated by hyperglycemia, damages retinal vasculature |
Reactive Oxygen Species (ROS) | Damages retinal cells, disrupts blood-retinal barrier |
Understanding these mechanisms is key to treating DRP eye conditions. By tackling the root causes, healthcare providers can offer better treatments. This helps manage diabetic retinopathy and prevent vision loss.
Risk Factors for Developing Diabetic Retinopathy
Knowing what can lead to diabetic retinopathy is key to preventing and managing it. This condition affects the blood vessels in the retina, which can cause vision loss if not treated.
Duration of Diabetes
The longer you have diabetes, the higher your risk of getting diabetic retinopathy. Studies show that after 20 years, almost all with type 1 diabetes and over 75% with type 2 will have some retinopathy.
Poor Glycemic Control
Keeping blood sugar levels in check is vital to avoid diabetic retinopathy. High blood sugar can harm the retina’s blood vessels, raising the risk. Tight blood sugar control can greatly lower this risk.
Hypertension and Cardiovascular Factors
Hypertension and heart health issues also affect diabetic retinopathy risk. High blood pressure can make retinal blood vessel problems worse. It’s important to manage blood pressure through lifestyle changes and, if needed, medication.
Genetic Predisposition
Genetics can also play a part in who gets diabetic retinopathy. While the exact genetic links are being studied, having a family history of diabetes increases risk.
These factors together can greatly affect your chance of getting diabetic retinopathy. Understanding and managing them is essential for prevention.
Risk Factor | Description | Impact on Diabetic Retinopathy |
Duration of Diabetes | Length of time a person has diabetes | Increased risk with longer duration |
Poor Glycemic Control | High blood sugar levels over time | Damages retinal blood vessels |
Hypertension | High blood pressure | Further strains retinal blood vessels |
Genetic Predisposition | Family history of diabetes and complications | Increases susceptibility |
By understanding these risk factors and taking proactive steps, people with diabetes can lower their risk of diabetic retinopathy. This helps protect their vision.
Complications of Untreated Diabetic Eye Disease
Diabetic retinopathy can cause serious problems if not treated. It can affect your vision and overall life quality. If not managed, it can lead to vision loss or even blindness.
Diabetic Macular Edema
Diabetic macular edema (DME) is a big problem. It happens when fluid builds up in the macula. This part of the retina is key for clear vision. Timely treatment is key to avoid losing vision forever.
Vitreous Hemorrhage
Vitreous hemorrhage is when blood leaks into the eye’s center. It can cause sudden vision loss. PDR eye treatment is vital to stop this and prevent more issues.
Retinal Detachment
Retinal detachment is a serious issue. It happens when the retina detaches from its normal spot. This can cause vision loss. If not treated, it can lead to permanent blindness. Quick medical help is needed to fix this.
Vision Loss and Blindness
The worst outcome of untreated diabetic retinopathy is vision loss or blindness. It’s a major cause of blindness in adults worldwide. Regular eye checks and early treatment can prevent this. Managing diabetes well is key to avoiding these problems.
In summary, untreated diabetic eye disease can have severe effects. It can harm your vision and life quality. It’s important to know these risks and take steps to manage diabetic retinopathy well.
Signs and Symptoms to Watch For
Diabetic retinopathy often starts without clear symptoms in its early stages. But as it gets worse, people may see changes in their vision. Knowing these signs is key to catching the problem early and avoiding serious vision loss.
Early Warning Signs
In the beginning, diabetic retinopathy might not show obvious symptoms. It could cause only slight vision issues. But there are early signs to watch for:
- Spots or floaters in vision
- Mild blurring of vision
- Fluctuations in vision quality
These signs can be easy to miss. That’s why regular eye checks are vital for catching diabetic retinopathy early.
Advanced Symptoms
As diabetic retinopathy gets worse, symptoms become more obvious and serious. Look out for:
- Significant blurring of vision
- Dark strings or floaters in the field of vision
- Difficulty perceiving colors
- Vision loss
Seek medical help right away if you notice these symptoms. Early treatment can lessen the impact on your vision.
When to Seek Medical Attention
If you’re seeing signs of diabetic retinopathy, see an eye doctor. Early treatment can greatly improve your chances of keeping your vision. Get help fast if you notice:
- Sudden changes in vision
- Severe eye pain
- Increased sensitivity to light
- Vision loss
Regular check-ups and quick action are essential for managing diabetic retinopathy. Stick to your eye exam schedule to catch and treat problems early.
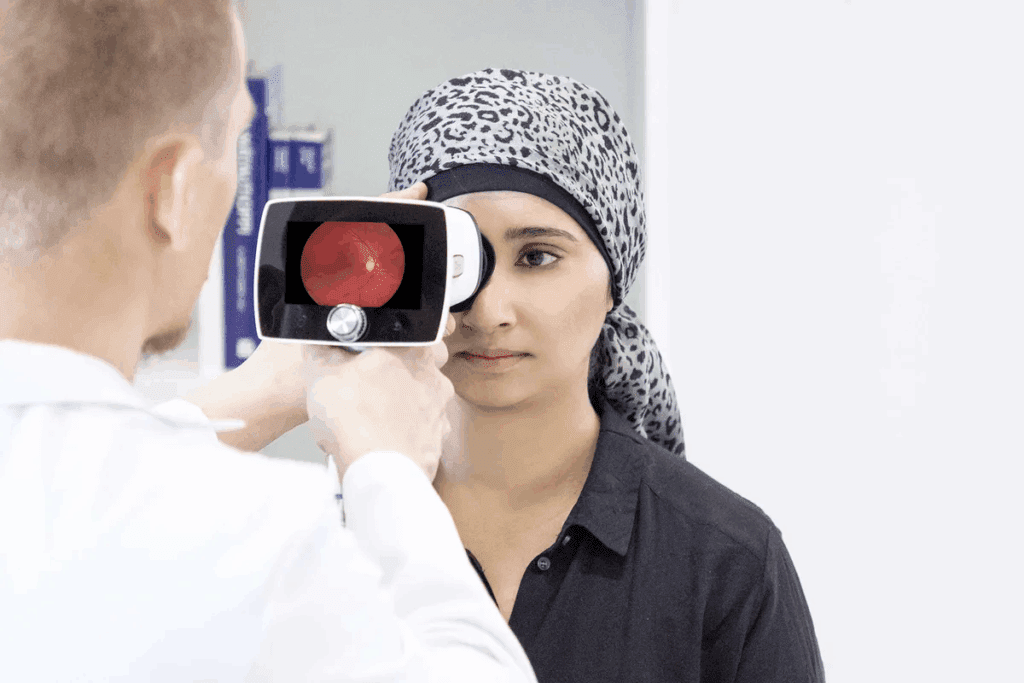
Diagnosis and Screening Protocols
Early detection is key in managing diabetic retinopathy. Regular eye exams help spot the condition early. This allows for quick action.
Comprehensive Eye Examination
A thorough eye exam is the first step in diagnosing diabetic retinopathy. It includes checking the patient’s medical history and visual acuity. A dilated eye exam lets us see the retina for damage.
During a detailed eye exam, we look for signs like microaneurysms and hemorrhages. This helps us understand how severe the condition is. It also guides our treatment choices.
Diagnostic Imaging Techniques
Advanced imaging is key in diagnosing and managing diabetic retinopathy. Optical Coherence Tomography (OCT) gives us detailed retina images. It helps spot diabetic macular edema and other issues.
Fundus Fluorescein Angiography (FFA) is also important. It shows us the retinal vasculature, helping us find leakage and non-perfusion areas. These tools are vital for tracking disease changes and treatment success.
Recommended Screening Intervals
How often to screen for diabetic retinopathy varies. It depends on the condition’s severity and the patient’s health. Generally, people with diabetes should get an eye exam yearly.
- Those with mild NPDR might need exams every 6 to 12 months.
- Patients with more severe NPDR or PDR should get checked every 3 to 6 months.
Regular screenings are essential. They help catch diabetic retinopathy early. This prevents vision loss and improves patient care.
Treatment Approaches for NPDR and PDR
Understanding how to manage diabetic retinopathy is key. There are treatments for Non-Proliferative Diabetic Retinopathy (NPDR) and Proliferative Diabetic Retinopathy (PDR). These treatments can stop the disease from getting worse.
Medical Management
Medical management is a big part of treating diabetic retinopathy. It means keeping blood sugar levels in check, managing blood pressure, and living a healthy lifestyle. Keeping blood sugar levels under control is very important to slow the disease’s progress. It’s also important to manage other health issues like high blood pressure and high cholesterol.
Laser Photocoagulation
Laser photocoagulation is a common treatment for diabetic retinopathy, mainly for PDR. It uses laser burns on the retina to reduce swelling and stop vision loss. This treatment can help prevent further vision problems by destroying bad blood vessels.
Anti-VEGF Therapy
Anti-Vascular Endothelial Growth Factor (anti-VEGF) therapy is a new treatment for diabetic retinopathy, mainly for diabetic macular edema. It involves injecting drugs that stop VEGF, a protein that helps bad blood vessels grow. This therapy can reduce swelling in the retina and improve vision.
Vitrectomy and Other Surgical Interventions
In severe cases of PDR, vitrectomy might be needed. Vitrectomy is a surgery that removes the vitreous gel and any blood in it. This surgery can help improve vision by removing blood and scar tissue that can cause retinal detachment. Other surgeries might be needed to fix retinal detachment.
Treatments for diabetic retinopathy include laser photocoagulation, anti-VEGF therapy, and vitrectomy. The right treatment depends on how severe the diabetic retinopathy is and the patient’s overall health.
Evidence-Based Prevention Strategies
To prevent diabetic retinopathy, a holistic approach is key. This includes managing blood sugar, blood pressure, and getting regular eye exams. Keeping diabetes under control can greatly lower the risk of retinopathy.
Optimal Glycemic Control
Keeping blood sugar levels in check is vital. Research shows tight control can cut the risk of retinopathy by 76% in type 1 diabetes patients.
Glycemic Targets: The American Diabetes Association suggests these blood sugar goals for most adults with diabetes: HbA1c
Blood Pressure Management
Hypertension is a big risk for diabetic retinopathy. Lowering blood pressure through lifestyle changes and, if needed, medication can help.
Blood Pressure Targets: The American Heart Association advises aiming for a blood pressure of
Lipid Management
Dyslipidemia also increases the risk of retinopathy. Controlling lipid levels through diet, exercise, and statins can prevent retinopathy from getting worse.
Lipid Parameter | Target Level |
LDL Cholesterol | |
Triglycerides | |
HDL Cholesterol | > 40 mg/dL (men), > 50 mg/dL (women) |
Regular Eye Examinations
Regular eye exams are essential for catching diabetic retinopathy early. The American Diabetes Association recommends an eye exam at diabetes diagnosis and yearly after that.
By following these prevention strategies, people with diabetes can lower their risk of retinopathy and its complications.
Conclusion
Diabetic retinopathy is a serious problem for people with diabetes. We’ve talked about what causes it, its symptoms, how it’s diagnosed, and how it’s treated. It’s important to know the risks and take steps to prevent PDR diabetes and its complications.
Keeping blood sugar levels in check, managing blood pressure, and getting regular eye exams can help. These steps can lower the risk of diabetic retinopathy. We want to stress that with the right care, diabetic retinopathy can be managed. Support is key for those dealing with this condition.
FAQ
What is diabetic retinopathy?
Diabetic retinopathy is a serious problem for people with diabetes. It damages the blood vessels in the retina. This can cause vision loss and even blindness if not treated.
What are the main types of diabetic retinopathy?
There are two main types: Non-Proliferative Diabetic Retinopathy (NPDR) and Proliferative Diabetic Retinopathy (PDR). Each type affects vision differently.
What causes diabetic retinopathy?
Diabetes damages the retina through several ways. This includes changes in blood vessels, biochemical issues, and inflammation and oxidative stress.
What are the risk factors for developing diabetic retinopathy?
Several factors increase the risk. These include how long you’ve had diabetes, poor blood sugar control, high blood pressure, and genetics.
What are the signs and symptoms of diabetic retinopathy?
Early signs might be hard to notice. But as it gets worse, you might see blurred vision, floaters, and vision loss. Seeing a doctor is key if you notice these.
How is diabetic retinopathy diagnosed?
Doctors use eye exams and imaging to diagnose it. They recommend regular screenings to catch it early.
What are the treatment options for diabetic retinopathy?
Treatments vary based on the type and severity. They include managing blood sugar, laser treatments, anti-VEGF therapy, and surgery.
How can diabetic retinopathy be prevented?
Preventing it is possible. Keep blood sugar, blood pressure, and cholesterol in check. Also, get regular eye exams.
What are the complications of untreated diabetic retinopathy?
If left untreated, it can lead to serious problems. These include diabetic macular edema, vitreous hemorrhage, retinal detachment, and vision loss.
How does diabetic retinopathy impact vision and quality of life?
It can greatly affect your vision and daily life. It can make everyday tasks harder and lower your overall well-being.
What is the prevalence of diabetic retinopathy worldwide?
It’s a growing problem worldwide. In the U.S. and globally, more people are getting it. Awareness and management are key.
How often should individuals with diabetes have their eyes screened?
People with diabetes should get their eyes checked regularly. This helps catch diabetic retinopathy early and treat it on time.
References
Government Health Resource. Evidence-Based Medical Guidance. Retrieved from
https://diabetes.org/health-wellness/eye-health/what-is-retinopathy





